Effects of high-volume hemofiltration on Th17/Treg imbalance in patients with acute pancreatitis in the intensive care unit
-
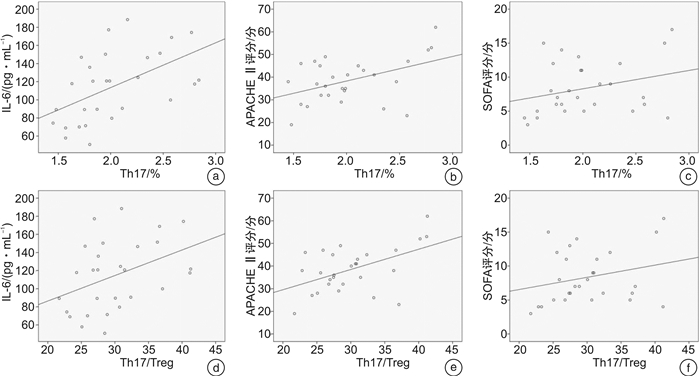
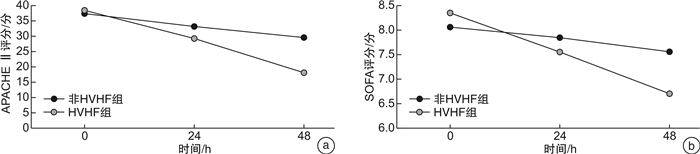
摘要: 目的 探究持续性高容量血液滤过(HVHF)对ICU重症急性胰腺炎(SAP)患者Th17/Treg失衡的影响。方法 选取2020年1月-2021年4月ICU收治的56例SAP患者为研究组,分为HVHF组(n=28)和非HVHF组(n=28)。另选取同期做健康体检的28例志愿者为对照组,提取外周血单个核细胞(PBMCs),采用流式细胞术检测Th17、Treg的百分率,采用酶联免疫吸附试验(ELISA)检测血清细胞炎症因子水平,并于治疗前、治疗24 h、48 h时评估急性生理与慢性健康评分Ⅱ(APACHEⅡ)及序贯器官功能衰竭评分(SOFA)。结果 研究组SAP患者Th17、Treg、Th17/Treg及血清IL-6、IL-10、IL-17、IL-23、转化生长因子-β(TGF-β)水平均显著高于对照组(P<0.05)。治疗12 h及24 h后,HVHF组患者Th17、Treg、Th17/Treg、IL-6、IL-10、IL-17、IL-23、TGF-β水平逐渐降低,与非HVHF组比较差异有统计学意义(P<0.05)。HVHF组患者在治疗24 h及48 h后APACHEⅡ评分、SOFA评分较基线值显著降低(P<0.05)。根据SAP患者在ICU住院期间死亡情况分为存活组(n=48)及非存活组(n=8),非存活组患者Th17、Treg、Th17/Treg、IL-6、IL-10、IL-17、IL-23、TGF-β基线值显著高于存活组(P<0.05)。经Spearman及Pearson分析,HVHF组患者基线Th17水平分别与IL-6水平及APACHEⅡ评分、SOFA评分呈正相关(r=0.525、0.347、0.286,P<0.001);基线Th17/Treg水平亦与血清IL-6水平及APACHEⅡ评分、SOFA评分呈正相关(r=0.402、0.389、0.265,P<0.001)。结论 HVHF治疗可在短时间内更好地消除炎症因子的过度分泌,纠正Th17/Treg失衡,进而有助于改善患者的预后。Abstract: Objective To investigate the effect of continuous high-volume hemofiltration(HVHF) on the imbalance of IL-17-producing CD4+T helper(Th17)/regulatory T(Treg) cells in intensive care unit(ICU) patients with severe acute pancreatitis(SAP).Methods Fifty-six patients with SAP admitted to ICU of our hospital from January 2020 to April 2021 were selected as the study subjects, including HVHF group(n=28) and non-HVHF group(n=28). In addition, 28 volunteers who underwent health examination in our hospital during the same period were selected as the control group. Peripheral blood mononuclear cells(PBMCs) were extracted, the percentage of Th17 and Treg were detected by flow cytometry, and the levels of serum inflammatory cytokines were detected by enzyme linked immunosorbent assay(ELISA).The acute physiological and chronic health evaluationⅡ(APACHEⅡ) score and sequential organ failure assessment(SOFA) score were assessed before treatment and at 24 h, and 48 h of treatment.Results Th17, Treg, Th17/Treg, IL-6, IL-10, IL-17, IL-23 and transforming growth factor-β(TGF-β) in patients with SAP were significantly higher than those in the control group(P < 0.05).The levels of Th17, Treg, Th17/Treg, IL-6, IL-10, IL-17, IL-23 and TGF-β in HVHF group decreased gradually, and there was a significant difference between the HVHF group and non-HVHF group(P < 0.05).The APACHE Ⅱ and SOFA baseline scores of patients in the HVHF group were significantly lower than the baseline value after 24 h and 48 h of treatment(P < 0.05). According to the life-or-death situation of SAP patients during ICU hospitalization, the patients were divided into the survival group(n=48) and non-survival group(n=8). Th17, Treg, Th17/Treg, IL-6, IL-10, IL-17, IL-23, and TGF-β in the non-survival group were significantly higher than those in the survival group(P < 0.05). Spearman and Pearson analysis showed that baseline Th17 level was a positive correlation with IL-6 level and APACHEⅡ and SOFA scores(r=0.525, 0.347, 0.286, P < 0.001). Baseline Th17/Treg levels were positive correlation with IL-6 levels and APACHEⅡ and SOFA scores(r=0.402, 0.389, 0.265, P < 0.001).Conclusion HVHF therapy can better eliminate the oversecretion of inflammatory factors in a short time, change the levels of Th17 and Treg, correct the Th17/Treg imbalance, and improve the clinical symptoms and prognosis of patients.
-
Key words:
- acute pancreatitis /
- high-volume hemofiltration /
- CD4+T helper cell /
- egulatory T cell
-

-
表 1 研究组和对照组Th17、Treg、Th17/Treg及血清细胞因子水平的比较
X±S 指标 对照组(n=28) 研究组(n=56) t P Th17/% 0.49±0.19 2.01±0.43 17.810 <0.001 Treg/% 4.11±0.26 6.79±0.42 30.880 <0.001 Th17/Treg 0.12±0.05 0.29±0.05 14.690 <0.001 IL-6/(pg·mL-1) 25.99±9.11 106.34±42.43 9.879 <0.001 IL-10/(pg·mL-1) 79.86±24.72 128.76±42.94 5.572 <0.001 IL-17/(pg·mL-1) 25.65±9.09 59.36±28.22 6.147 <0.001 IL-23/(pg·mL-1) 117.68±35.02 280.09±153.13 5.525 <0.001 TGF-β/(pg·mL-1) 300.44±89.10 1 037.41±354.21 10.810 <0.001 表 2 HVHF组和非HVHF组SAP患者的临床资料比较
X±S,例(%) 临床资料 非HVHF组(n=28) HVHF组(n=28) t/x2 P 年龄/岁 59.21±17.31 59.61±14.96 0.093 0.927 男 13(46.43) 16(57.14) 0.644 0.422 器官受累 单器官衰竭 17(60.71) 15(53.57) 0.292 0.589 MODS 11(39.29) 13(46.43) 合并症 高血压 6(21.43) 4(14.29) 0.487 0.485 冠心病 2(7.14) 3(10.71) 0.220 0.639 糖尿病 3(10.71) 3(10.71) COPD 2(7.14) 3(10.71) 0.220 0.639 脑梗死 1(3.57) 0 1.018 0.313 APACHEⅡ评分/分 37.46±9.84 38.57±9.86 0.422 0.675 SOFA评分/分 8.07±4.28 8.36±3.93 0.264 0.793 乳酸/(mg·L-1) 4.45±2.32 4.27±2.19 0.299 0.767 Scr/(μmol·L-1) 100.71±39.37 107.49±42.94 0.616 0.541 MAP/mmHga) 58.54±10.74 58.68±8.13 0.056 0.956 使用米力农治疗 12(42.85) 9(32.14) 0.686 0.408 注:a)1 mmHg=0.133 kPa。 表 3 HVHF组与非HVHF组患者各时间点Th17、Treg、Th17/Treg及血清细胞因子水平比较
X±S 指标 HVHF组(n=28) 非HVHF组(n=28) F时间,P F组别,P F组别×时间,P Th17/% 0 h 2.03±0.41 1.99±0.45 6 h 2.01±0.38 2.04±0.45 21.225,<0.001 2.280,0.143 11.927,<0.001 12 h 1.82±0.37 2.05±0.52 24 h 1.65±0.45 1.94±0.48 Treg/% 0 h 6.72±0.33 6.87±0.49 6 h 6.73±0.34 6.64±0.66 66.519,<0.001 5.514,0.026 8.714,<0.001 12 h 6.18±0.51 6.55±0.51 24 h 6.00±0.45 6.33±0.51 Th17/Treg 0 h 0.30±0.05 0.29±0.05 6 h 0.30±0.05 0.31±0.06 3.445,0.020 0.648,0.428 5.157,0.003 12 h 0.28±0.06 0.32±0.08 24 h 0.26±0.08 0.32±0.07 IL-6/(pg·mL-1) 0 h 114.81±38.53 97.87±45.10 6 h 106.76±38.07 104.73±46.51 16.973,<0.001 0.022,0.882 16.215,<0.001 12 h 89.09±37.93 108.93±48.57 24 h 80.79±36.29 98.74±48.29 IL-10/(pg·mL-1) 0 h 134.21±43.37 123.30±42.58 6 h 126.43±46.38 124.37±46.86 84.985,<0.001 0.098,0.756 10.297,<0.001 12 h 105.25±47.27 119.56±51.36 24 h 88.29±43.20 113.00±51.68 IL-17/(pg·mL-1) 0 h 60.99±30.15 57.72±26.60 6 h 58.42±24.64 59.01±30.21 19.718,<0.001 0.432,0.517 6.014,0.001 12 h 48.82±19.77 56.06±22.97 24 h 40.50±14.08 52.16±25.21 IL-23/(pg·mL-1) 0 h 283.99±136.02 276.19±170.97 6 h 276.06±153.13 291.73±213.32 25.454,<0.001 0.268,0.609 5.956,0.001 12 h 236.85±141.28 280.65±194.86 24 h 199.93±162.07 260.16±191.14 TGF-β/(pg·mL-1) 0 h 1 003.83±330.95 1 070.99±379.09 6 h 1 050.47±436.30 1 076.47±395.77 20.821, <0.001 1.297, 0.265 2.944, 0.038 12 h 845.97±443.89 1 016.20±416.28 24 h 731.72±403.41 984.04±402.17 表 4 不同生存结局的SAP患者Th17、Treg、Th17/Treg及血清细胞因子水平比较
X±S 指标 存活组(n=48) 非存活组(n=8) t/χ2 P Th17/% 1.94±0.40 2.43±0.37 3.238 0.002 Treg/% 6.74±0.41 7.09±0.39 2.249 0.029 Th17/Treg 0.29±0.05 0.34±0.04 2.682 0.01 IL-6/(pg·mL-1) 101.73±40.40 134.03±46.55 2.051 0.045 IL-10/(pg·mL-1) 121.74±41.04 170.85±28.60 3.244 0.002 IL-17/(pg·mL-1) 53.47±25.21 94.67±18.05 4.421 <0.001 IL-23/(pg·mL-1) 246.98±116.44 478.78±201.41 4.647 <0.001 TGF-β/(pg·mL-1) 979.62±315.74 1 384.12±395.18 3.238 0.002 -
[1] 钟浩亮, 孙备. 急性胰腺炎的多学科治疗[J]. 临床急诊杂志, 2021, 22(3): 163-167. http://zzlc.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=a2978009-128a-40c8-a118-7d39e93ccc9a
[2] 张娟, 章润叶, 杨淑洁, 等. 实验室指标和评分系统对急性胰腺炎患者病情严重程度及早期预后的评估价值[J]. 临床急诊杂志, 2021, 22(1): 50-54. http://zzlc.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=099d1d39-ea76-429f-801d-722ea00d3c89
[3] Wang D, Tang M, Zong P, et al. MiRNA-155 Regulates the Th17/Treg Ratio by Targeting SOCS1 in Severe Acute Pancreatitis[J]. Front Physiol, 2018, 9: 686. doi: 10.3389/fphys.2018.00686
[4] Guo Y, Cao F, Li C, et al. Continuous Hemofiltration Reduces Mortality in Severe Acute Pancreatitis: A Meta-Analysis[J]. Emerg Med Int, 2020, 2020: 6474308.
[5] Huang H, Zhou Q, Chen MH. High-volume hemofiltration reduces short-term mortality with no influence on the incidence of MODS, hospital stay, and hospitalization cost in patients with severe-acute pancreatitis: A meta-analysis[J]. Artif Organs, 2021, 45(12): 1456-1465. doi: 10.1111/aor.14016
[6] 中华医学会外科学分会胰腺外科学组. 急性胰腺炎诊治指南(2014版)[J]. 中华消化外科杂志, 2015, 14(1): 1-5. doi: 10.3760/cma.j.issn.1673-9752.2015.01.001
[7] Zhou H, Mei X, He X, et al. Severity stratification and prognostic prediction of patients with acute pancreatitis at early phase: A retrospective study[J]. Medicine(Baltimore), 2019, 98(16): e15275.
[8] Basile-Filho A, Lago AF, Menegueti MG, et al. The use of APACHEⅡ, SOFA, SAPS 3, C-reactive protein/albumin ratio, and lactate to predict mortality of surgical critically ill patients: A retrospective cohort study[J]. Medicine(Baltimore), 2019, 98(26): e16204.
[9] 陈静. 急性胰腺炎患者外周血中Th17和Treg细胞及其细胞因子水平变化[J]. 空军医学杂志, 2016, 32(6): 368-371. https://www.cnki.com.cn/Article/CJFDTOTAL-ZJZY201606006.htm
[10] 林凯, 齐育英, 王开银, 等. 免疫性甲状腺疾病患者肠道菌群分布及其对Th17/Treg细胞的影响[J]. 中国微生态学杂志, 2022, 34(3): 318-322, 326-326. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGWS202203014.htm
[11] 穆蕊, 余剑波. 脓毒症相关性脑病与免疫功能障碍的研究进展[J]. 中国中西医结合外科杂志, 2022, 28(1): 132-136. doi: 10.3969/j.issn.1007-6948.2022.01.025
[12] 陈曼芹, 史菲. 细胞因子在脓毒症诊断及预后的研究进展[J]. 岭南急诊医学杂志, 2022, 27(1): 98-100. https://www.cnki.com.cn/Article/CJFDTOTAL-LNJZ202201040.htm
[13] 叶瑞, 胡炜, 刘炳炜, 等. 脓毒症患者T淋巴细胞亚群变化及与炎症状态的关系研究[J]. 中国现代医学杂志, 2019, 29(17): 41-47. doi: 10.3969/j.issn.1005-8982.2019.17.008
[14] Tozlu M, Kayar Y, Ince AT, et al. Low molecular weight heparin treatment of acute moderate and severe pancreatitis: A randomized, controlled, open-label study[J]. Turk J Gastroenterol, 2019, 30(1): 81-87.
[15] 郑智, 曲元旭, 丁乙轩, 等. 急性胰腺炎发病机制的研究进展[J]. 中华肝胆外科杂志, 2021, 27(2): 152-155. doi: 10.3760/cma.j.cn113884-20200411-00192
[16] 蔡照弟, 奚耀, 王重卿. 清胰通腑汤联合生长抑素对重症急性胰腺炎并发麻痹性肠梗阻患者Th17/Treg细胞平衡及相关因子的影响[J]. 中国中医急症, 2019, 28(12): 2142-2145. doi: 10.3969/j.issn.1004-745X.2019.12.019
[17] 刘洁, 胡小辉, 龚道恺. 急性脑梗死患者外周血Th17、Treg、Th17/Treg及炎症因子的动态变化过程研究[J]. 临床神经病学杂志, 2020, 33(2): 102-105. doi: 10.3969/j.issn.1004-1648.2020.02.006
[18] 田洲, 王嘉菲, 李萌, 等. TNF-α和TIPE2在急性胰腺炎患者外周血中的表达及与疾病严重程度的关系[J]. 临床急诊杂志, 2021, 22(11): 742-746. http://zzlc.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=0f7513ff-2192-462a-aa73-432c42b2b8d9
[19] Fasching P, Stradner M, Graninger W, et al. Therapeutic potential of targeting the Th17/Treg axis in autoimmune disorders[J]. Molecules, 2017, 22(1): 134-157. doi: 10.3390/molecules22010134
[20] Yuliasih Y, Rahmawati LD, Putri RM. Th17/Treg Ratio and Disease Activity in Systemic Lupus Erythematosus[J]. Caspian J Intern Med, 2019, 10(1): 65-72.
[21] Liu B, Ren H, Chen J. LncRNA NEAT1 correlates with Th1 and Th17 and could serve as an assistant biomarker in sepsis[J]. Biomark Med, 2021, 15(13): 1177-1186. doi: 10.2217/bmm-2020-0906
[22] Zhao Q, Manohar M, Wei Y, et al. STING signalling protects against chronic pancreatitis by modulating Th17 response[J]. Gut, 2019, 68(10): 1827-1837. doi: 10.1136/gutjnl-2018-317098
[23] 谢春阳, 王秀坤, 游雪甫. 治疗脓毒症药物研究进展[J]. 药学学报, 2020, 55(3): 413-420. https://www.cnki.com.cn/Article/CJFDTOTAL-YXXB202003009.htm
[24] 马志兰, 孙雪婷, 梁艳琴. 血液净化对重症急性胰腺炎合并MODS患者Th17/Treg细胞平衡的影响[J]. 中华医院感染学杂志, 2020, 30(15): 2347-2351. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHYY202015025.htm
[25] Rokyta R Jr, Holub M, Matejovic M, et al. Continuous venovenous hemofiltration: effects on monocyte and lymphocyte immunophenotype in critically ill patients[J]. Int J Artif Organs, 2002, 25(11): 1066-1073. doi: 10.1177/039139880202501105
-




 下载:
下载: