Effect of fluid balance on short-term prognosis in patients of liver cirrhosis with hepatic encephalopathy
-
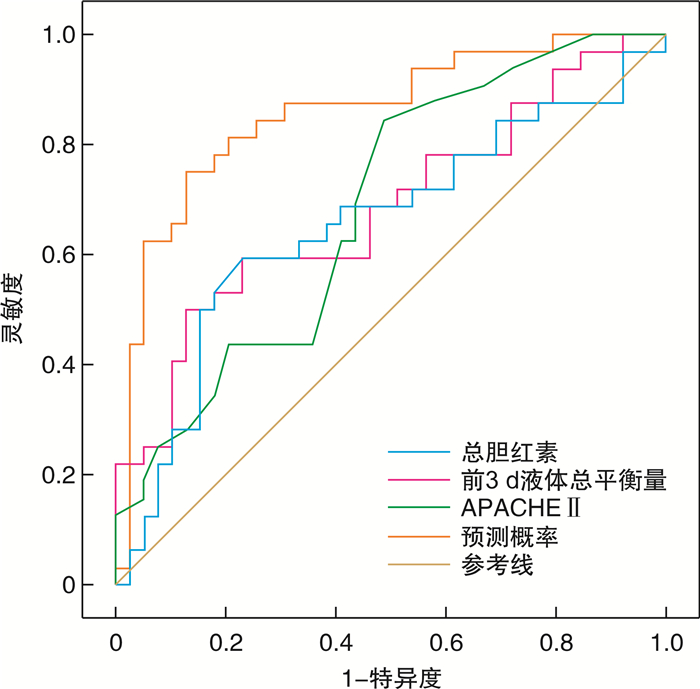
摘要: 目的 研究液体平衡对肝硬化合并肝性脑病患者短期预后的影响,为肝硬化合并肝性脑病患者早期合理的液体治疗提供依据。方法 回顾性分析2018年1月—2021年3月入住南京中医药大学附属南京医院重症医学科(ICU)的肝硬化合并肝性脑病患者共71例。根据患者转入ICU 28 d后是否存活分为存活组和死亡组,比较两组患者的各项数据,包括人口学特征(性别、年龄)、基础疾病(高血压、糖尿病等)、急性生理与慢性健康评分(APACHE Ⅱ)、实验室检查[白细胞、血小板、血红蛋白、血细胞比容、总胆红素、谷丙转氨酶、谷草转氨酶、白蛋白、凝血酶原活动度(PTA)、血清钾、血清钠、血乳酸、血氨等]、入ICU后前3 d液体总平衡量、住ICU时间等指标并进行统计学分析。两组间比较采用t检验或Mann-Whitney U检验,两组间计数资料采用χ2检验或Fisher确切概率法检验,应用logistic回归模型进行多因素分析,采用Pearson相关分析法分析两组患者入ICU后前3 d液体总平衡量与28 d生存率的关系。结果 单因素分析显示,两组患者APACHE Ⅱ评分、总胆红素值、PTA及前3 d液体总平衡量之间比较,差异有统计学意义(P<0.05)。两组患者多因素logistic回归分析显示,前3 d液体总平衡量(OR=1.000,95%CI:1.000~1.001)、总胆红素值(OR=1.006,95%CI:1.002~1.010)及APACHE Ⅱ评分(OR=1.152,95%CI:1.008~1.318)为肝硬化合并肝性脑病患者28 d预后的独立危险因素(P<0.05)。ROC曲线提示该模型预测肝硬化合并肝性脑病患者28 d预后的曲线下面积(AUC)为0.857(P<0.01,95%CI:0.767~0.948);Pearson相关分析显示前3 d液体总平衡量与生存率的相关系数为-0.366(P<0.05)。结论 入ICU后前3 d液体总平衡量、总胆红素值及APACHE Ⅱ评分是影响肝硬化合并肝性脑病患者28 d生存率的独立危险因素,前3 d总液体平衡量和生存率呈负相关,较少的液体入量可能会降低患者病死率。Abstract: Objective To study the effect of fluid balance on the short-term prognosis in patients of liver cirrhosis with hepatic encephalopathy, and to provide evidence for early and reasonable fluid therapy for patients with liver cirrhosis complicated with hepatic encephalopathy.Methods Seventy-one patients with cirrhosis and hepatic encephalopathy who were admitted to the intensive care unit(ICU) of Nanjing Hospital Affiliated to Nanjing University of Traditional Chinese Medicine from January 2018 to March 2021 were retrospectively analyzed. According to whether the patients survived 28 days after being transferred to the ICU, they were divided into the survival group and the death group. The data of the two groups of patients were compared, including demographic characteristics(sex, age), underlying diseases(hypertension, diabetes, etc.), acute physiology and chronic health evaluation(APACHE Ⅱ)score, laboratory tests(leukocytes, platelets, hemoglobin, hematocrit, total bilirubin, alanine aminotransferase, aspartate aminotransferase, albumin, prothrombin activity(PTA), serum potassium, serum sodium, blood lactate, blood ammonia, etc.), total fluid balance in the first 3 days after ICU admission, ICU stay time were statistically analyzed. The comparison between the two groups was performed by t test or Mann-Whitney U test, the count data between the two groups was by the χ2 test or Fisher's precise test, the logistic regression model was used for multivariate analysis, Pearson correlation analysis was used to analyze the relationship between the total fluid balance in the 3 days after admission to the ICU and the 28-day survival rate in the two groups.Results Univariate analysis showed that there were significant differences in APACHE Ⅱ score, , total bilirubin value, prothrombin activity and total fluid balance in the first 3 days between the two groups(P < 0.05). Multivariate logistic regression analysis showed that the total fluid balance in the first 3 days(OR=1.000, 95%CI: 1.000-1.001), total bilirubin value(OR=1.006, 95%CI: 1.002-1.010) and APACHE Ⅱ score(OR=1.152, 95%CI: 1.008-1.318) were independent risk factor for the 28-day prognosis of patients with liver cirrhosis and hepatic encephalopathy(P < 0.05); The ROC curve suggested that the area under the curve(AUC) of the model to predict the prognosis of patients with liver cirrhosis and hepatic encephalopathy at 28 days was 0.857(P < 0.01, 95%CI: 0.767-0.948); Pearson correlation analysis showed that the correlation coefficient between the total fluid balance in the first 3 days and the survival rate was -0.366(P < 0.05).Conclusion The total fluid balance in the first 3 days after admission to the ICU, total bilirubin and APACHE Ⅱ score are independent risk factors affecting the 28-day survival rate of patients with liver cirrhosis and hepatic encephalopathy. Total fluid balance in the first 3 days was negative correlated with survival, and less fluid intake may reduce the mortality of the patients.
-
Key words:
- liver cirrhosis /
- hepatic encephalopathy /
- liquid balance /
- prognosis
-

-
表 1 两组患者各项数据的单因素比较
X±S 指标 存活组(39例) 死亡组(32例) t/Z/χ2 P 年龄/岁 56.2±2.13 57.8±2.49 -0.492 0.624 男性/例(%) 25(64.1) 16(50) 1.433 0.231 高血压/例(%) 6(15.4) 8(25.0) 1.027 0.331 糖尿病/例(%) 6(15.4) 9(28.1) 1.712 0.191 APACHE Ⅱ评分/分 17.30±5.17 20.90±5.05 -2.989 0.004 白细胞/(×109·L-1) 7.23(4.66~11.60) 9.43(6.02~13.60) -1.572 0.116 血小板/(×109·L-1) 83(46~124) 57(35~109) -1.416 0.157 血红蛋白/(g·L-1) 97.4±30.6 99.9±23.1 -0.372 0.711 血细胞比容/% 28.5±8.7 29.9±6.5 -0.761 0.449 总胆红素/(μmol·L-1) 96(29~211) 267.9(54~453) -2.219 0.026 谷丙转氨酶/(U·L-1) 42(24~140) 68.1(23.8~214.0) -1.011 0.312 谷草转氨酶/(U·L-1) 68.5(45~144) 113(44.0~250.9) -1.063 0.288 白蛋白/(g·L-1) 30.0±4.5 31.3±3.7 -1.351 0.181 PTA/% 39.7(29.7~54.3) 29.2(18.4~39.6) -2.479 0.013 血清钾/(mmol·L-1) 4.01±0.74 3.86±0.58 1.212 0.230 血清钠/(mmol·L-1) 138.00±6.54 137.3±8.4 0.414 0.680 乳酸/(mmol·L-1) 2.91±2.20 3.73±1.7 -1.714 0.091 血氨/(mmol·L-1) 122(59~205) 137(113~224) -1.514 0.130 入ICU后前3 d液体总平衡量/mL -459.9±1109.3 622.7±1666.9 -3.270 0.002 住ICU时间/d 7(5~11) 7(4~10) -0.882 0.378 表 2 两组患者多因素logistic回归分析结果
变量 OR 95%CI P 前3 d液体总平衡量 1.001 (1.000~1.001) 0.002 总胆红素 1.006 (1.002~1.010) 0.001 APACHⅡ评分 1.152 (1.008~1.318) 0.038 -
[1] Ginès P, Krag A, Abraldes JG, et al. Liver cirrhosis. Lancet[J]. 2021, 398(10308): 1359-1376.
[2] Butterworth RF. Hepatic Encephalopathy in Cirrhosis: Pathology and Pathophysiology[J]. Drugs, 2019, 79(Suppl 1): 17-21.
[3] Weir V, Reddy KR. Nonpharmacologic Management of Hepatic Encephalopathy: An Update[J]. Clin Liver Dis, 2020, 24(2): 243-261. doi: 10.1016/j.cld.2020.01.003
[4] Dhondup T, Tien JC, Marquez A, et al. Association of negative fluid balance during the de-escalation phase of sepsis management with mortality: A cohort study[J]. J Crit Care, 2020, 55: 16-21. doi: 10.1016/j.jcrc.2019.09.025
[5] Messmer AS, Zingg C, Müller M, et al. Fluid Overload and Mortality in Adult Critical Care Patients-A Systematic Review and Meta-Analysis of Observational Studies[J]. Crit Care Med, 2020, 48(12): 1862-1870. doi: 10.1097/CCM.0000000000004617
[6] 徐小元, 丁惠国, 李文刚, 等. 肝硬化肝性脑病诊疗指南[J]. 中华肝脏病杂志, 2018, 26(10): 721-736. doi: 10.3760/cma.j.issn.1007-3418.2018.10.001
[7] Hadjihambi A, Arias N, Sheikh M, et al. Hepatic encephalopathy: a critical current review[J]. Hepatol Int, 2018, 12(Suppl 1): 135-147.
[8] Rose CF, Amodio P, Bajaj JS, et al. Hepatic encephalopathy: Novel insights into classification, pathophysiology and therapy[J]. J Hepatol, 2020, 73(6): 1526-1547. doi: 10.1016/j.jhep.2020.07.013
[9] Malbrain MLNG, Van Regenmortel N, Saugel B, et al. Principles of fluid management and stewardship in septic shock: it is time to consider the four D's and the four phases of fluid therapy[J]. Ann Intensive Care, 2018, 8(1): 66. doi: 10.1186/s13613-018-0402-x
[10] Evans L, Rhodes A, Alhazzani W, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2021[J]. Crit Care Med, 2021, 49(11): e1063-e1143. doi: 10.1097/CCM.0000000000005337
[11] Vincent JL. Fluid management in the critically ill[J]. Kidney Int, 2019, 96(1): 52-57. doi: 10.1016/j.kint.2018.11.047
[12] Zhang L, Xu F, Li S, et al. Influence of fluid balance on the prognosis of patients with sepsis[J]. BMC Anesthesiol, 2021, 21(1): 269. doi: 10.1186/s12871-021-01489-1
[13] 李芬, 邢柏, 李诗阳. 基于数据挖掘评估累积液体平衡对重症患者ICU重返率及死亡率的影响[J]. 临床急诊杂志, 2019, 20(12): 935-940. http://zzlc.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=291ffd5e-2953-4b2a-b46f-786c46344f90
[14] Jhee JH, Park JY, An JN, et al. Cumulative fluid balance and mortality in elderly patients with acute kidney injury requiring continuous renal-replacement therapy: a multicenter prospective cohort study[J]. Kidney Res Clin Pract, 2020, 39(4): 414-425. doi: 10.23876/j.krcp.20.089
[15] Wiegers EJA, Lingsma HF, Huijben JA, et al. Fluid balance and outcome in critically ill patients with traumatic brain injury(CENTER-TBI and OzENTER-TBI): a prospective, multicentre, comparative effectiveness study[J]. Lancet Neurol, 2021, 20(8): 627-638. doi: 10.1016/S1474-4422(21)00162-9
[16] 赵千文, 李秋红, 谢玉萍. 限制性液体负平衡治疗急性呼吸窘迫综合征患者的效果观察[J]. 临床急诊杂志, 2020, 21(9): 707-710. http://zzlc.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=7589827f-33cb-4dd1-8c96-1175fe57f99f
[17] Alobaidi R, Morgan C, Basu RK, et al. Association between fluid balance and outcomes in critically ill children: a systematic review and meta-analysis[J]. JAMA Pediatr, 2018, 172(3): 257-268. doi: 10.1001/jamapediatrics.2017.4540
[18] Jaffe A, Lim JK, Jakab SS. Pathophysiology of Hepatic Encephalopathy[J]. Clin Liver Dis, 2020, 24(2): 175-188. doi: 10.1016/j.cld.2020.01.002
[19] Spacek L A, Strzepka A, Saha S, et al. Repeated Measures of Blood and Breath Ammonia in Response to Control, Moderate and High Protein Dose in Healthy Men[J]. Sci Rep, 2018, 8(1): 2554. doi: 10.1038/s41598-018-20503-0
[20] Liotta EM, Romanova AL, Lizza BD, et al. Osmotic Shifts, Cerebral Edema, and Neurologic Deterioration in Severe Hepatic Encephalopathy[J]. Crit Care Med, 2018, 46(2): 280-289. doi: 10.1097/CCM.0000000000002831
[21] Valantine B, Sundaray N, Mishra D, et al. Predictors of early mortality among patients with acute-on-chronic liver failure[J]. JGH Open, 2021, 5(6): 686-694. doi: 10.1002/jgh3.12557
[22] Karagoz S, Tekdos Seker Y, Cukurova Z, et al. The Effectiveness of Scoring Systems in the Prediction of Diagnosis-Based Mortality[J]. Ther Apher Dial, 2019, 23(5): 418-424. doi: 10.1111/1744-9987.12780
-




 下载:
下载: