Consistency study of lung ultrasound and CT imaging in the assessment of traumatic acute respiratory distress syndrome
-
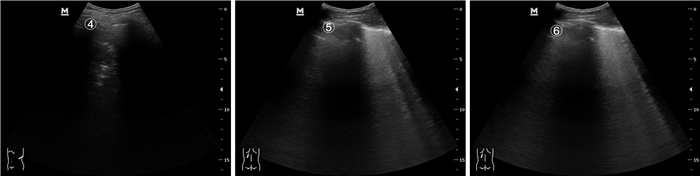
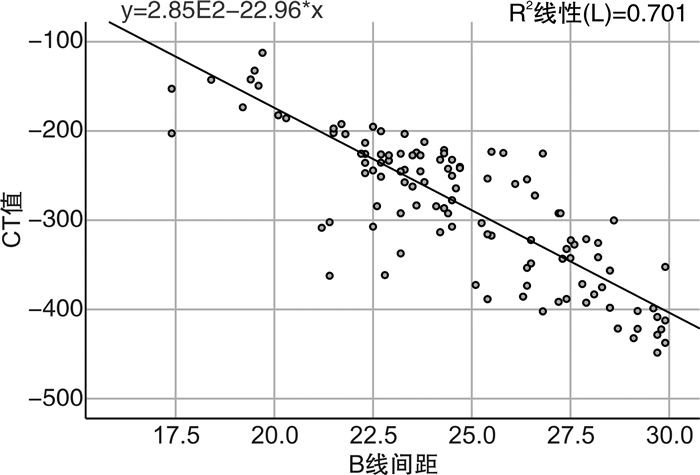
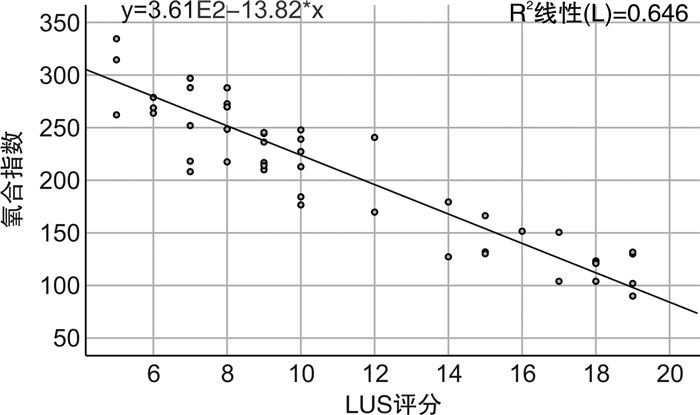
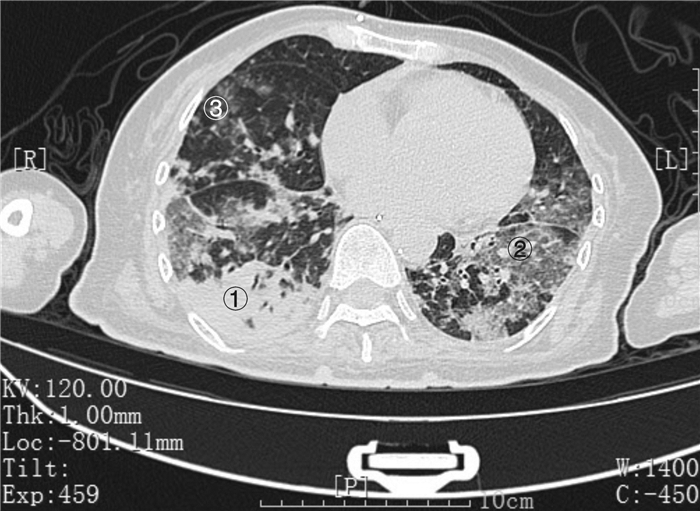
摘要: 目的 探讨肺部超声技术在创伤性急性呼吸窘迫综合征(ARDS)患者中的诊断评估价值。方法 将2020年6月-2021年9月期间在常熟市第二人民医院急诊医学科收治的因创伤住院继发ARDS的85例患者纳入本研究,采用床边超声探查患者两侧各区肺部影像,与肺CT影像对照,分析两种方法影像表现的一致性,明确肺部超声评估创伤性ARDS的准确性。结果 肺部超声诊断发现的肺部阳性病灶与肺部CT具有高度一致性,超声手段发现病灶的阳性率为75.2%,而CT检查则为78.7%。肺部超声图像改变与肺部CT影像学特征变化具有高度一致性(κ=0.828,P<0.001),两者在评估肺部病变中差异有统计学意义(P<0.001)。B线间距与CT值呈负相关(r=-0.837,P<0.001),B线间距越短,CT值越高,提示病变越重。肺超声评分(LUS)与氧合指数呈负相关(r=-0.772,P<0.001),LUS评分越高提示肺部病变越重,氧合情况越差,ARDS程度越重。结论 创伤性ARDS患者肺部超声与肺部CT影像有较好的一致性,肺部超声能准确识别其肺部特征性改变,在急危重患者救治时可替代CT进行影像学评估。Abstract: Objective To explore the diagnostic evaluation value of lung ultrasound in patients with traumatic acute respiratory distress syndrome(ARDS).Methods A total of 85 patients with ARDS secondary to trauma admitted to the Changshu NO. 2 People's Hospital from June 2020 to September 2021 were enrolled. Bedside ultrasound was used to explore the lung images of each area on both sides of the patient, and compared with lung CT images to analyze the consistency of the imaging performance of the two methods, and to clarify the accuracy of lung ultrasound in evaluating traumatic ARDS.Results The positive lung lesions found in lung ultrasound diagnosis were highly consistent with lung CT. The positive rate of lesions detected by ultrasound was 75.2%, while that of CT examination was 78.7%. The changes of lung ultrasound images were highly consistent with the changes of lung CT imaging features(κ=0.828, P < 0.001), and there was a statistical difference between the two in evaluating lung lesions(P < 0.001). B-line spacing was negatively correlated with CT value(r=-0.837, P < 0.001), the shorter the B-line spacing, the higher the CT value, which indicated the heavier the lesion. The LUS score was negatively correlated with the oxygenation index(r=-0.772, P < 0.001). The higher the LUS score, the more severe the lung disease, the worse the oxygenation, and the more severe the degree of ARDS.Conclusion The lung ultrasound and lung CT images of traumatic ARDS patients have good consistency. Lung ultrasound can accurately identify the characteristic changes of the lungs, and can replace CT for imaging evaluation in the treatment of critically ill patients.
-
Key words:
- ultrasound /
- trauma /
- acute respiratory distress syndrome /
- CT value /
- diagnosis
-

-
表 1 LUS评分标准
分 分区 正常 1~2个彗星尾征 3个以上彗星尾征 肺实变、肺不张 液性暗区 前区 0 1 4 5 1 侧区 0 1 3 4 1 后区 0 1 2 3 0 表 2 超声检查和CT检查阳性肺区比例数的比较
个(%) 分组 肺区总计 阳性个数 阴性个数 一致性 κ χ2 P 超声检查CT检查 1020 768(75.2) 802(78.7) 252(24.8) 218(21.3) 高度一致 0.718 531.1 <0.001 表 3 LUS及肺部CT诊断一致性比较
个 超声图像表现 CT影像表现 一致性评价 κ χ2 P 正常(肺区) 毛玻璃影(肺区) 弥漫渗出(肺区) 间质改变(肺区) 肺不张(肺区) 正常(肺区) 232 20 0 0 0 高度一致 0.828 18.06 0.003 B7线(肺区) 3 152 25 5 3 B3线(肺区) 0 8 132 32 7 融合成片(肺区) 0 2 22 156 10 碎片征(肺区) 0 0 0 4 208 -
[1] 连细华, 吕国荣, 朱志兴, 等. 肺部超声B线征与肺水肿病理的相关性研究[J]. 中国超声医学杂志, 2020, 36(2): 181-184. doi: 10.3969/j.issn.1002-0101.2020.02.026
[2] Fan E, Brodie D, Slutsky AS. Acute Respiratory Distress Syndrome: Advances in Diagnosis and Treatment[J]. JAMA, 2018, 319(7): 698-710. doi: 10.1001/jama.2017.21907
[3] Bellani G, Laffey JG, Pham T, et al. Epidemiology, Patterns of Care, and Mortality for Patients With Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries[J]. JAMA, 2016, 316(3): 350.
[4] Manivel V, Lesnewski A, Shamim S, et al. CLUE: COVID-19 lung ultrasound in emergency department[J]. Emerg Med Australas, 2020, 32(4): 694-696. doi: 10.1111/1742-6723.13546
[5] 乔莉, 马元, 张劲松. 急性呼吸窘迫综合征: 柏林标准[J]. 中华急诊医学杂志, 2012, 21(9): 952-957. doi: 10.3760/cma.j.issn.1671-0282.2012.09.006
[6] Ferguson ND, Fan E, Camporota L, et al. The Berlin definition of ARDS: an expanded rationale, justification, and supplementary material[J]. Intensive Care Med, 2012, 38(10): 1573-1582. doi: 10.1007/s00134-012-2682-1
[7] 李黎明, 李莲花, 关键, 等. 肺部超声评分在呼吸机相关性肺炎疗效评价中的作用[J]. 中华内科杂志, 2016, 55(12): 950-952. doi: 10.3760/cma.j.issn.0578-1426.2016.12.009
[8] Wang G, Ji X, Xu Y, et al. Lung ultrasound: a promising tool to monitor ventilator-associated pneumonia in critically ill patients[J]. Crit Care, 2016, 20(1): 320. doi: 10.1186/s13054-016-1487-y
[9] Huppert LA, Matthay MA, Ware LB. Pathogenesis of Acute Respiratory Distress Syndrome[J]. Semin Respir Crit Care Med, 2019, 40(1): 31-39. doi: 10.1055/s-0039-1683996
[10] Tasaka S, Ohshimo S, Takeuchi M, et al. ARDS Clinical Practice Guideline 2021[J]. J Intensive Care, 2022, 10(1): 32. doi: 10.1186/s40560-022-00615-6
[11] Bernard GR, Artigas A, Brigham KL, et al. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination[J]. Am J Respir Crit Care Med, 1994, 149(3 Pt 1): 818-824.
[12] Pham T, Rubenfeld GD. Fifty Years of Research in ARDS. The Epidemiology of Acute Respiratory Distress Syndrome. A 50th Birthday Review[J]. Am J Respir Crit Care Med, 2017, 195(7): 860-870. doi: 10.1164/rccm.201609-1773CP
[13] Allinovi M, Parise A, Giacalone M, et al. Lung Ultrasound May Support Diagnosis and Monitoring of COVID-19 Pneumonia[J]. Ultrasound Med Biol, 2020, 46(11): 2908-2917. doi: 10.1016/j.ultrasmedbio.2020.07.018
[14] 朱海云, 段军, 孙艳文, 等. 急诊床旁肺部超声在诊断ICU术后低氧血症中的价值[J]. 中国中西医结合急救杂志, 2019, 26(3): 293-295. doi: 10.3969/j.issn.1008-9691.2019.03.009
[15] Brat R, Yousef N, Klifa R, et al. Lung Ultrasonography Score to Evaluate Oxygenation and Surfactant Need in Neonates Treated With Continuous Positive Airway Pressure[J]. JAMA Pediatr, 2015, 169(8): e151797. doi: 10.1001/jamapediatrics.2015.1797
[16] 张颖, 连细华, 黄顺发, 等. 肺部超声与高分辨率CT评估间质性肺疾病的对比研究[J]. 临床超声医学杂志, 2021, 23(5): 365-368. doi: 10.3969/j.issn.1008-6978.2021.05.013
[17] Broderick, Joseph C, et al. Combat Trauma-Related Acute Respiratory Distress Syndrome: A Scoping Review[J]. Crit Care Explor, 2022, 4(9): e0759. doi: 10.1097/CCE.0000000000000759
[18] 刘月, 郭丽苹, 杨爽, 等. 床旁肺超声实时动态评估危重症患者肺炎病情严重程度的应用价值[J]. 临床急诊杂志, 2022, 23(2): 87-90. http://zzlc.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=242cbd29-58a4-4fe7-8eb2-c8f1e324e6eb
[19] Koch V, Gruenewald LD, Albrecht MH, et al. Lung Opacity and Coronary Artery Calcium Score: A Combined Tool for Risk Stratification and Outcome Prediction in COVID-19 Patients[J]. Acad Radiol, 2022: S1076-6332(22)00129-5.
[20] 彭誉, 李佳. 肺超声在静脉-静脉体外膜肺患者行俯卧位通气治疗中的应用价值[J]. 临床急诊杂志, 2021, 22(9): 603-608. http://zzlc.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=02eaaf56-9d2b-4ebd-97a9-272f634ee870
[21] Chiumello D, Mongodi S, Algieri I, et al. Assessment of Lung Aeration and Recruitment by CT Scan and Ultrasound in Acute Respiratory Distress Syndrome Patients[J]. Crit Care Med, 2018, 46(11): 1761-1768. doi: 10.1097/CCM.0000000000003340
[22] Biasucci DG, Buonsenso D, Piano A, et al. Lung ultrasound predicts non-invasive ventilation outcome in COVID-19 acute respiratory failure: a pilot study[J]. Minerva Anestesiol, 2021, 87(9): 1006-1016.
[23] 高平, 许菡苡, 劳妙婵. 阻塞性通气功能障碍合并肺动脉高压患者肺叶平均CT值差异性的研究[J]. 国际呼吸杂志, 2020, 40(23): 1796-1800.
[24] Zieleskiewicz L, Markarian T, Lopez A, et al. Comparative study of lung ultrasound and chest computed tomography scan in the assessment of severity of confirmed COVID-19 pneumonia[J]. Intensive Care Med, 2020, 46(9): 1707-1713.
-




 下载:
下载: