Optimal timing of initiating continuous renal replacement therapy in septic shock patients with acute kidney injury
-
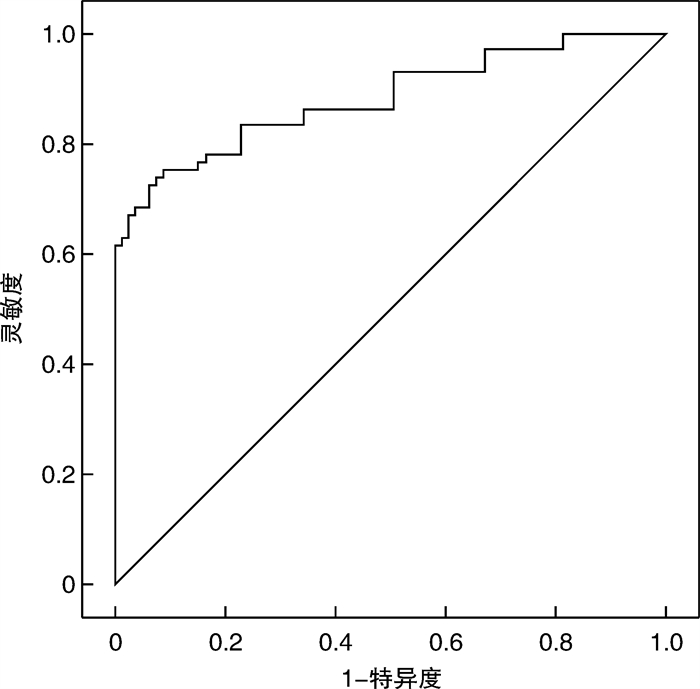
摘要: 目的 通过分析脓毒性休克致急性肾损伤(acute kidney injury,AKI)患者从AKI到持续肾脏替代治疗(continuous renal replacement therapy,CRRT)开始时间对病死率的影响,以期找到启动CRRT的最佳时间。方法 回顾性分析2020年7月—2022年6月新疆医科大学第一附属医院急诊重症监护室(EICU)脓毒性休克合并AKI接受CRRT的152例患者的临床资料。收集患者的一般资料、实验室及临床指标,将患者分为存活组和死亡组,比较2组指标之间的差异,根据病死率使用ROC曲线下面积得出脓毒性休克致AKI行CRRT的最佳间隔时间临界值,根据此临界值再将患者分为2组,分别在临界值内和临界值后开始CRRT,比较2组患者28 d总病死率。结果 152例患者中,存活组79例,死亡组73例,基线数据比较,存活组与死亡组的SOFA评分、APACHE Ⅱ评分、SAPSⅡ评分、平均动脉压(MAP)、白细胞水平、白蛋白水平、胆红素水平、血钠水平、乳酸水平、降钙素原水平比较,均差异有统计学意义;肾功能比较,AKI发生时,2组间尿素氮水平、血肌酐水平比较差异有统计学意义,进入EICU时和开始CRRT时,2组间血乳酸水平比较差异有统计学意义,从AKI到CRRT开始时间,2组间差异有统计学意义,CRRT持续时间差异无统计学意义;死亡风险分析,进入EICU时较高的乳酸水平与病死率增加有关,从AKI到CRRT开始时间越长,EICU病死率越高;根据患者病死率的ROC曲线分析显示,曲线下面积为0.883(95%CI:0.828~0.938,P < 0.001),得出AKI行CRRT的最佳间隔时间临界值为16.37 h;以16.37 h为临界点进行分组后患者的28 d生存率的对比,结果显示16.37 h之内组生存率是16.37 h之后组的7.835倍,差异统计学意义(P < 0.001)。结论 对于脓毒性休克致AKI的患者在16.37 h以内启动CRRT可提高患者的生存率。Abstract: Objective The purpose of this study is to find the time to start by analyzing the effect of the time from AKI to CRRT on mortality in patients with caused by septic shock.Methods The clinical data of 152 patients in the Emergency Intensive Care Unit(EICU) of the first affiliated Hospital of Xinjiang Medical University from July 2020 to June 2022 were analyzed retrospectively. The general data, laboratory and clinical indexes of the patients were collected, and the patients were divided into survival group and death group, the differences between the two groups were compared, and the critical value of the optimal interval time for CRRT in AKI caused by septic shock was obtained by using the AUROC curve. According to this critical value, the patients were divided into two groups: CRRT within the critical value and after the critical value, respectively. The total mortality of the two groups was compared.Results In 152 patients, there were 79 cases in the survival group and 73 cases in the death group. There were significant differences in SOFA score, APACHEII score, SAPSⅡ score, mean arterial pressure(MAP), white blood cell level, albumin level, bilirubin level, serum sodium level, lactic acid level and procalcitonin level between the survival group and the death group. In the comparison of renal function, there was a significant difference in the level of blood urea nitrogen and serum creatinine between the two groups at the occurrence of AKI. here was a significant difference in the level of blood lactic acid between the two groups at the time of entering EICU and at the beginning of CRRT. There was a statistical difference in the time from AKI to the start of CRRT between the two groups, but there was no significant difference in the duration of CRRT between the two groups. Death risk analysis showed that the higher lactate level when entering EICU was associated with increased mortality. The longer the time from AKI to CRRT, the higher the mortality rate of EICU. According to the ROC curve analysis of case fatality rate, the area under the curve is 0.883(95%CI: 0.828-0.938, P < 0.001), it is concluded that the critical value of the best interval time between AKI and CRRT is 16.37 h. Taking 16.37 h as the critical point, the 28-day mortality of the patients was compared. The results showed that the survival rate of the group within16.37 h was 7.835 times higher than that of the group after 16.37 h, and the difference was statistically significant(P < 0.001).Conclusion For patients with AKI caused by septic shock, starting CRRT within 16.37 hours can improve the survival rate of patients.
-

-
表 1 2组患者基线资料比较分析
X±S,例(%) 指标 存活组(n=79) 死亡组(n=73) t/χ2 P 年龄 65.25±4.972 66.58±3.975 -1.804 0.073 性别(男/女) 48/31 37/36 1.562 0.211 SOFA评分/分 8.95±1.033 9.49±1.122 -3.105 0.002 APACHEⅡ评分/分 21.15±1.788 23.58±2.926 -6.243 < 0.001 SAPSⅡ评分/分 39.27±4.739 45.52±3.720 -9.002 < 0.001 BMI/(kg/m2) 21.61±1.059 22.03±1.638 -1.906 0.059 感染途径 胃肠道 23(29.1) 21(28.8) 0.002 0.962 呼吸道 25(31.6) 28(38.4) 0.752 0.386 尿道 20(25.3) 17(23.3) 0.085 0.771 中枢神经系统 12(15.2) 10(13.7) 0.068 0.794 皮肤软组织感染 12(15.2) 10(13.7) 0.068 0.794 其他途径 8(10.1) 10(13.7) 0.464 0.496 基础疾病 冠心病 14(17.7) 17(23.3) 0.724 0.395 高血压 11(13.9) 14(19.2) 0.762 0.383 糖尿病 11(13.9) 10(13.7) 0.002 0.968 COPD 12(15.2) 10(13.7) 0.068 0.794 肿瘤 8(10.1) 10(13.7) 0.464 0.496 血液病 6(7.6) 10(13.7) 1.501 0.221 临床参数 心率/(次/min) 110.43±9.482 111.90±4.673 -1.200 0.232 MAP/mmHg 74.14±7.293 70.45±6.968 3.186 0.002 白细胞/(×109/L) 12.354±3.100 13.800±3.430 -2.729 0.007 血小板/(×109/L) 96.06±8.205 94.02±7.187 1.629 0.105 白蛋白/(g/dL) 2.474±0.573 2.293±0.486 2.082 0.039 胆红素/(mg/dL) 1.056±0.580 1.227±0.360 -2.369 0.019 尿素氮/(mg/dL) 44.913±11.775 46.027±8.570 -0.663 0.509 肌酐/(mg/dL) 2.513±0.965 2.624±0.991 -0.698 0.486 钠/(mmol/L) 138.619±4.595 140.333±5.041 -2.193 0.030 钾/(mmol/L) 4.318±0.492 4.445±0.471 -1.628 0.106 乳酸/(mmol/L) 3.478±0.933 8.397±1.473 -24.785 < 0.001 尿排出量/(mL/d) 595.70±201.205 614.16±218.499 -0.543 0.588 降钙素原/(ng/mL) 15.955±7.848 18.361±6.246 -2.080 0.039 CRP/(mg/L) 192.502±57.125 186.507±66.241 0.599 0.550 注:COPD为慢性阻塞性肺病,CRP为C反应蛋白。 表 2 2组患者在AKI不同阶段生化指标比较
X±S 指标 存活组(n=79) 死亡组(n=73) t P AKI发生时 尿素氮/(mg/dL) 50.783±19.177 57.821±24.743 -1.981 0.049 肌酐/(mg/dL) 1.890±0.825 2.240±0.723 -2.787 0.006 钾/(mmol/L) 4.224±0.456 4.359±0.429 -1.875 0.063 乳酸/(mmol/L) 5.228±2.295 5.120±1.641 0.331 0.741 尿排出量/(mL/d) 1 372.010±522.700 1 345.010±408.013 0.353 0.725 进入EICU时 尿素氮/(mg/dL) 44.913±11.775 46.027±8.570 -0.663 0.509 肌酐/(mg/dL) 2.513±0.965 2.624±0.991 -0.698 0.486 钾/(mmol/L) 4.318±0.492 4.445±0.471 -1.628 0.106 乳酸/(mmol/L) 3.478±0.933 8.397±1.473 -24.785 < 0.001 尿排出量/(mL/d) 595.700±201.205 614.160±218.499 -0.543 0.588 开始CRRT时 乳酸/(mmol/L) 5.201±2.077 6.489±2.262 -3.658 < 0.001 NGAL/(ng/mL) 1 022.190±530.187 941.810±361.060 1.084 0.280 胱抑素C/(mg/L) 2.997±1.052 3.151±1.067 -0.895 0.372 从AKI到CRRT时间/h 13.240±2.589 21.450±5.849 -11.329 < 0.001 CRRT持续时间/h 74.590±15.150 69.800±17.454 1.810 0.072 注:NGAL为中性粒细胞明胶酶相关脂蛋白。 表 3 EICU脓毒性休克致AKI CRRT患者死亡风险Cox回归分析
指标 β SE Wald P HR 95%CI AKI发生时 尿素氮 0.002 0.006 0.104 0.747 1.002 0.991~1.013 肌酐 -0.028 0.178 0.025 0.874 0.972 0.686~1.378 进入EICU时 SOFA评分 -0.047 0.119 0.157 0.692 0.954 0.756~1.204 APACHEⅡ评分 0.094 0.048 3.786 0.052 1.099 0.999~1.208 SAPSⅡ评分 0.026 0.036 0.511 0.475 1.026 0.956~1.101 MAP -0.014 0.018 0.627 0.428 0.986 0.951~1.021 白细胞 0.060 0.042 2.073 0.150 1.062 0.978~1.154 蛋白质 -0.411 0.280 2.159 0.142 0.663 0.383~1.147 胆红素 -0.411 0.364 1.272 0.259 0.663 0.325~1.354 钠 -0.021 0.025 0.686 0.407 0.980 0.933~1.029 乳酸 0.401 0.076 28.075 < 0.001 1.493 1.287~1.732 降钙素原 0.001 0.018 0.006 0.939 1.001 0.966~1.038 开始CRRT时 乳酸 0.121 0.065 3.473 0.062 1.128 0.994~1.281 从AKI到CRRT时间 0.093 0.025 13.660 < 0.001 1.097 1.044~1.152 CRRT持续时间 -0.012 0.007 2.790 0.095 0.988 0.974~1.002 -
[1] 李敏, 杨虎勇, 杨伟伟, 等. 基于MIMIC-Ⅲ数据库的重症患者急性肾损伤预后预测模型的建立[J]. 中华危重病急救医学, 2021, 33(8): 949-954. doi: 10.3760/cma.j.cn121430-20200924-00649
[2] Manrique-Caballero CL, Del Rio-Pertuz G, Gomez H. sepsis-associated acute kidney injury[J]. Crit Care Clin, 2021, 37(2): 279-301. doi: 10.1016/j.ccc.2020.11.010
[3] 张宇慧, 杨莉. 脓毒症相关急性肾损伤[J]. 临床内科杂志, 2022, 39(6): 372-376. doi: 10.3969/j.issn.1001-9057.2022.06.004
[4] Zhi DY, Lin J, Zhuang HZ, et al. Acute kidney injury in critically ill patients with sepsis: clinical characteristics and outcomes[J]. J Investig Surg, 2019, 32(8): 689-696. doi: 10.1080/08941939.2018.1453891
[5] Agapito Fonseca J, Gameiro J, Marques F, et al. Timing of initiation of renal replacement therapy in sepsis-associated acute kidney injury[J]. J Clin Med, 2020, 9(5): 1413. doi: 10.3390/jcm9051413
[6] Zha JJ, Li C, Cheng GX, et al. The efficacy of renal replacement therapy strategies for septic-acute kidney injury: a PRISMA-compliant network meta-analysis[J]. Medicine(Baltimore), 2019, 98(16): e15257.
[7] Shankar-Hari M, Phillips GS, Levy ML, et al. Developing a new definition and assessing new clinical criteria for septic shock: for the third international consensus definitions for sepsis and septic shock(sepsis-3)[J]. JAMA, 2016, 315(8): 775-787. doi: 10.1001/jama.2016.0289
[8] Khwaja A. KDIGO clinical practice guidelines for acute kidney injury[J]. Nephron Clin Pract, 2012, 120(4): c179-184. doi: 10.1159/000339789
[9] 付优, 何聪, 白银箱, 等. 肾阻力指数联合中心静脉压预测脓毒性休克患者发生急性肾损伤的价值[J]. 中华危重病急救医学, 2020, 32(4): 473-477. doi: 10.3760/cma.j.cn121430-20191014-00062
[10] Kuwabara S, Goggins E, Okusa MD. The pathophysiology of sepsis-associated AKI[J]. Clin J Am Soc Nephrol, 2022, 17(7): 1050-1069. doi: 10.2215/CJN.00850122
[11] Fan LL, Wang YJ, Nan CJ, et al. Neutrophil-lymphocyte ratio is associated with all-cause mortality among critically ill patients with acute kidney injury[J]. Clin Chim Acta, 2019, 490: 207-213. doi: 10.1016/j.cca.2018.09.014
[12] 李玉婷, 李洪祥, 郭健杏, 等. 平均动脉压对脓毒性休克患者发生急性肾损伤的影响[J]. 中华急诊医学杂志, 2019, 28(9): 1088-1092. doi: 10.3760/cma.j.issn.1671-0282.2019.09.006
[13] 何力, 苏连久, 张婧, 等. ICU内脓毒性休克急性肾损伤患者肾功能恢复的影响因素分析[J]. 中华危重病急救医学, 2020, 32(2): 199-203. doi: 10.3760/cma.j.cn121430-20200106-00037
[14] 王伟, 冯庆国, 杨万杰, 等. 不同液体复苏策略对脓毒性休克AKI患者肾功能的影响[J]. 中华危重病急救医学, 2020, 32(9): 1080-1084. doi: 10.3760/cma.j.cn121430-20200717-00529
[15] He FF, Wang YM, Chen YY, et al. sepsis-induced AKI: from pathogenesis to therapeutic approaches[J]. Front Pharmacol, 2022, 13: 981578. doi: 10.3389/fphar.2022.981578
[16] 关明镜, 张凌. 脓毒症相关急性肾损伤的体外血液净化治疗进展[J]. 中华医学杂志, 2023, 103(8): 617-622. doi: 10.3760/cma.j.cn112137-20220921-01988
[17] An N, Chen RM, Bai YF, et al. Efficacy and prognosis of continuous renal replacement therapy at different times in the treatment of patients with sepsis-induced acute kidney injury[J]. Am J Transl Res, 2021, 13(6): 7124-7131.
[18] Yoon BR, Leem AY, Park MS, et al. Optimal timing of initiating continuous renal replacement therapy in septic shock patients with acute kidney injury[J]. Sci Rep, 2019, 9(1): 11981. doi: 10.1038/s41598-019-48418-4
-




 下载:
下载:
