Prognostic value of serum cystatin C combined with left ventricular outflow tract velocity time integral in elderly patients with heart failure
-
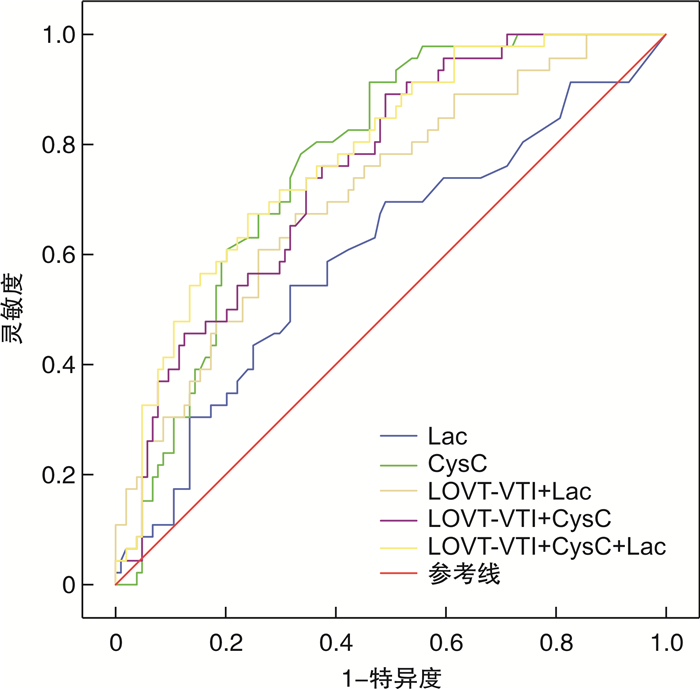
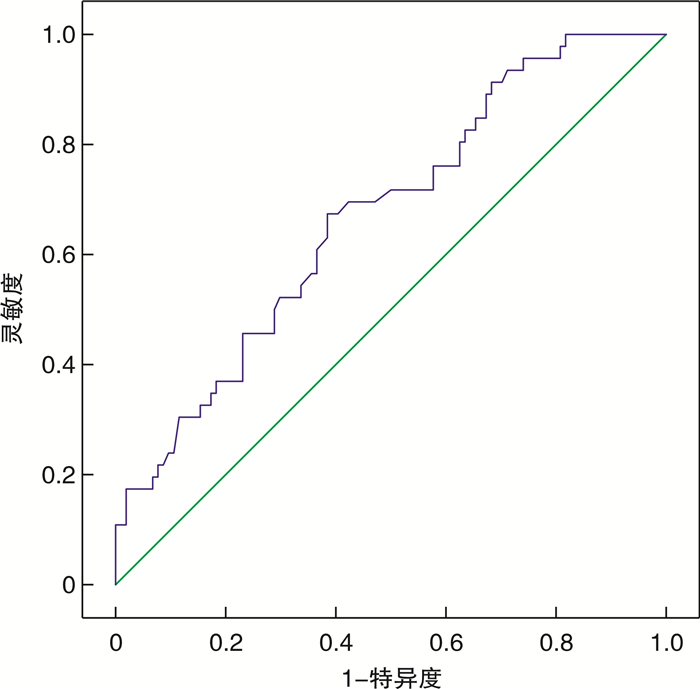
摘要: 目的 探讨高龄心衰患者死亡危险因素并评估血清胱抑素C(Cys C)及左室流出道速度时间积分(LOVT-VTI)对预后的预测价值。方法 纳入2019年10月—2022年10月在连云港市第二人民医院老年科住院的150例90周岁以上的心力衰竭患者,根据左心室射血分数(LVEF)是否大于50%分为2组,并根据28 d随访结果分为生存组和死亡组,ROC曲线评估Cys C及LOVT-VTI对高龄心衰患者预后的预测价值。结果 150例高龄心衰患者死亡46例,病死率为30.67%。死亡组的PCT、Cys C、Lac和NT-ProBNP均显著高于生存组(P < 0.05),而e-GFR、LVEF、TAPSE、MAPSE和LOVT-VTI均显著低于生存组(P < 0.05)。LVEF < 50%组的病死率高于LVEF≥50%组(45.50% vs 15.10%,P < 0.05)。LVEF < 50%组的NT-ProBNP、Cys C显著高于LVEF≥50%组(P < 0.05),而e-GFR、TAPSE、MAPSE和LOVT-VTI均显著低于LVEF≥50%组(P < 0.05)。高龄心衰患者NT-ProBNP与LVEF、TAPSE、MAPSE及LOVT-VTI呈负相关,r分别为-0.588,-0.263,-0.270,-0.243(均P < 0.05);而NT-ProBNP与Cys C呈正相关(r=0.583,P < 0.05)。logistic回归显示:Lac、LOVT-VTI和Cys C是高龄心衰患者死亡的主要危险因素(P < 0.05)。LOVT-VTI对高龄心衰患者预后预测的AUC为0.670(95%CI:0.597~0.761),截点为20.075;LOVT-VTI +Cys C+Lac三者联合时AUC为0.780(95%CI:0.704~0.857)。根据LOVT-VTI是否大于截点20.075分为2组,存活28 d为上限,Kaplan-Meier曲线生存分析:2组28 d存活率差异有统计学意义(84.62% vs. 52.78%,χ2=18.389,P < 0.001)。结论 对于高龄心衰患者,血清Cys C及LOVT-VTI可用于预测预后,指导心衰患者分类救治。
-
关键词:
- 高龄 /
- 心力衰竭 /
- 血清胱抑素C /
- 左室流出道速度时间积分 /
- 预后
Abstract: Objective To investigate the risk factors of death in elderly patients with heart failure, and to evaluate the prognostic value of serum cystatin C and left ventricular outflow tract velocity time integral(LOVT-VTI).Methods A total of 150 patients over 90 years old with heart failure admitted to the Geriatric Department of the Second People's Hospital of Lianyungang from October 2019 to October 2022 were included. They were divided into two groups according to whether the LVEF was more than 50%. According to the clinical outcome of 28-day follow-up, they were divided into survival group and death group.Results The mortality rate of 150 elderly patients with heart failure was 30.67%. Lac, PCT, NT-ProBNP and Cys C in death group were significantly higher than those in survival group(P < 0.05), while e-GFR, LVEF, TAPSE, MAPSE and LOVT-VTI in death group were significantly lower than those in survival group(P < 0.05). The mortality rate in LVEF < 50% group was higher than that in LVEF≥50% group(45.50% vs. 15.10%, P < 0.05). The levels of NT-ProBNP and Cys C in LVEF < 50% group were significantly higher than those in LVEF≥50% group(P < 0.05), while the levels of e-GFR, TAPSE, MAPSE and LOVT-VTI in LVEF < 50% group were significantly lower than those in LVEF≥50% group(P < 0.05). There was a negative correlation between NT-ProBNP and LVEF, TAPSE, MAPSE and LOVT-VTI in elderly patients with heart failure, and the correlation coefficients r were-0.588, -0.263, -0.270, -0.243 respectively (all P < 0.05). There was a positive correlation between NT-ProBNP and Cys C(r=0.583, P < 0.05). Logistic regression: Lac, LOVT-VTI and Cys C were the main risk factors for death in elderly patients with heart failure(P < 0.05). The AUC under ROC curve of LOVT-VTI for predicting poor prognosis in elderly patients with heart failure was 0.670(95%CI: 0.597-0.761), and the cut-off point was 20.075. The AUC of LOVT-VTI+Cys C+Lac was 0.780(95%CI: 0.704-0.857). According to whether the LOVT-VTI was greater than the cut-off point of 20.075, patients were divided into two groups, with 28-day survival as the upper limit, Kaplan-Meier curve survival analysis showed that the 28-day survival rate of the two groups was significantly different(84.62% vs. 52.78%, χ2=18.389, P < 0.001).Conclusion For elderly patients with heart failure, Cys C and LOVT-VTI can be used to predict the prognosis and guide the classified treatment of patients with heart failure. -

-
表 1 生存组与死亡组比较
例(%),X±S,M(P25,P75) 项目 生存组(n=104) 死亡组(n=46) t/Z/χ2 P 男性 63(60.60) 33(71.70) 1.725 0.203 年龄/岁 91.86±2.01 92.48±2.58 -1.557 0.122 高血压 49(47.10) 26(56.50) 1.129 0.376 糖尿病 37(35.60) 22(47.80) 2.005 0.204 房颤 31(29.80) 26(56.50) 9.661 0.003 冠心病 57(54.80) 30(65.20) 1.419 0.283 脑梗死 46(44.20) 18(39.10) 0.339 0.595 慢性肺疾病 41(39.40) 24(52.20) 2.112 0.157 白细胞计数/(×109·L-1) 12.17±7.81 14.51±13.11 -1.353 0.178 血小板计数/(×109·L-1) 162.00(114.00,214.00) 126.50(104.75,187.50) -1.235 0.217 IL-6/(pg·mL-1) 114.00(38.23,598.63) 193.70(58.94,1481.25) 1.810 0.070 PCT/(ng·mL-1) 1.36(0.50,2.97) 4.47(1.47,10.06) 4.327 < 0.001 CK-MB/(ng·mL-1) 3.09(2.08,5.97) 4.82(1.92,7.66) 0.948 0.343 cTnT/(ng·L-1) 50.30(21.25,147.95) 112.35(43.20,267.08) 2.688 0.007 NT-ProBNP/(pg·mL-1) 804.50(376.00,3613.75) 3461.50(1181.00,11820.25) 4.028 < 0.001 AST/(IU·L-1) 60.50(25.00,180.00) 60.50(25.00,257.75) 0.114 0.909 ALB/(g·L-1) 30.39±4.15 29.18±4.24 1.629 0.106 e-GFR/(mL·min-1) 87.14(64.32,105.82) 70.18(41.56,91.40) -2.152 0.031 Cys C/(mg·L-1) 1.15(0.85,1.72) 2.15(1.47,2.30) 5.266 < 0.001 Lac/(mmol·L-1) 1.90(1.30,3.58) 2.70(1.48,6.15) 1.982 0.047 LVEF/% 54.81±7.39 48.69±8.84 4.402 < 0.001 TAPSE/mm 2.30±0.60 1.80±0.56 4.699 < 0.001 MAPSE/mm 1.67±0.52 1.28±0.41 4.508 < 0.001 LOVT-VTI/cm 21.69±4.83 18.48±4.07 3.938 < 0.001 注:IL-6,白细胞介素-6;PCT,降钙素原;CK-MB,肌酸激酶同工酶;cTnT,肌钙蛋白T;NT-ProBNP,B型N末端钠尿肽前体;AST,天冬氨酸转氨酶;ALB,血清白蛋白;e-GFR,估算肾小球滤过率;Lac,乳酸。 表 2 不同类型心衰组间比较
例(%),X±S,M(P25,P75) 项目 LVEF≥50%(n=73) LVEF < 50%(n=77) t/Z/χ P 死亡(例%) 11(15.10) 35(45.50) 16.273 < 0.001 男性 50(68.50) 46(59.70) 1.246 0.309 年龄/岁 91.88±1.86 92.21±2.60 0.893 0.373 高血压 36(49.30) 39(50.60) 0.027 0.998 糖尿病 30(41.10) 29(37.70) 0.185 0.739 房颤 25(34.20) 32(41.60) 0.850 0.402 冠心病 42(57.50) 45(58.40) 0.013 1.000 脑梗死 30(41.40) 34(44.20) 0.143 0.743 慢性肺疾病 35(47.90) 30(39.00) 1.232 0.323 白细胞计数/(×109·L-1) 13.03±10.56 12.76±9.00 0.171 0.865 血小板计数/(×109·L-1) 140.00(112.00,209.00) 138.00(111.00,192.50) -0.626 0.531 IL-6/(pg·mL-1) 118.00(44.21,501.45) 181.10(45.27,973.50) 0.957 0.339 PCT/(ng·mL-1) 1.56(0.53,3.83) 1.96(0.91,7.06) 1.638 0.102 CK-MB/(ng·mL-1) 2.93(2.11,5.40) 4.48(2.00,9.63) 1.585 0.113 cTnT/(ng·L-1) 32.50(15.25,62.50) 124.40(63.15,238.10) 6.105 < 0.001 NT-ProBNP/(pg·mL-1) 549.00(228.00,925.50) 4086.00(1860.00,13964.00) 7.626 < 0.001 AST/(IU·L-1) 91.00(29.50,318.50) 40.00(24.00,132.00) -2.247 0.025 ALB/(g·L-1) 30.24±4.07 29.81±4.34 0.616 0.539 e-GFR/(mL·min-1) 87.55(67.89,107.52) 74.23(42.07,100.89) -2.213 0.027 Cys C/(mg·L-1) 1.15(0.86,1.73) 1.71(1.15,3.05) 4.018 < 0.001 Lac/(mmol·L-1) 2.20(1.40,4.85) 2.20(1.35,3.75) -0.581 0.561 TAPSE/mm 2.35±0.65 1.95±0.56 4.121 < 0.001 MAPSE/mm 1.70±0.58 1.41±0.41 3.510 0.001 LOVT-VTI/cm 22.41±5.00 19.09±4.08 4.473 < 0.001 表 3 NT-ProBNP与各指标的相关性分析
项目 r P LVEF -0.588 < 0.001 TAPSE -0.263 0.001 MAPSE -0.270 0.001 LOVT-VTI -0.243 0.003 Cys C 0.583 < 0.001 cTnT 0.558 < 0.001 表 4 变量赋值表
变量 赋值情况 预后(Y) 存活=0,死亡=1 LVEF < 50%(X1) 否=0,是=1 房颤(X2) 否=0,是=1 PCT≥1.80 ng/mL(X3) 否=0,是=1 cTnT≥63.35 ng/L(X4) 否=0,是=1 NT-ProBNP≥1315.00 pg/mL(X5) 否=0,是=1 e-GFR < 82.55 mL/min(X6) 否=0,是=1 Cys C≥1.43 mg/L(X7) 否=0,是=1 Lac≥2.20 mmol/L(X8) 否=0,是=1 TAPSE < 2.05 mm(X9) 否=0,是=1 MAPSE < 1.52 mm(X10) 否=0,是=1 LOVT-VTI < 20.40 cm(X11) 否=0,是=1 表 5 logistic回归分析高龄心衰患者死亡发生的危险因素
自变量 β SE Waldχ2 P OR 95%CI 房颤 0.821 0.518 2.513 0.113 2.273 0.824~6.276 PCT 0.880 0.556 2.507 0.113 2.410 0.811~7.163 cTnT -0.942 0.625 2.274 0.132 0.390 0.115~1.326 NT-ProBNP 0.511 0.658 0.604 0.437 1.667 0.459~6.056 LVEF 0.827 0.687 1.449 0.229 2.286 0.595~8.783 Lac 1.335 0.575 5.384 0.020 3.801 1.230~11.740 TAPSE 0.945 0.575 2.703 0.100 2.572 0.834~7.930 MAPSE 0.966 0.525 3.387 0.066 2.628 0.939~7.356 LOVT-VTI 1.353 0.576 5.524 0.019 3.869 1.252~11.958 e-GFR -0.290 0.593 0.239 0.625 0.748 0.234~2.394 Cys C 2.379 0.635 14.019 < 0.001 10.796 3.107~37.510 表 6 各指标预测预后的曲线下面积
指标 曲线下面积AUC 标准误 P 95%CI LOVT-VTI 0.670 0.046 0.001 0.579~0.761 Cys C 0.770 0.038 < 0.001 0.696~0.845 Lac 0.602 0.051 0.048 0.501~0.702 LOVT-VTI+Lac 0.713 0.045 < 0.001 0.625~0.801 LOVT-VTI+Cys C 0.754 0.040 < 0.001 0.675~0.832 LOVT-VTI+Cys C+Lac 0.780 0.039 < 0.001 0.704~0.857 -
[1] Ahmad OB, Boschi-Pinto C, Lopez AD, et al. Age standardization of rates: a new WHO standard[J]. Geneva: World Health Organization, 2001, 9(10): 1-14.
[2] 中国医疗保健国际交流促进会急诊医学分会, 中华医学会急诊医学分会, 中国医师协会急诊医师分会, 等. 急性心力衰竭中国急诊管理指南(2022)[J]. 临床急诊杂志, 2022, 23(8): 519-547. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2022.08.001
[3] Hao G, Wang X, Chen Z, et al. Prevalence of heart failure and left ventricular dysfunction in China: the China Hypertension Survey, 2012-2015[J]. Eur J Heart Fail, 2019, 21(11): 1329-1337. doi: 10.1002/ejhf.1629
[4] Wu JH, Liang YM, Chen R, et al. Association of plasma cystatin C with all-cause and cause-specific mortality among middle-aged and elderly individuals: a prospective community-based cohort study[J]. Sci Rep, 2022, 12(1): 22265. doi: 10.1038/s41598-022-24722-4
[5] 黄志平, 崔巍, 乔雪峰, 等. 慢性心力衰竭患者血清胱抑素C水平变化的meta分析[J]. 临床心血管病杂志, 2018, 34(9): 909-913. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB201809016.htm
[6] West M, Kirby A, Stewart RA, et al. Circulating cystatin C is an independent risk marker for cardiovascular outcomes, development of renal impairment, and long-term mortality in patients with stable coronary heart disease: the LIPID study[J]. J Am Heart Assoc, 2022, 11(5): e020745. doi: 10.1161/JAHA.121.020745
[7] Omote K, Nagai T, Iwano H, et al. Left ventricular outflow tract velocity time integral in hospitalized heart failure with preserved ejection fraction[J]. ESC Heart Fail, 2020, 7(1): 167-175.
[8] Spathoulas K, Tsolaki V, Zakynthinos GE, et al. The role of left ventricular ejection fraction and left ventricular outflow tract velocity-time integral in assessing cardiovascular impairment in septic shock[J]. J Pers Med, 2022, 12(11): 1786. doi: 10.3390/jpm12111786
[9] Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology(ESC)Developed with the special contribution of the Heart Failure Association(HFA)of the ESC[J]. Eur Heart J, 2016, 37(27): 2129-2200. doi: 10.1093/eurheartj/ehw128
[10] McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure[J]. Eur Heart J, 2021, 42(36): 3599-3726. doi: 10.1093/eurheartj/ehab368
[11] 张班, 刘晓刚, 胡立群. 射血分数保留的心力衰竭研究新展[J]. 临床心血管病杂志, 2022, 38(4): 271-275. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202204004.htm
[12] Nazir T, Nuffati M. Cardiac amyloidosis-an underdiagnosed cause of heart failure in the elderly[J]. J Saudi Heart Assoc, 2020, 32(1): 98-102.
[13] Adamo L, Rocha-Resende C, Prabhu SD, et al. Reappraising the role of inflammation in heart failure[J]. Nat Rev Cardiol, 2020, 17(5): 269-285. doi: 10.1038/s41569-019-0315-x
[14] 王传合, 李志超, 佟菲, 等. 血清胱抑素C联合N末端B型利钠肽原对心力衰竭患者院内死亡的评估价值[J]. 中国循环杂志, 2020, 35(10): 990-995. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGXH202010009.htm
[15] Matana A, Zaninović Jurjević T, Matana Kaštelan Z. Can the difference in serum concentration of urea and cystatin C be used in diagnosis and prognosis of heart failure?[J]. Med Hypotheses, 2014, 83(3): 401-403.
[16] Rothenbacher D, Rehm M, Iacoviello L, et al. Contribution of cystatin C-and creatinine-based definitions of chronic kidney disease to cardiovascular risk assessment in 20 population-based and 3 disease cohorts: the BiomarCaRE project[J]. BMC Med, 2020, 18(1): 300.
[17] Wang CH, Han S, Tong F, et al. Predictive value of the serum cystatin C/prealbumin ratio in combination with NT-proBNP levels for long-term prognosis in chronic heart failure patients: a retrospective cohort study[J]. Front Cardiovasc Med, 2021, 8: 684919.
[18] Zivlas C, Triposkiadis F, Psarras S, et al. Left atrial volume index in patients with heart failure and severely impaired left ventricular systolic function: the role of established echocardiographic parameters, circulating cystatin C and galectin-3[J]. Ther Adv Cardiovasc Dis, 2017, 11(11): 283-295.
[19] Zhai SS, Wang H, Sun LC, et al. Artificial intelligence(AI)versus expert: a comparison of left ventricular outflow tract velocity time integral(LVOT-VTI) assessment between ICU doctors and an AI tool[J]. J Appl Clin Med Phys, 2022, 23(8): e13724.
[20] Tan C, Rubenson D, Srivastava A, et al. Left ventricular outflow tract velocity time integral outperforms ejection fraction and Doppler-derived cardiac output for predicting outcomes in a select advanced heart failure cohort[J]. Cardiovasc Ultrasound, 2017, 15(1): 18.
[21] Blanco P. Rationale for using the velocity-time integral and the minute distance for assessing the stroke volume and cardiac output in point-of-care settings[J]. Ultrasound J, 2020, 12(1): 1-9.
-




 下载:
下载: