Predictive value of serological indexes in patients with multiple trauma complicated with acute gastrointestinal function injury
-
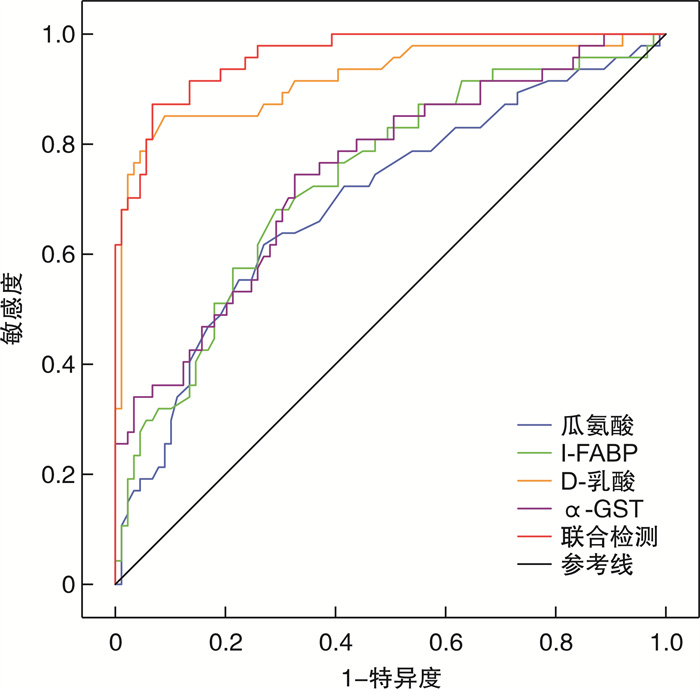
摘要: 目的 探讨血清瓜氨酸、肠型脂肪酸结合蛋白(Ⅰ-FABP)、D-乳酸、α-谷胱甘肽S转移酶(α-GST)等指标对多发伤并发急性胃肠功能损伤(AGFI)的预测价值。方法 回顾性分析陕西省人民医院急诊外科于2019年8月-2021年8月期间收治的多发伤患者136例,根据是否合并AGFI分为多发伤未并发AGFI组(N-AGFI组,89例)和多发伤并发AGFI组(AGFI组,47例)。收集并对比两组年龄、既往史等一般资料,以及血常规、生化指标、C反应蛋白(CPR)、降钙素原(PCT)、凝血功能、瓜氨酸、Ⅰ-FABP、D-乳酸、α-GST等指标的差异。应用二元logistics回归分析多发伤并发AGFI的影响因素,随后绘制ROC曲线分析各指标对多发伤并发AGFI的预测价值。结果 AGFI组患者年龄以及血清PCT、Ⅰ-FABP、D-乳酸、α-GST水平均显著高于N-AGFI组,而瓜氨酸水平则显著低于N-AGFI组,差异均有统计学意义(P < 0.05)。二元logistics回归分析结果显示血清瓜氨酸、Ⅰ-FABP、D-乳酸、α-GST水平是多发伤合并AGFI的独立影响因素(P < 0.05)。由ROC曲线可见,血清瓜氨酸、Ⅰ-FABP、D-乳酸、α-GST水平及联合检测均可用于预测多发伤并发AGFI,其AUC分别为0.696、0.734、0.919、0.748、0.960,其中联合检测的AUC最高,其预测多发伤并发AGFI的敏感度和特异度分别为87.23%、93.26%。结论 血清瓜氨酸、Ⅰ-FABP、D-乳酸、α-GST水平对多发伤患者并发AGFI具有较好的预测价值,四项指标联合预测的效果更佳。Abstract: Objective To explore the predictive value of serum indexes such as citrulline, intestinal fatty acid binding protein(Ⅰ-FABP), D-lactate and α-glutathione S-transferase(α-GST) in patients with multiple trauma complicated with acute gastrointestinal function injury(AGFI).Methods The medical records of 136 patients with multiple trauma treated in Shaanxi Provincial People's Hospital from August 2019 to August 2021 were analyzed retrospectively. According to whether they were complicated with AGFI, they were divided into multiple trauma without AGFI group(N-AGFI group) and multiple trauma with AGFI group(AGFI group). The general data such as age, past history and other indicators as well as blood routine, biochemical indexes, CPR, coagulation function, citrulline, Ⅰ-FABP, D-lactate and α-GST were collected and compared between the two groups. Binary logistic regression was used to analyze the influencing factors of multiple trauma complicated with AGFI, and then ROC curve was drawn to analyze the predictive value of each index to multiple trauma complicated with AGFI.Results The age and serum levels of PCT, Ⅰ-FABP, D-lactate and α-GST in AGFI group were significantly higher than those in N-AGFI group, while the level of citrulline was significantly lower than that in N-AGFI group, the differences were statistically significant(P < 0.05). The results of binary logistic regression analysis showed that the levels of serum citrulline, Ⅰ-FABP, D-lactate and α-GST were independent influencing factors of multiple trauma complicated with AGFI(P < 0.05). ROC curve showed that the levels of serum citrulline, Ⅰ-FABP, D-lactate, α-GST and combined detection can be used to predict multiple trauma complicated with AGFI, with AUC of 0.696, 0.734, 0.919, 0.748 and 0.960 respectively. The AUC of combined detection is the highest, and the sensitivity and specificity for predicting multiple trauma complicated with AGFI are 87.23% and 93.26% respectively.Conclusion The levels of serum citrulline, Ⅰ-FABP, D-lactate and α-GST have good predictive value for AGFI in patients with multiple trauma, and the combined prediction of the four has better predictive value.
-

-
表 1 两组患者一般资料比较
例(%),x±S 一般资料 N-AGFI组(89例) AGFI组(47例) t/χ2 P 年龄/岁 39.26±9.37 42.79±10.75 -1.984 0.049 性别 男 68(76.40) 35(74.47) 0.063 0.802 女 21(23.60) 12(25.53) 既往史 高血压 22(27.72) 12(25.53) 0.011 0.917 糖尿病 9(10.11) 7(14.89) 0.677 0.411 冠心病 13(14.61) 9(19.15) 0.468 0.494 慢性肺部疾病 7(7.87) 3(6.38) 0.001 0.976 病因 交通事故 64(71.91) 32(68.09) 高处坠落 16(17.98) 7(14.89) 2.022 0.568 挤压伤 4(4.49) 5(10.64) 其他 5(5.62) 3(6.38) APACHEⅡ评分/分 8.12±3.03 9.13±3.29 -1.783 0.077 表 2 两组患者实验室检查指标比较
指标 N-AGFI组(89例) AGFI组(47例) t P WBC/(×109·L-1) 10.12±2.74 10.76±3.03 -1.236 0.219 PLT/(×109·L-1) 164.40±35.95 151.62±41.48 1.869 0.064 Hb/(g·L-1) 96.82±16.08 95.11±18.62 0.559 0.577 谷草转氨酶/(U·L-1) 60.34±9.91 62.47±10.27 -1.178 0.241 谷丙转氨酶/(U·L-1) 69.30±13.76 69.11±15.58 0.076 0.940 白蛋白/(g·L-1) 38.79±5.89 36.79±5.96 1.872 0.063 前蛋白/(mg·L-1) 316.11±51.34 299.81±51.52 1.759 0.081 随机血糖/(mmol·L-1) 8.10±1.87 7.94±1.60 0.501 0.617 TC/(mmol·L-1) 5.42±0.85 5.37±1.05 0.296 0.767 LDL-C/(mmol·L-1) 3.18±0.77 3.11±0.84 0.486 0.628 血肌酐/(μmol·L-1) 122.08±20.39 130.36±26.07 -1.880 0.062 血尿酸/(μmol·L-1) 286.36±67.93 285.49±67.11 0.071 0.943 CPR/(mg·L-1) 18.42±6.36 20.54±6.08 -1.873 0.063 PCT/(ng·mL-1) 2.05±0.70 2.31±0.76 -1.991 0.049 D-二聚体/(μg·mL-1) 14.58±5.55 16.23±5.58 -1.642 0.103 APTT时间/s 34.40±5.28 35.77±4.10 -1.550 0.123 瓜氨酸/(μmol·L-1) 18.93±4.02 16.26±4.26 3.614 < 0.001 Ⅰ-FABP/(μg·L-1) 1.56±0.46 1.97±0.48 -4.820 < 0.001 D-乳酸/(mg·L-1) 2.66±0.56 4.14±0.88 -9.121 < 0.001 α-GST/(U·L-1) 14.97±4.91 20.35±6.23 -5.528 < 0.001 表 3 多发伤并发AGFI的多因素logistic分析
因素 β SE Wals χ2 P Exp(B) 95%CI 年龄 -0.862 0.709 1.478 0.224 0.422 0.105~1.695 PCT 0.133 0.438 0.093 0.761 1.143 0.484~2.697 瓜氨酸 -0.153 0.074 4.247 0.039 0.858 0.742~0.993 Ⅰ-FABP 1.529 0.718 4.536 0.033 4.613 1.130~18.836 D-乳酸 3.123 0.675 21.427 < 0.001 22.718 6.054~85.247 α-GST 0.179 0.066 7.283 0.007 1.196 1.050~1.361 常量 -13.734 3.256 17.787 < 0.001 0.000 注:Hosmer-Lemeshow检验,χ2=3.622,P=0.890;模型检验,χ2=112.734,P < 0.001。 表 4 各指标预测多发伤并发AGFI的效能分析
指标 AUC SE P 95% CI Cut off 敏感度/% 特异度/% 瓜氨酸 0.696 0.049 < 0.001 0.601~0.792 16.75 61.70 74.16 Ⅰ-FABP 0.734 0.045 < 0.001 0.645~0.824 1.78 68.09 70.79 D-乳酸 0.9191)2) 0.028 < 0.001 0.864~0.975 3.34 85.11 91.01 α-GST 0.7483) 0.044 < 0.001 0.661~0.835 16.91 74.47 67.42 联合检测 0.9601)2)3)4) 0.015 < 0.001 0.932~0.989 0.4075 87.23 93.26 与瓜氨酸比较,1)P < 0.05;与Ⅰ-FABP比较,2)P < 0.05;与D-乳酸比较,3)P < 0.05;与α-GST比较,4)P < 0.05。 -
[1] Relja B, Yang B, Bundkirchen K, et al. Different experimental multiple trauma models induce comparable inflammation and organ injury[J]. Sci Rep, 2020, 10(1): 20185. doi: 10.1038/s41598-020-76499-z
[2] Liu H, Xiao X, Sun C, et al. Systemic inflammation and multiple organ injury in traumatic hemorrhagic shock[J]. Front Biosci(Landmark Ed), 2015, 20(6): 927-933. doi: 10.2741/4347
[3] 陈福进, 姚莉, 赵晶晶. 多发伤后急性胃肠损伤预测模型建立和评价[J]. 中国急救医学, 2021, 41(11): 972-976. doi: 10.3969/j.issn.1002-1949.2021.11.010
[4] 高亚萍, 苗云凤, 刘媛. 严重多发伤患者伤后肠道细菌移位与患者发生感染的关系[J]. 医学临床研究, 2020, 37(3): 450-452. doi: 10.3969/j.issn.1671-7171.2020.03.039
[5] 中华医学会创伤学分会创伤急救与多发伤学组. 多发伤病历与诊断: 专家共识意见(2013版)[J]. 创伤外科杂志, 2014, 16(2): 192, 封3. https://www.cnki.com.cn/Article/CJFDTOTAL-CXWK201402048.htm
[6] Reintam Blaser A, Malbrain ML, Starkopf J, et al. Gastrointestinal function in intensive care patients: terminology, definitions and management. Recommendations of the ESICM Working Group on Abdominal Problems[J]. Intensive Care Med, 2012, 38(3): 384-94. doi: 10.1007/s00134-011-2459-y
[7] Palmer CS, Cameron PA, Gabbe BJ. Comparison of revised Functional Capacity Index scores with Abbreviated Injury Scale 2008 scores in predicting 12-month severe trauma outcomes[J]. Inj Prev, 2020, 26(2): 138-146. doi: 10.1136/injuryprev-2018-043085
[8] 缪舜, 彭国宏, 韩萍. 多发伤并发多器官功能障碍综合征的临床特点及危险因素[J]. 中国急救复苏与灾害医学杂志, 2021, 16(3): 286-288, 307. doi: 10.3969/j.issn.1673-6966.2021.03.018
[9] 郭常敏, 宋睿, 黄强, 等. 急性创伤性出血和凝血障碍的诊断和治疗[J]. 临床急诊杂志, 2021, 22(7): 508-512.
[10] 刘刚, 王波, 唐小莹, 等. 严重多发伤家兔早期急性胃肠功能损伤分级与肠道微环境改变的相关性研究[J]. 中华创伤杂志, 2017, 33(10): 929-937. doi: 10.3760/cma.j.issn.1001-8050.2017.10.013
[11] 张聪, 邓海, 李镇文, 等. 严重多发伤后免疫紊乱与急性胃肠功能损伤间的关系[J]. 中华急诊医学杂志, 2021, 30(5): 537-541. doi: 10.3760/cma.j.issn.1671-0282.2021.05.005
[12] Maric S, Restin T, Muff JL, et al. Citrulline, Biomarker of Enterocyte Functional Mass and Dietary Supplement. Metabolism, Transport, and Current Evidence for Clinical Use[J]. Nutrients, 2021, 13(8): 2794. doi: 10.3390/nu13082794
[13] Gonzalez AM, Trexler ET. Effects of Citrulline Supplementation on Exercise Performance in Humans: A Review of the Current Literature[J]. J Strength Cond Res, 2020, 34(5): 1480-1495. doi: 10.1519/JSC.0000000000003426
[14] Kao CC, Bandi V, Guntupalli KK, et al. Arginine, citrulline and nitric oxide metabolism in sepsis[J]. Clin Sci(Lond), 2009, 117(1): 23-30. doi: 10.1042/CS20080444
[15] Padar M, Starkopf J, Starkopf L, et al. Enteral nutrition and dynamics of citrulline and intestinal fatty acid-binding protein in adult ICU patients[J]. Clin Nutr ESPEN, 2021, 45: 322-332. doi: 10.1016/j.clnesp.2021.07.026
[16] Teng J, Xiang L, Long H, et al. The Serum Citrulline and D-Lactate are Associated with Gastrointestinal Dysfunction and Failure in Critically Ill Patients[J]. Int J Gen Med, 2021, 14: 4125-4134. doi: 10.2147/IJGM.S305209
[17] Costa BP, Martins P, Verissimo C, et al. Intestinal dysfunction in the critical trauma patients-An early and frequent event[J]. Nutr Hosp, 2017, 34(2): 284-289. doi: 10.20960/nh.788
[18] Derikx JP, Schellekens DH, Acosta S. Serological markers for human intestinal ischemia: A systematic review[J]. Best Pract Res Clin Gastroenterol, 2017, 31(1): 69-74. doi: 10.1016/j.bpg.2017.01.004
[19] Sun DL, Cen YY, Li SM, et al. Accuracy of the serum intestinal fatty-acid-binding protein for diagnosis of acute intestinal ischemia: a meta-analysis[J]. Sci Rep, 2016, 6: 34371. doi: 10.1038/srep34371
[20] Zenger S, Demir Piroǧlu, Çevik A, et al. The importance of serum intestinal fatty acid-binding protein for the early diagnosis of acute mesenteric ischemia[J]. Ulus Travma Acil Cerrahi Derg, 2021, 27(3): 278-283.
[21] Wu C, Zhu X, Ren H, et al. Intestinal fatty acid-binding protein as a biomarker for the diagnosis of strangulated intestinal obstruction: A meta-analysis[J]. Open Med(Wars), 2021, 16(1): 264-273. doi: 10.1515/med-2021-0214
[22] Blaser A, Padar M, Tang J, et al. Citrulline and intestinal fatty acid-binding protein as biomarkers for gastrointestinal dysfunction in the critically ill[J]. Anaesthesiol Intensive Ther, 2019, 51(3): 230-239. doi: 10.5114/ait.2019.86049
[23] Voth M, Lustenberger T, Relja B, et al. Is Ⅰ-FABP not only a marker for the detection abdominal injury but also of hemorrhagic shock in severely injured trauma patients? [J]. World J Emerg Surg, 2019, 14: 49. doi: 10.1186/s13017-019-0267-9
[24] Piton G, Capellier G. Biomarkers of gut barrier failure in the ICU[J]. Curr Opin Crit Care, 2016, 22(2): 152-160.
[25] 王锐. 瓜氨酸、Ⅰ-FABP、内毒素及PCT与严重创伤后急性胃肠损伤的相关性研究[D]. 兰州: 兰州大学, 2017.
[26] Nielsen C, Kirkegard J, Erlandsen EJ, et al. D-lactate is a valid biomarker of intestinal ischemia induced by abdominal compartment syndrome[J]. J Surg Res, 2015, 194(2): 400-404. doi: 10.1016/j.jss.2014.10.057
[27] Sun XQ, Fu XB, Zhang R, et al. Relationship between plasma D(-)-lactate and intestinal damage after severe injuries in rats[J]. World J Gastroenterol, 2001, 7(4): 555-558. doi: 10.3748/wjg.v7.i4.555
[28] Liu L, Wen L, Gao C, et al. Effects of Non-directional Mechanical Trauma on Gastrointestinal Tract Injury in Rats[J]. Front Physiol, 2021, 12: 649554. doi: 10.3389/fphys.2021.649554
[29] Shi H, Wu B, Wan J, et al. The role of serum intestinal fatty acid binding protein levels and D-lactate levels in the diagnosis of acute intestinal ischemia[J]. Clin Res Hepatol Gastroenterol, 2015, 39(3): 373-378. doi: 10.1016/j.clinre.2014.12.005
[30] 张玮, 褚永果, 李伟, 等. 肠型脂肪酸结合蛋白和D-乳酸在危重症肠黏膜屏障功能的临床研究[J]. 临床急诊杂志, 2018, 19(1): 6-12.
[31] Li H, Chen Y, Huo F, et al. Association between acute gastrointestinal injury and biomarkers of intestinal barrier function in critically ill patients[J]. BMC Gastroenterol, 2017, 17(1): 45. doi: 10.1186/s12876-017-0603-z
[32] Treskes N, Persoon AM, van Zanten ARH. Diagnostic accuracy of novel serological biomarkers to detect acute mesenteric ischemia: a systematic review and meta-analysis[J]. Intern Emerg Med, 2017, 12(6): 821-836. doi: 10.1007/s11739-017-1668-y
[33] Kong C, Li SM, Yang H, et al. Screening and combining serum biomarkers to improve their diagnostic performance in the detection of intestinal barrier dysfunction in patients after major abdominal surgery[J]. Ann Transl Med, 2019, 7(16): 388. doi: 10.21037/atm.2019.07.102
[34] 王艳, 王建荣, 唐晟, 等. 危重患者急性胃肠损伤现状及影响因素的调查研究[J]. 国际消化病杂志, 2017, 37(1): 54-58. https://www.cnki.com.cn/Article/CJFDTOTAL-GWXH201701015.htm
[35] 潘春熹, 陈万, 吕立文, 等. 老年脓毒性休克患者急性胃肠道损伤超声表现及相关性研究[J]. 临床急诊杂志, 2020, 21(4): 261-266.
[36] 武娟, 孙雪莲, 李力卓. 急诊多发伤患者急性胃肠功能损伤的影响因素及相关防治措施[J]. 临床急诊杂志, 2021, 22(12): 814-819. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202112006.htm
-




 下载:
下载: