Risk factors of noninvasive ventilator treatment failure in patients with severe acute pancreatitis complicated with acute respiratory distress syndrome
-
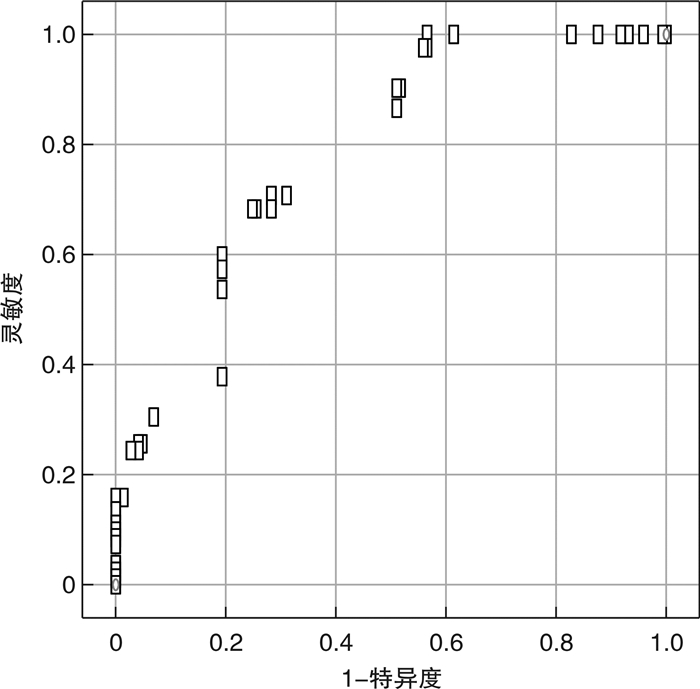
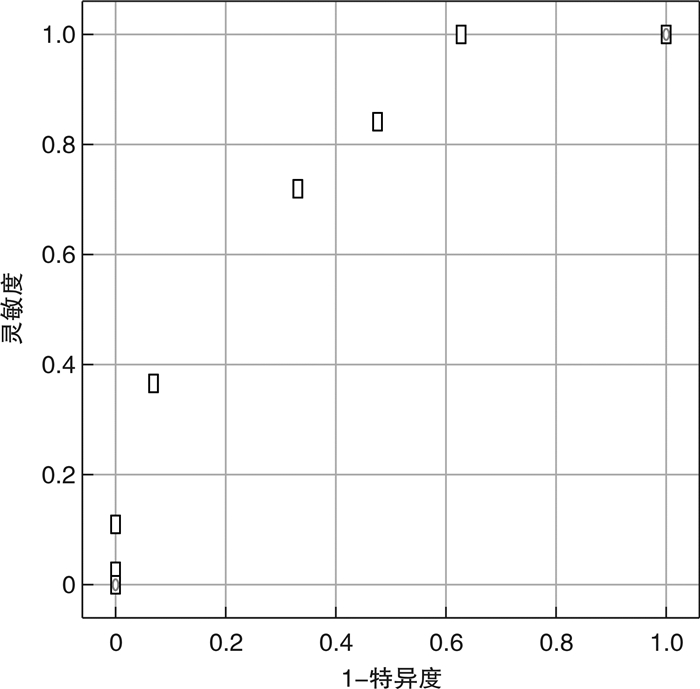
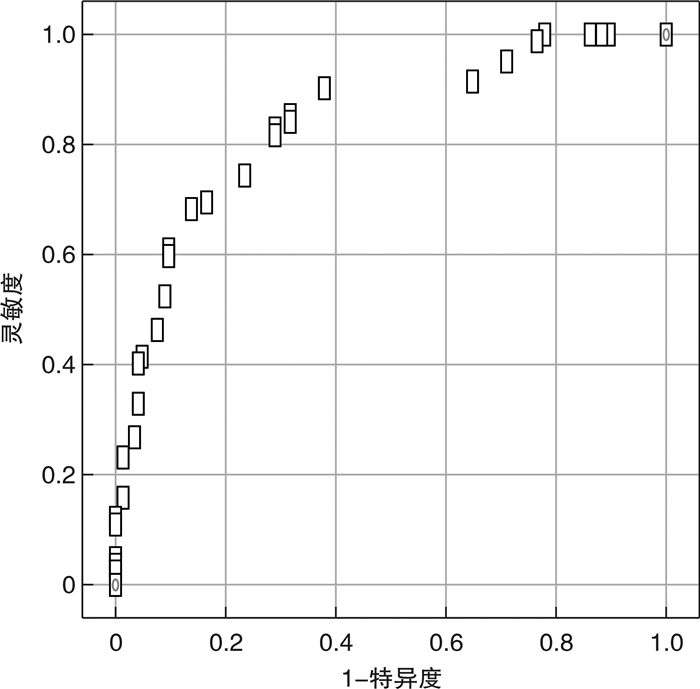
摘要: 目的 探讨无创呼吸机对重症急性胰腺炎(SAP)合并急性呼吸窘迫综合征(ARDS)患者治疗失败的危险因素,分析危险因素对治疗失败的预测价值。方法 收集2019年5月—2022年5月急诊重症病房(EICU)收治的SAP合并ARDS患者的临床资料,根据无创呼吸机治疗成功与否将患者分为失败组与成功组。收集患者基本资料、实验室检查结果、并发症发生人数及危重症相关评分等。采用二元logistic回归分析SAP合并ARDS患者无创呼吸机治疗失败的独立危险因素,运用受试者工作特征曲线(ROC)分析危险因素的预测价值。结果 符合纳入标准病例227例,失败组82例,成功组145例。失败组性别比、年龄、BMI、基础疾病史、吸烟史、大量饮酒史、胆道疾病、高甘油三酯血症、轻中重度ARDS、ICU住院天数、心率、MAP、PaO2/FiO2、HbA1c、Alb、RANSON评分、BISAP评分、镇静药物、血液净化与成功组比较,差异无统计学意义(P>0.05);2组间APACHE Ⅱ评分、CTSI评分、CRP、IL-6、腹腔压力、ACS比较,差异有统计学意义(P < 0.05);二元logistic回归分析显示,CTSI评分、IL-6、腹腔压力是治疗失败的独立危险因素(P < 0.05)。ROC曲线结果显示,IL-6较另外2个因素更具有预测价值,其截断值为110.45 pg/mL,灵敏度和特异度分别为0.683、0.317,曲线下面积(AUC)为0.841(95%CI:0.787~0.895,P=0.001)。结论 CTSI评分、IL-6、腹腔压力是SAP合并ARDS患者无创呼吸机治疗失败的独立危险因素,其中IL-6对于SAP合并ARDS患者无创呼吸机治疗失败具有预测价值。Abstract: Objective To investigate the risk factors of non-invasive ventilator for treatment failure in patients with severe acute pancreatitis(SAP) complicated with acute respiratory distress syndrome(ARDS), and to analyze the predictive value of risk factors for treatment failure.Methods Clinical data of SAP patients with ARDS admitted to the emergency intensive care unit(EICU) from May 2019 to May 2022 were collected, and the patients were divided into failure group and success group according to the success of non-invasive ventilator treatment. Basic data such as gender, age, body mass index(BMI), smoking history, heavy alcohol consumption history, heart rate, and mean arterial pressure(MAP) were collected. Imaging and laboratory results were collected, such as the number of biliary diseases and hypertriglyceridemia, glycosylated hemoglobin(HbA1c), C-reactive protein(CRP), interleukin 6(IL-6), serum albumin(Alb), and oxygenation index(PaO2/FiO2). The number of patients with intraperitoneal compartment syndrome(ACS) and moderate to severe ARDS were collected. The number of patients receiving sedative drugs and blood purification treatment was collected. Patients'critical illness scores, such as APACHE Ⅱ score, RANSON score, BISAP score and CTSI score, were collected. The independent risk factors of non-invasive ventilator treatment failure in SAP patients with ARDS were analyzed by binary logistic regression, and the predictive value of risk factors was analyzed by receiver operating characteristic curve(ROC).Results A total of 227 cases met the inclusion criteria, including 82 cases in the failed group and 145 cases in the successful group. By comparison, There was no significant difference in sex ratio, age, BMI, smoking history, heavy drinking history, biliary tract disease, hypertriglyceridemia, moderate to severe ARDS, length of ICU stay, heart rate, MAP, PaO2/FiO2, HbA1c, Alb, RANSON score, BISAP score, sedate drugs, blood purification between the failed group and the successful group(P>0.05); APACHE Ⅱ score, CTSI score, CRP, IL-6, abdominal pressure and ACS were statistically significant between the two groups(P < 0.05). Binary logistic regression analysis showed that CTSI score, IL-6 and abdominal pressure were independent risk factors for treatment failure(P < 0.05). ROC curve results showed that IL-6 had higher predictive value than the other two factors, with a cut-off value of 110.45, sensitivity and specificity of 0.683 and 0.317, respectively, and area under the curve(AUC) of 0.841(95%CI: 0.77-0.895, P=0.002).Conclusion CTSI score, IL-6 and abdominal pressure are independent risk factors for non-invasive ventilator treatment failure in SAP patients with ARDS, and IL-6 has a guiding role in predicting non-invasive ventilator treatment failure in SAP patients with ARDS.
-

-
表 1 2组患者基本资料比较
例(%),X±S 参数 失败组(n=82) 成功组(n=145) t/ χ2 P 性别(男/女) 35/47 64/81 0.045 0.832 平均年龄/岁 45.45±16.04 41.85±14.33 1.742 0.083 BMI/(kg/m2) 26.25±6.46 24.90±5.29 2.513 0.063 吸烟史 31(37.8) 51(35.2) 0.157 0.692 大量饮酒史a) 43(52.4) 95(65.5) 3.759 0.053 胆道疾病 49(59.8) 84(57.9) 0.072 0.789 基础疾病史 循环系统 21(25.6) 39(26.9) 0.711 0.782 神经系统 5(6.1) 10(6.9) 7.254 0.654 呼吸系统 9(11.0) 14(9.7) 3.144 0.371 高甘油三酯血症 55(67.1) 82(56.6) 2.423 0.120 ARDS分级 轻度 25(30.5) 52(35.9) 0.675 0.467 中度 34(41.5) 52(35.9) 0.698 0.477 重度 23(28.0) 41(28.3) 0.001 1.000 ICU住院天数/d 8.09±3.21 7.61±2.59 1.206 0.229 心率/(次·min-1) 71.98±14.48 70.52±13.75 0.753 0.452 MAP/mmHg 68.90±9.68 64.28±15.94 1.919 0.056 PaO2/FiO2 290.12±24.97 289.86±25.08 0.075 0.940 HbA1c/% 12.21±3.99 11.40±3.94 1.491 0.137 Alb/(g·L-1) 34.25±5.32 35.08±5.66 1.084 0.280 CRP/(mg·L-1) 142.30±50.49 120.40±44.37 3.396 < 0.050 IL-6/(pg·mL-1) 115.91±30.04 68.69±35.76 10.107 < 0.001 APACHE Ⅱ评分 12.45±4.48 11.02±4.60 2.265 < 0.050 RANSON评分 2.84±1.16 2.88±1.30 0.238 0.812 BISAP评分 2.38±1.24 2.19±1.14 1.177 0.241 CTSI评分 4.06±1.26 2.50±1.40 8.361 < 0.050 腹腔压力/mmHg 19.13±6.83 12.85±4.51 8.327 < 0.050 ACS 21(25.6) 7(4.8) 5.213 < 0.050 镇静药物 25(30.5) 57(39.3) 1.767 0.184 血液净化 52(63.4) 81(55.9) 1.231 0.267 注:a)每日饮酒≥150 mL。 表 2 无创呼吸机治疗失败因素logistic回归分析
因素 系数 SE Wald P OR 95%CI 腹腔压力 0.213 0.057 13.809 0.007 0.808 0.723~0.904 CRP 0.009 0.005 3.054 0.081 0.991 0.982~1.001 IL-6 0.044 0.008 30.860 0.001 0.957 0.942~0.972 APACHE Ⅱ评分 0.076 0.048 2.495 0.114 0.926 0.843~1.019 CTSI评分 0.887 0.184 23.139 < 0.001 0.412 0.287~0.591 ACS 0.575 0.660 0.759 0.384 1.777 0.487~6.484 -
[1] 曹锋, 李非, 赵玉沛. 《中国急性胰腺炎诊治指南(2021)》解读[J]. 中国实用外科杂志, 2021, 41(7): 758-761. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGWK202107007.htm
[2] 许利明, 郑悦亮. 基于指南强化重症急性胰腺炎的综合评估和治疗[J]. 临床急诊杂志, 2022, 23(12): 837-841. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2022.12.007
[3] Gragossian A, Siuba MT. Acute respiratory distress syndrome[J]. Emerg Med Clin North Am, 2022, 40(3): 459-472. doi: 10.1016/j.emc.2022.05.002
[4] Meyer NJ, Gattinoni L, Calfee CS. Acute respiratory distress syndrome[J]. Lancet, 2021, 398(10300): 622-637. doi: 10.1016/S0140-6736(21)00439-6
[5] Bellani G, Laffey JG, Pham T, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries[J]. JAMA, 2016, 315(8): 788-800. doi: 10.1001/jama.2016.0291
[6] Kwizera A, Kateete DP, Ssenyonga R, et al. Acute respiratory distress syndrome in an African intensive care unit setting: a prospective study of prevalence and outcomes[J]. Ann Am Thorac Soc, 2022, 19(4): 691-694. doi: 10.1513/AnnalsATS.202103-270RL
[7] 崔文华, 张仕娟, 刘宏波. 血浆胶体渗透压在早期创伤失血性休克合并ARDS中的诊断和预后价值[J]. 临床急诊杂志, 2022, 23(1): 30-33. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2022.01.007
[8] Saguil A, Fargo MV. Acute respiratory distress syndrome: diagnosis and management[J]. Am Fam Physician, 2020, 101(12): 730-738.
[9] Szatmary P, Grammatikopoulos T, Cai WH, et al. Acute pancreatitis: diagnosis and treatment[J]. Drugs, 2022, 82(12): 1251-1276. doi: 10.1007/s40265-022-01766-4
[10] Gosangi B, Rubinowitz AN, Irugu D, et al. COVID-19 ARDS: a review of imaging features and overview of mechanical ventilation and its complications[J]. Emerg Radiol, 2022, 29(1): 23-34. doi: 10.1007/s10140-021-01976-5
[11] Janssens JP, Cantero C, Pasquina P, et al. Monitoring long term noninvasive ventilation: benefits, caveats and perspectives[J]. Front Med(Lausanne), 2022, 9: 874523.
[12] Zhao XL, Huang W, Li J, et al. Noninvasive positive-pressure ventilation in acute respiratory distress syndrome in patients with acute pancreatitis: a retrospective cohort study[J]. Pancreas, 2016, 45(1): 58-63. doi: 10.1097/MPA.0000000000000377
[13] Copelin E, Widmer J. Management of severe acute pancreatitis in 2019[J]. Transl Gastroenterol Hepatol, 2022, 7: 16. doi: 10.21037/tgh-2020-08
[14] Wald R, Beaubien-Souligny W, Chanchlani R, et al. Delivering optimal renal replacement therapy to critically ill patients with acute kidney injury[J]. Intensive Care Med, 2022, 48(10): 1368-1381. doi: 10.1007/s00134-022-06851-6
[15] Ward J, Noel C. Basic modes of mechanical ventilation[J]. Emerg Med Clin North Am, 2022, 40(3): 473-488. doi: 10.1016/j.emc.2022.05.003
[16] Song LJ, Xiao B. Medical imaging for pancreatic diseases: Prediction of severe acute pancreatitis complicated with acute respiratory distress syndrome[J]. World J Gastroenterol, 2022, 28(44): 6206-6212. doi: 10.3748/wjg.v28.i44.6206
[17] Mancilla Asencio C, Berger Fleiszig Z. Intra-abdominal hypertension: a systemic complication of severe acute pancreatitis[J]. Medicina(Kaunas), 2022, 58(6): 785.
[18] De Waele JJ. Intra-abdominal hypertension and abdominal compartment syndrome[J]. Curr Opin Crit Care, 2022, 28(6): 695-701.
[19] 郑智, 曲元旭, 丁乙轩, 等. 急性胰腺炎发病机制的研究进展[J]. 中华肝胆外科杂志, 2021, 27(2): 152-155. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGWK201207034.htm
[20] Rose-John S. Local and systemic effects of interleukin-6(IL-6) in inflammation and cancer[J]. FEBS Lett, 2022, 596(5): 557-566.
[21] 杨宁, 王瑞峰, 耿金婷, 等. 白细胞和乳酸脱氢酶对急性胰腺炎MCTSI评分和预后关系的研究[J]. 中国中西医结合消化杂志, 2021, 29(8): 555-558. https://www.cnki.com.cn/Article/CJFDTOTAL-ZXPW202108006.htm
[22] 赖震宇, 赵展庆, 余秉昌, 等. BISAP评分联合YKL-40和GIP对重症急性胰腺炎患者的预后评估[J]. 临床急诊杂志, 2022, 23(9): 649-654. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2022.09.008
-




 下载:
下载: