Research progress of intestinal mucosal barrier dysfunction in severe acute pancreatitis
-
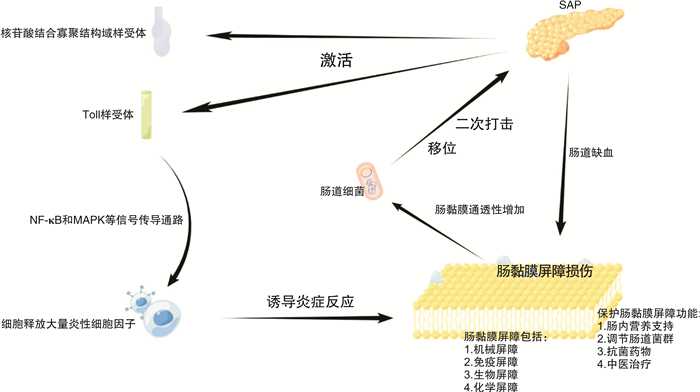
摘要: 重症急性胰腺炎(SAP)是临床上最常见的急腹症之一,病死率高,可伴有多脏器损伤,肠道是最晚修复的损伤器官。肠道不仅可以吸收营养物质,也可以抵御外来有害物质,肠黏膜屏障可阻断肠腔和人体内部组织,有效防止肠道外来有害物质进入血液循环,维持正常的肠道功能,降低肠源性感染的可能性。SAP可引起肠道缺血和缺氧,机体炎症反应也可破坏肠黏膜屏障,引起肠道细菌移位并损伤肠道功能,加速SAP的进展。本文检索大量SAP相关文献进行分析归纳,总结了SAP肠黏膜屏障功能损伤的机制,以期为SAP肠道损伤患者的临床诊疗提供参考和指导。Abstract: Severe acute pancreatitis(SAP) is one of the most common acute abdomen diseases in clinic, and it has a high mortality and can be accompanied by organ damage. The intestinal damage is the slowest to repair. The intestinal mucosal barrier(IB) blocks the intestinal cavity and the internal tissues of the body. The intestinal tract can not only absorb nutrients but also resist foreign harmful substances, effectively prevent foreign harmful substances in the intestinal tract from entering blood circulation, maintain normal intestinal function, and reduce the possibility of enterogenous infection. SAP can cause intestinal ischemia and hypoxia. The inflammatory response of the body can also directly damage the intestinal mucosal barrier, causing intestinal bacterial translocation. It can damage the intestinal function and accelerate the progress of SAP. In this paper, a large number of relevant literature were retrieved for analysis and summary, in order to help know the mechanism of intestinal mucosal barrier dysfunction of SAP and the part of intestinal mucosal barrier in the progression of SAP, and to guide the treatment of complications of SAP.
-

-
[1] Portelli M, Jones CD. Severe acute pancreatitis: pathogenesis, diagnosis and surgical management[J]. Hepatobiliary Pancreat Dis Int, 2017, 16(2): 155-159. doi: 10.1016/S1499-3872(16)60163-7
[2] Bushyhead D, Quigley EM. Small Intestinal Bacterial Overgrowth[J]. Gastroenterol Clin North Am, 2021, 50(2): 463-474. doi: 10.1016/j.gtc.2021.02.008
[3] Fukui H. Increased Intestinal Permeability and Decreased Barrier Function: Does It Really Influence the Risk of Inflammation?[J]. Inflamm Intest Dis, 2016, 1(3): 135-145. doi: 10.1159/000447252
[4] Brockmann JG, Hüsing-Kabar A, Bohlen K, et al. [Chronic intestinal failure][J]. Chirurg, 2022, 93(2): 205-214. doi: 10.1007/s00104-021-01423-8
[5] Usuda H, Okamoto T, Wada K. Leaky Gut: Effect of Dietary Fiber and Fats on Microbiome and Intestinal Barrier[J]. Int J Mol Sci, 2021, 22(14): 7613. doi: 10.3390/ijms22147613
[6] Camilleri M, Madsen K, Spiller R, et al. Intestinal barrier function in health and gastrointestinal disease[J]. Neurogastroenterol Motil, 2012, 24(6): 503-512. doi: 10.1111/j.1365-2982.2012.01921.x
[7] Cardoso-Silva D, Delbue D, Itzlinger A, et al. Intestinal Barrier Function in Gluten-Related Disorders[J]. Nutrients, 2019, 11(10): 2325. doi: 10.3390/nu11102325
[8] Suzuki T. Regulation of the intestinal barrier by nutrients: The role of tight junctions[J]. Anim Sci J, 2020, 91(1): e13357.
[9] Mehandru S, Colombel JF. The intestinal barrier, an arbitrator turned provocateur in IBD[J]. Nat Rev Gastroenterol Hepatol, 2021, 18(2): 83-84. doi: 10.1038/s41575-020-00399-w
[10] Nagalingam NA, Lynch SV. Role of the microbiota in inflammatory bowel diseases[J]. Inflamm Bowel Dis, 2012, 18(5): 968-984. doi: 10.1002/ibd.21866
[11] Hobby GP, Karaduta O, Dusio GF, et al. Chronic kidney disease and the gut microbiome[J]. Am J Physiol Renal Physiol, 2019, 316(6): F1211-F1217. doi: 10.1152/ajprenal.00298.2018
[12] Gooshe M, Abdolghaffari AH, Nikfar S, et al. Antioxidant therapy in acute, chronic and post-endoscopic retrograde cholangiopancreatography pancreatitis: An updated systematic review and meta-analysis[J]. World J Gastroenterol, 2015, 21(30): 9189-9208. doi: 10.3748/wjg.v21.i30.9189
[13] Sahoo BR. Structure of fish Toll-like receptors(TLR)and NOD-like receptors(NLR)[J]. Int J Biol Macromol, 2020, 161: 1602-1617. doi: 10.1016/j.ijbiomac.2020.07.293
[14] Tilstra JS, John S, Gordon RA, et al. B cell-intrinsic TLR9 expression is protective in murine lupus[J]. J Clin Invest, 2020, 130(6): 3172-3187. doi: 10.1172/JCI132328
[15] Yan Y, Lu B, Li P, et al. NOD receptor and TLR9 modulation in severe acute pancreatitis-induced intestinal injury[J]. Mol Med Rep, 2017, 16(6): 8471-8476. doi: 10.3892/mmr.2017.7661
[16] Root-Bernstein R. Synergistic Activation of Toll-Like and NOD Receptors by Complementary Antigens as Facilitators of Autoimmune Disease: Review, Model and Novel Predictions[J]. Int J Mol Sci, 2020, 21(13): 4645. doi: 10.3390/ijms21134645
[17] Hsu LC, Ali SR, McGillivray S, et al. A NOD2-NALP1 complex mediates caspase-1-dependent IL-1beta secretion in response to Bacillus anthracis infection and muramyl dipeptide[J]. Proc Natl Acad Sci U S A, 2008, 105(22): 7803-7808. doi: 10.1073/pnas.0802726105
[18] Xu S, Wei S, Guo Y, et al. Involvement of Nucleotide-Binding and Oligomerization Domain-Like Receptors in the Intestinal Injury of Severe Acute Pancreatitis in Rats[J]. Pancreas, 2018, 47(2): 245-251. doi: 10.1097/MPA.0000000000000977
[19] Wirtz TH, Puengel T, Buendgens L, et al. [Diagnosis and treatment of severe acute pancreatitis in critical care][J]. Dtsch Med Wochenschr, 2020, 145(12): 850-862. doi: 10.1055/a-0949-0878
[20] Wang YH. Current progress of research on intestinal bacterial translocation[J]. Microb Pathog, 2021, 152: 104652. doi: 10.1016/j.micpath.2020.104652
[21] Guo Y, Li H, Liu Z, et al. Impaired intestinal barrier function in a mouse model of hyperuricemia[J]. Mol Med Rep, 2019, 20(4): 3292-3300.
[22] Parada Venegas D, De la Fuente MK, Landskron G, et al. Corrigendum: Short Chain Fatty Acids(SCFAs)-Mediated Gut Epithelial and Immune Regulation and Its Relevance for Inflammatory Bowel Diseases[J]. Front Immunol, 2019, 10(5): 1486.
[23] Watanabe T, Asano N, Kudo M, et al. Nucleotide-binding oligomerization domain 1 and gastrointestinal disorders[J]. Proc Jpn Acad Ser B Phys Biol Sci, 2017, 93(8): 578-599. doi: 10.2183/pjab.93.037
[24] Li X, He C, Li N, et al. The interplay between the gut microbiota and NLRP3 activation affects the severity of acute pancreatitis in mice[J]. Gut Microbes, 2020, 11(6): 1774-1789. doi: 10.1080/19490976.2020.1770042
[25] Zhong K. Curcumin Mediates a Protective Effect Via TLR-4/NF-κB Signaling Pathway in Rat Model of Severe Acute Pancreatitis[J]. Cell Biochem Biophys, 2015, 73(1): 175-180. doi: 10.1007/s12013-015-0664-y
[26] James TW, Crockett SD. Management of acute pancreatitis in the first 72 hours[J]. Curr Opin Gastroenterol, 2018, 34(5): 330-335. doi: 10.1097/MOG.0000000000000456
[27] Reintam Blaser A, Starkopf J, Alhazzani W, et al. Early enteral nutrition in critically ill patients: ESICM clinical practice guidelines[J]. Intensive Care Med, 2017, 43(3): 380-398. doi: 10.1007/s00134-016-4665-0
[28] Kumar M, Kissoon-Singh V, Coria AL, et al. Probiotic mixture VSL reduces colonic inflammation and improves intestinal barrier function in Muc2 mucin-deficient mice[J]. Am J Physiol Gastrointest Liver Physiol, 2017, 312(1): G34-G45. doi: 10.1152/ajpgi.00298.2016
[29] Din AU, Hassan A, Zhu Y, et al. Inhibitory effect of Bifidobacterium bifidum ATCC 29521 on colitis and its mechanism[J]. J Nutr Biochem, 2020, 79: 108353. doi: 10.1016/j.jnutbio.2020.108353
[30] Ewaschuk JB, Diaz H, Meddings L, et al. Secreted bioactive factors from Bifidobacterium infantis enhance epithelial cell barrier function[J]. Am J Physiol Gastrointest Liver Physiol, 2008, 295(5): G1025-1034. doi: 10.1152/ajpgi.90227.2008
[31] 王锐, 韩秋菊, 敬慧丹. 重症急性胰腺炎合并腹腔感染的病原菌特点与治疗分析[J]. 临床急诊杂志, 2022, 23(1): 51-54. http://zzlc.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=0ce695e9-3c64-4607-adcd-73fb101da259
[32] Keeney KM, Yurist-Doutsch S, Arrieta MC, et al. Effects of antibiotics on human microbiota and subsequent disease[J]. Annu Rev Microbiol, 2014, 68: 217-235. doi: 10.1146/annurev-micro-091313-103456
[33] Langdon A, Crook N, Dantas G. The effects of antibiotics on the microbiome throughout development and alternative approaches for therapeutic modulation[J]. Genome Med, 2016, 8(1): 39. doi: 10.1186/s13073-016-0294-z
[34] 姚雪含, 刘喜平, 朱中博. 艾灸对菌群失调幼鼠结肠黏膜屏障的影响[J]. 中国中医药信息杂志, 2022, 29(8): 72-77. https://www.cnki.com.cn/Article/CJFDTOTAL-XXYY202208013.htm
[35] 余琳, 武晓灵. 香丹注射液联合乌司他丁治疗重症急性胰腺炎的疗效及对血液流变学和血清SOD、CRP、IL-6水平的影响[J]. 中国中西医结合消化杂志, 2021, 29(6): 421-425. doi: 10.3969/j.issn.1671-038X.2021.06.08
-




 下载:
下载: