The value of NLR combined with MPR in auxiliary diagnosis and evaluation of sepsis patients
-
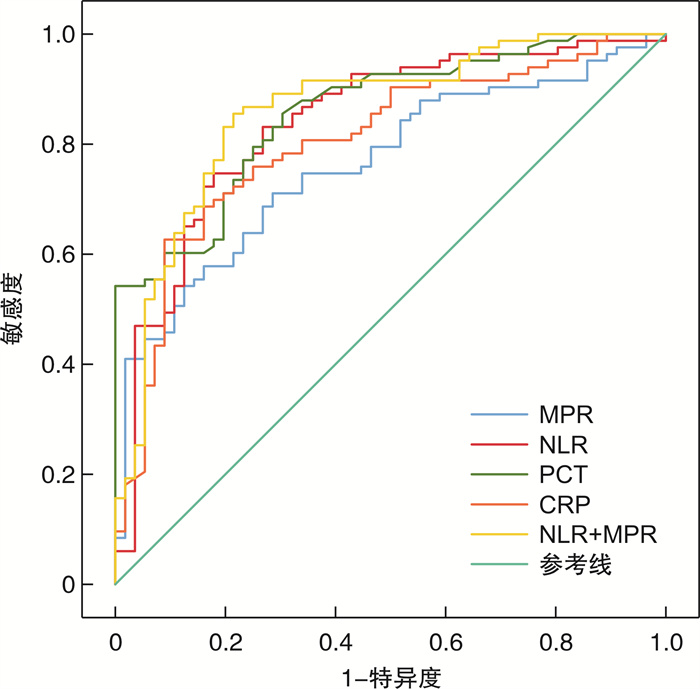
摘要: 目的 探讨中性粒细胞/淋巴细胞比值(NLR)联合平均血小板体积/血小板计数比值(MPR)对脓毒症患者辅助诊断及病情评估的价值。方法 回顾性分析2020年1月-2022年1月期间蚌埠医学院第一附属医院重症医学科(ICU)收治的142例感染患者的临床资料,依据脓毒症3.0诊断标准将患者分为脓毒症组(86例)、非脓毒症组(56例)。单因素和多因素logistic回归分析确定脓毒症发生的危险因素。Spearman相关性分析NLR、MPR、CRP、PCT与SOFA评分以及APACHEⅡ评分的相关性,评估NLR、MPR、CRP、PCT与脓毒症病情严重程度的相关性;应用受试者工作特征曲线(ROC),评估NLR、MPR、CRP、PCT对脓毒症辅助诊断价值。结果 脓毒症组与非脓毒症组相比,NLR、MPR、CRP、PCT、APACHEⅡ评分、SOFA评分、病死率均明显升高,差异均具有统计学意义(均P < 0.05)。相关性分析显示:NLR、MPR、CRP、PCT与SOFA评分均呈强相关,其中以PCT与SOFA评分相关性最强,NLR、MPR、CRP、PCT与APACHEⅡ评分相关性较弱,NLR与APACHEⅡ评分中等强度相关。logistic回归分析结果表明NLR、MPR、CRP、PCT是脓毒症发生的危险因素。ROC曲线显示,NLR、MPR、CRP、PCT、NLR+MPR对脓毒症均有一定诊断价值(ROC曲线下面积分别为0.83、0.80、0.81、0.86,95%CI分别为0.76~0.90、0.73~0.87、0.73~0.88、0.80~0.92、0.80~0.93),其中以PCT和NLR+MPR诊断效能最高,当NLR=临界值13.05时,其敏感度和特异度分别为74.7%和82.1%,高于PCT=临界值0.81 μg/L时的特异度和CRP=临界值116.75 mg/L时的敏感度。结论 NLR、MPR可以作为脓毒症的辅助诊断的生物指标,NLR、MPR联合检测在识别脓毒症及其严重程度方面具有较高临床价值。
-
关键词:
- 脓毒症 /
- 中性粒细胞/淋巴细胞比值 /
- 平均血小板体积/血小板计数比值 /
- 辅助诊断 /
- 病情评估
Abstract: Objective To investigate the value of neutrophils/lymphocyte ratio (NLR) combined with mean platelet volume-to-platelet count ratio(MPR) in the auxiliary diagnosis and disease evaluation of patients with sepsis.Methods The clinical data of 142 infected patients admitted to the Critical Care Department of Medicine(ICU) of the First Affiliated Hospital of Bengbu Medical College from January 2020 to January 2020 were retrospectively analyzed, and the patients were divided into sepsis(86) and non-sepsis(56) according to the diagnostic criteria of sepsis 3.0. Univariate and multivariate logistic regression analysis were used to identify the risk factors for the development of sepsis. Spearman correlation analyzed the correlation of NLR, MPR, CRP, PCT and SOFA score and APACHEⅡ score, evaluated the correlation of NLR, MPR, CRP, PCT and sepsis severity. Receiver operating characteristic curve (ROC) was applied to evaluate the auxiliary diagnosis value of NLR, MPR, CRP and PCT for sepsis.Results Compared with the non-sepsis group, NLR, MPR, CRP, PCT, APACHEⅡ score, SOFA score, and mortality were significantly increased in the sepsis group, with statistical significance (all P < 0.05). Correlation analysis showed that NLR, MPR, CRP and PCT were all strongly correlated with SOFA score, among which PCT was the most strongly correlated with SOFA score, NLR, MPR, CRP and PCT were weakly correlated with APACHEⅡ score, and NLR was moderately associated with APACHEⅡ score. logistic regression analysis showed that NLR, MPR, CRP and PCT were independent risk factors for sepsis. ROC curve showed that NLR, MPR, CRP, PCT and NLR+MPR all had certain diagnostic value for sepsis. The areas under ROC curve were 0.83, 0.80, 0.81 and 0.86, respectively. 95%CI was 0.76-0.90, 0.73-0.87, 0.73-0.88, 0.80-0.92, 0.80-0.93}, respectively. PCT and NLR+MPR had the highest diagnostic efficacy. When NLR=critical value 13.05, the sensitivity and specificity were 74.7% and 82.1%, respectively, which were higher than those when the critical value of CRP=116.75 mg/L.Conclusion NLR and MPR can be used as biological indicators for the auxiliary diagnosis of sepsis, and the combination detection of NLR and MPR has high clinical value in identifying sepsis and its severity. -

-
表 1 两组患者一般资料比较
x±S 组别 性别/例 年龄/岁 病死率/% 男 女 非脓毒症组 30 26 65.71±14.13 14.3 脓毒症组 53 33 62.93±15.61 44.2 χ2/t 0.910 1.08 13.85 P 0.341 0.28 < 0.01 表 2 两组患者间实验室指标及严重程度评分比较
M(QL,QU), x±S 项目 非脓毒症组(56例) 脓毒症组(86例) U/t P NLR 8.13(6.49,12.29) 18.26(12.72,28.52) 6.69 < 0.01 MPR 0.04(0.03,0.06) 0.08(0.05,0.14) 5.35 < 0.01 CRP/(mg·L-1) 42.43(25.32,59.72) 183.50(59.18,217.00) 6.14 < 0.01 PCT/(ng·mL-1) 0.39(0.18,1.10) 6.54(1.88,22.24) 7.15 < 0.01 SOFA/分 5(3,6) 6(4,9) 3.39 < 0.01 APACHEⅡ/分 18.05±5.58 22.36±6.35 4.14 < 0.01 表 3 脓毒症患者实验室指标与SOFA评分以及APACHEⅡ评分的相关性分析
指标 SOFA评分 APACHEⅡ评分 r P r P NLR 0.60 < 0.01 0.41 < 0.01 MPR 0.62 < 0.01 0.33 < 0.01 CRP 0.57 < 0.01 0.31 < 0.01 PCT 0.68 < 0.01 0.32 < 0.01 表 4 Logistic回归分析脓毒症发生的危险因素
指标 β OR 95%CI P NLR 0.134 1.144 1.09~1.21 < 0.01 CRP 0.017 1.017 1.01~1.02 < 0.01 PCT 0.640 1.189 1.39~2.59 < 0.01 表 5 实验室指标对脓毒症的辅助诊断价值
指标 临界值 敏感度/% 特异度/% AUC 95%CI P NLR 13.05 74.7 82.1 0.84 0.77~0.91 < 0.01 MPR 0.05 71.1 71.4 0.76 0.68~0.84 < 0.01 CRP 116.75 61.6 91.1 0.80 0.73~0.88 < 0.01 PCT 0.81 86.0 69.6 0.86 0.80~0.92 < 0.01 PCT+MPR 0.49 85.5 78.6 0.86 0.80~0.93 < 0.01 -
[1] Irving SY, Daly B, Verger J, et al. The Association of Nutrition Status Expressed as Body Mass Index z Score With Outcomes in Children With Severe Sepsis: A Secondary Analysis From the Sepsis Prevalence, Outcomes, and Therapies(SPROUT)Study[J]. Crit Care Med, 2018, 46(11): e1029-e1039. doi: 10.1097/CCM.0000000000003351
[2] Thakkar RK, Weiss SL, Fitzgerald JC, et al. Risk Factors for Mortality in Pediatric Postsurgical versus Medical Severe Sepsis[J]. J Surg Res, 2019, 242: 100-110. doi: 10.1016/j.jss.2019.04.011
[3] Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021[J]. Intensive Care Med, 2021, 47(11): 1181-1247. doi: 10.1007/s00134-021-06506-y
[4] Kim HI, Park S. Sepsis: Early Recognition and Optimized Treatment[J]. Tuberc Respir Dis(Seoul), 2019, 82(1): 6-14. doi: 10.4046/trd.2018.0041
[5] Kaushik R, Gupta M, Sharma M, et al. Diagnostic and Prognostic Role of Neutrophil-to-Lymphocyte Ratio in Early and Late Phase of Sepsis[J]. Indian J Crit Care Med, 2018, 22(9): 660-663. doi: 10.4103/ijccm.IJCCM_59_18
[6] Dewitte A, Lepreux S, Villeneuve J, et al. Blood platelets and sepsis pathophysiology: A new therapeutic prospect in critically[corrected]ill patients?[J]. Ann Intensive Care, 2017, 7(1): 115. doi: 10.1186/s13613-017-0337-7
[7] Oh GH, Chung SP, Park YS, et al. Mean Platelet Volume to Platelet Count Ratio as a Promising Predictor of Early Mortality in Severe Sepsis[J]. Shock, 2017, 47(3): 323-330. doi: 10.1097/SHK.0000000000000718
[8] Seymour CW, Liu VX, Iwashyna TJ, et al. Assessment of Clinical Criteria for Sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock(Sepsis-3)[J]. JAMA, 2016, 315(8): 762-774. doi: 10.1001/jama.2016.0288
[9] Djordjevic D, Rondovic G, Surbatovic M, et al. Neutrophil-to-Lymphocyte Ratio, Monocyte-to-Lymphocyte Ratio, Platelet-to-Lymphocyte Ratio, and Mean Platelet Volume-to-Platelet Count Ratio as Biomarkers in Critically Ill and Injured Patients: Which Ratio to Choose to Predict Outcome and Nature of Bacteremia?[J]. Mediators Inflamm, 2018, 15(7): 3758068.
[10] Flores-Mejía LA, Cabrera-Rivera GL, Ferat-Osorio E, et al. Function is Dissociated From Activation-Related Immunophenotype on Phagocytes From Patients With SIRS/Sepsis Syndrome[J]. Shock, 2019, 52(5): e68-e75. doi: 10.1097/SHK.0000000000001314
[11] Sun R, Huang J, Yang Y, et al. Dysfunction of low-density neutrophils in peripheral circulation in patients with sepsis[J]. Sci Rep, 2022, 12(1): 685. doi: 10.1038/s41598-021-04682-x
[12] van der Poll T, van de Veerdonk FL, Scicluna BP, et al. The immunopathology of sepsis and potential therapeutic targets[J]. Nat Rev Immunol, 2017, 17(7): 407-420. doi: 10.1038/nri.2017.36
[13] Liang H, Gao Y, Miao C, et al. [Predictive value of neutrophil to lymphocyte ratio on 28-day mortality of patients with severe pneumonia][J]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue, 2019, 31(7): 827-831.
[14] Liu Y, Zheng J, Zhang D, et al. Neutrophil-lymphocyte ratio and plasma lactate predict 28-day mortality in patients with sepsis[J]. J Clin Lab Anal, 2019, 33(7): e22942.
[15] Inci K, Kalin B S, Türkoglu, Melda, et al. Prognostic Value of Red Cell Distribution Width and Neutrophil-Lymphocyte Ratio on Admission in Critically Ill Patients: A Retrospective Cohort Study[J]. Egyptian J Crit Care Med, 2020, 7(2): 92-97.
[16] Kocaturk O, Besli F, Gungoren F, et al. The relationship among neutrophil to lymphocyte ratio, stroke territory, and 3-month mortality in patients with acute ischemic stroke[J]. Neurol Sci, 2019, 40(1): 139-146. doi: 10.1007/s10072-018-3604-y
[17] Zhao C, Wei Y, Chen D, et al. Prognostic value of an inflammatory biomarker-based clinical algorithm in septic patients in the emergency department: An observational study[J]. Int Immunopharmacol, 2020, 80: 106145. doi: 10.1016/j.intimp.2019.106145
[18] Liu J, Liu Y, Xiang P, et al. Neutrophil-to-lymphocyte ratio predicts critical illness patients with 2019 coronavirus disease in the early stage[J]. J Transl Med, 2020, 18(1): 206. doi: 10.1186/s12967-020-02374-0
[19] 王卿语, 陈新军, 武冬, 等. 中性粒细胞与淋巴细胞比值及红细胞分布宽度对脓毒症患者预后评估价值性[J]. 临床急诊杂志, 2021, 22(2): 136-140. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202102013.htm
[20] 梁欢, 苗常青, 吴梦茹, 等. 中性粒细胞与淋巴细胞比值对脓毒性休克患者28 d死亡风险的预测价值评估[J]. 临床急诊杂志, 2019, 20(7): 503-508. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC201907001.htm
[21] Oh GH, Chung SP, Park YS, et al. Mean Platelet Volume to Platelet Count Ratio as a Promising Predictor of Early Mortality in Severe Sepsis[J]. Shock, 2017, 47(3): 323-330. doi: 10.1097/SHK.0000000000000718
[22] 郑印, 郭小丹, 张正阳. 血小板参数与老年脓毒症病情严重程度的关系及对短期预后的预测作用[J]. 临床急诊杂志, 2020, 21(4): 271-276, 281. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202004003.htm
[23] Zhu MY, Sun LQ. Ulcerative colitis complicated with colonic necrosis, septic shock and venous thromboembolism: A case report[J]. World J Clin Cases, 2019, 7(16): 2360-2366. doi: 10.12998/wjcc.v7.i16.2360
[24] 朱明玉, 孙立群. 中性粒细胞/血小板计数比值及平均血小板体积/血小板计数比值对老年脓毒症患者预后的评估价值[J]. 中华老年多器官疾病杂志, 2021, 20(2): 108-112. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLQG202102007.htm
[25] Dewitte A, Lepreux S, Villeneuve J, et al. Blood platelets and sepsis pathophysiology: A new therapeutic prospect in critically[corrected]ill patients?[J]. Ann Intensive Care, 2017, 7(1): 115. doi: 10.1186/s13613-017-0337-7
[26] Iba T, Levy JH, Warkentin TE, et al. Diagnosis and management of sepsis-induced coagulopathy and disseminated intravascular coagulation[J]. J Thromb Haemost, 2019, 17(11): 1989-1994. doi: 10.1111/jth.14578
[27] Xu X, Wang H, Wu X, et al. Risk factors of early septic shock-related thrombocytopenia and its impact on prognosis[J]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue, 2021, 33(8): 938-943.
[28] Vardon-Bounes F, Gratacap MP, Groyer S, et al. Kinetics of mean platelet volume predicts mortality in patients with septic shock[J]. PLoS One, 2019, 14(10): e0223553. doi: 10.1371/journal.pone.0223553
[29] Cho SY, Lee HJ, Kim JW, et al. Mean platelet volume and mean platelet volume/platelet count ratio in patients with chronic alcohol consumption[J]. Platelets, 2015, 26(4): 371-372. doi: 10.3109/09537104.2014.887200
[30] Guclu E, Durmaz Y, Karabay O. Effect of severe sepsis on platelet count and their indices[J]. Afr Health Sci, 2013, 13(2): 333-338.
[31] Cai N, Chen ZQ, Tao M, et al. Mean platelet volume and red blood cell distribution width is associated with prognosis in premature neonates with sepsis[J]. Open Med(Wars), 2021, 16(1): 1175-1181. doi: 10.1515/med-2021-0323
[32] Omran A, Sobh H, Abdalla MO, et al. Salivary and Serum Interleukin-10, C-Reactive Protein, Mean Platelet Volume, and CRP/MPV Ratio in the Diagnosis of Late-Onset Neonatal Sepsis in Full-Term Neonates[J]. J Immunol Res, 2021, 12(10): 4884537.
[33] Vélez-Páez JL, Legua P, Vélez-Páez P, et al. Mean platelet volume and mean platelet volume to platelet count ratio as predictors of severity and mortality in sepsis[J]. PLoS One, 2022;17(1): 232-236.
[34] Engelbrecht M, Atkinson B, Goddard A, et al. Mean Platelet Volume and Platelet Volume Distribution Width in Canine Parvoviral Enteritis[J]. Front Vet Sci, 2021, 8: 722280. doi: 10.3389/fvets.2021.722280
[35] Hanaganahalli SB, Sreeram S, Bompada M, et al. Is MPV a Predictive Marker for Neonatal Sepsis? A Pilot Study[J]. J Pediatr Hematol Oncol, 2018, 40(7): 548-552. doi: 10.1097/MPH.0000000000001272
[36] Orak M, Karakoç Y, Ustundag M, et al. An investigation of the effects of the mean platelet volume, platelet distribution width, platelet/lymphocyte ratio, and platelet counts on mortality in patents with sepsis who applied to the emergency department[J]. Niger J Clin Pract, 2018, 21(5): 667-671. doi: 10.4103/njcp.njcp_44_17
-




 下载:
下载: