The value of a scoring system based on ultrasound imaging signs in predicting the severity of acute appendicitis
-
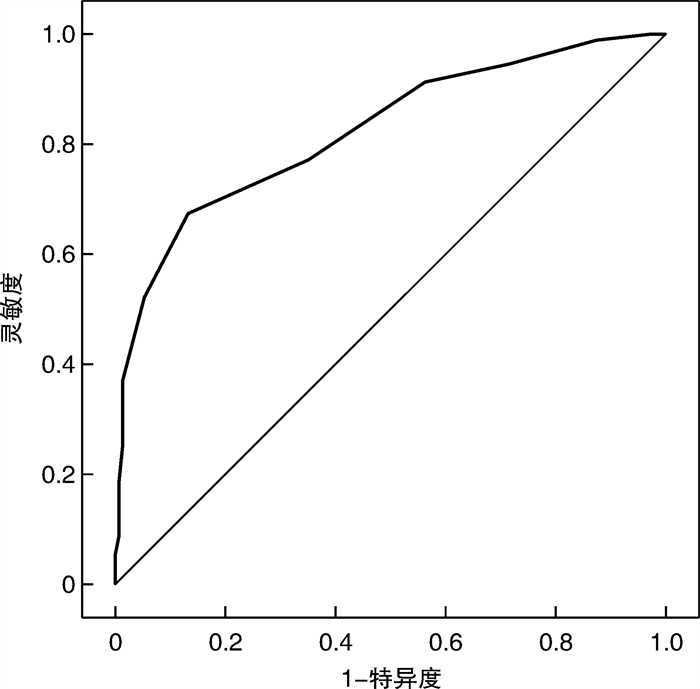
摘要: 目的 通过分析彩超下急性阑尾炎征象建立预测其严重程度的评分系统,并探究在临床上的应用价值。方法 根据急性阑尾炎术后病理结果分为非复杂性阑尾炎组(151例)和复杂性阑尾炎组(92例),通过单因素及多因素logistic回归分析复杂性阑尾炎的独立因素。然后对超声下各征象赋值进行评分,比较两组患者的得分,并绘制受试者工作特征(ROC)曲线,以探讨评分系统诊断复杂性急性阑尾炎的最佳得分值及其灵敏度与特异度。结果 复杂性阑尾炎的独立因素有管腔积液、界限不清、腹(盆)腔积液、肠系膜(网膜)增厚及回声增强、肠蠕动异常。急性阑尾炎严重程度评分共17分,非复杂性阑尾炎组评分为3.7(2.0,5.0)分,复杂性阑尾炎组为6.84(5.0,8.7)分,两组比较差异有统计学意义(P < 0.05)。曲线下面积AUC为0.824(95%CI:0.768~0.880,P < 0.001),最佳诊断截断值为5.5分,即评分≥6分诊断为复杂性阑尾炎,灵敏度为67.4%,特异度为86.8%。结论 重视超声下急性阑尾炎征象独立因素有助于复杂性阑尾炎的诊断,新建立的急性阑尾炎严重程度评分系统可指导临床病情评估。Abstract: Objective To establish a scoring system for predicting the severity of acute appendicitis by analyzing the signs of acute appendicitis under color ultrasound, and explore its clinical application value.Methods Acute appendicitis was divided into two groups: uncomplicated appendicitis group(151 cases) and complicated appendicitis group(92 cases). The independent factors of complicated appendicitis were analyzed by univariate and multivariate logistic regression. Then, each sign assigned under ultrasound was scored, the scores of the two groups were compared, and the receiver operating characteristic(ROC) curve was drawn to explore the best score value, sensitivity and specificity of the scoring system in diagnosing complex acute appendicitis.Results The independent factors of complex appendicitis were lumen effusion, unclear boundary, abdominal/pelvic effusion, mesentery/omental thickening and echo enhancement, and intestinal peristalsis. The severity score of acute appendicitis was 17 points, that of the non-complicated appendicitis group was 3.7(2.0, 5.0), and that of the complicated appendicitis group was 6.84(5.0, 8.7), and the difference between the two groups was statistically significant(P < 0.05). The AUC under the curve was 0.824(95%CI: 0.7688-0.880, P < 0.001), the best diagnostic cut-off point was 5.5 points, that is, the score ≥6 points was diagnosed as complex appendicitis, the sensitivity was 67.4%, and the specificity was 86.8%.Conclusion Paying attention to the independent factors of ultrasound signs of acute appendicitis is helpful for the diagnosis of complicated appendicitis. The newly established acute appendicitis severity scoring system can guide the clinical evaluation of the disease.
-
Key words:
- acute appendicitis /
- ultrasound examination /
- independent factor /
- scoring system
-

-
表 1 急性阑尾炎超声征象单因素比较分析
征象 非复杂型(151例) 复杂型(92例) Z/χ2 P 管径宽度/mm 9.7(8.0,11.0) 11.1(9.0,13.0) -3.614 < 0.001 管腔积液/例(%) 64(42.2) 55(59.8) 6.925 0.008 管腔粪石/例(%) 33(21.9) 33(35.5) 5.676 0.017 管壁血流增多/例(%) 47(31.1) 27(29.3) 0.085 0.770 脓肿形成/例(%) 0 3(1.2) 4.985 0.026 界限不清/例(%) 6(4.0) 31(33.7) 31.126 < 0.001 腹(盆)腔积液/例(%) 13(8.6) 36(39.1) 33.081 < 0.001 回(盲)肠壁增厚/例(%) 8(5.3) 21(22.8) 16.712 < 0.001 肠系膜(网膜)增厚、回声增强/例(%) 16(10.6) 25(27.2) 11.202 0.001 肠蠕动异常/例(%) 2(1.3) 27(29.3) 42.717 < 0.001 淋巴结肿大/例(%) 3(2.0) 5(5.4) 3.415 0.065 表 2 复杂性阑尾炎超声征象多因素的logistic回归分析
征象 B Wald χ2 P OR 95%CI 管腔积液 0.771 5.020 0.025 2.021 1.101~4.248 界限不清 2.125 15.693 < 0.001 12.281 2.925~23.945 腹(盆)腔积液 1.846 19.173 < 0.001 6.824 2.773~14.481 肠系膜(网膜)增厚、回声增强 1.118 6.279 0.012 3.148 1.276~7.336 肠蠕动异常 3.388 0.789 < 0.001 30.946 6.303~139.156 表 3 新建立的急性阑尾炎严重程度超声评分
超声表现 分值/分 管径宽度 ≤6.0 mm=0;6.0~9.4 mm=1;≥9.4 mm=2 管腔积液 无=0;有=2 管腔粪石 无=0;有=1 管壁血流 无=0;有=1 脓肿形成 无=0;有=1 界限 清=0;不清=2 腹(盆)腔积液 无=0;有=2 回(盲)肠壁增厚 无=0;有=1 肠系膜(网膜)增厚、回声增强 无=0;有=2 肠蠕动异常 无=0;有=2 淋巴结肿大 无=0;有=1 注:评分取超声表现结果累计得分,总分为17分。盲肠(回肠)壁增厚:≥2.0 mm;肠蠕动异常:蠕动增强指探及蠕动波>10次/min,蠕动减弱是指蠕动波 < 1次/min;淋巴结肿大:横径≥5.0 mm。 表 4 急性阑尾炎严重程度超声评分结果
例 分组 例数 评分/分 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 非复杂性阑尾炎 151 4 15 24 23 32 33 12 6 0 1 0 1 0 0 0 0 0 0 复杂性阑尾炎 92 0 1 4 3 13 9 14 14 11 6 9 3 0 4 0 1 0 0 合计 243 4 16 28 26 45 42 26 20 11 7 9 4 0 4 0 1 0 0 -
[1] 陈文君, 王亚萍, 张佩雯. 急诊成人急性阑尾炎患者腹部超声、CT平扫影像学特征及其诊断效果对比[J]. 中国CT和MRI杂志, 2022, 20(10): 126-127.
[2] 吴燕妮, 赵博厚, 陶思敏, 等. 人工智能在急性阑尾炎诊断中的研究进展[J]. 中国急救医学, 2022, 42(7): 631-634.
[3] Kim HY, Park JH, Lee Y J, et al. Systematic review and metaanalysis of CT features for differentiating complicated and uncomplicated appendicitis[J]. Radiology, 2018, 287(1): 104-115. doi: 10.1148/radiol.2017171260
[4] Bhangu A, Soreide K, Di Saverio S, et al. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management[J]. Lancet, 2015, 386(10000): 1278-1287. doi: 10.1016/S0140-6736(15)00275-5
[5] 念诗勇. 腹部彩超检查用于诊断急性阑尾炎的价值分析[J]. 现代医用影像学, 2023, 32(11): 2157-2159.
[6] 马天翼, 张骞, 赵宏伟, 等. 复杂性阑尾炎发病风险因素分析[J]. 中国现代普通外科进展, 2023, 26(3): 239-241.
[7] 罗建彬. 阑尾超声检查评分系统在成人急性阑尾炎诊断中的应用[J]. 中国医学影像学杂志, 2016, 24(8): 580-584.
[8] 陈伟纲, 韦巧萍, 尤宇晴. 多层螺旋CT与腹部超声在小儿急性阑尾炎临床诊断中的应用[J]. 中国基层医药, 2022, 29(4): 517-520.
[9] 占一姗, 朱友荣, 张守华, 等. 急性阑尾炎相关诊断预测模型的研究进展[J]. 中华普通外科学文献(电子版), 2023, 17(2): 151-154.
[10] 冯丽颖, 刘文飞, 董翼, 等. 临床评分系统在急性阑尾炎诊断中的应用研究进展[J]. 广西医学, 2023, 45(3): 342-345, 350.
[11] 张博诚, 王连臣. 成人复杂性阑尾炎临床预测评分模型的建立与验证[J]. 临床急诊杂志, 2020, 21(8): 608-614. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2020.08.002
[12] 丁姣姣, 高军喜, 孙艳, 等. 超声直接征象与间接征象诊断急性阑尾炎单因素及多因素分析[J]. 中国超声医学杂志, 2014, 30(8): 719-722.
[13] 毕世玥, 王玉, 熊晓苓, 等. 超声对儿童急性阑尾炎的诊断价值[J]. 临床超声医学杂志, 2023, 25(12): 986-989.
[14] 焦健, 都基权, 孟玫, 等. 超声检查在经CT检查未确诊疑似急性阑尾炎诊断中的应用[J]. 山东医药, 2020, 60(18): 89-91.
[15] 路婧, 黎新艳, 杨水华, 等. 超声征象诊断儿童急性阑尾炎合并穿孔的价值[J]. 广西医学, 2022, 44(9): 947-950.
[16] 孙健玮, 闫楠, 丁丁, 等. 彩色多普勒超声诊断复杂性阑尾炎的临床应用[J]. 影像研究与医学应用, 2019, 3(4): 201-203.
[17] 张龙方, 陈英, 丁蔓妮, 等. 老年急性阑尾炎病情严重程度的超声评估及其临床应用[J]. 中华老年多器官疾病杂志, 2022, 21(3): 180-183.
[18] 曹欢, 陈焕庭, 潘丽, 等. 伴有感染休克的急性阑尾炎临床特点及其预后研究[J]. 国际医药卫生导报, 2022, 28(1): 106-109.
[19] 郭悦, 朱晓旭, 韩煦. 急性阑尾炎B型超声、MSCT检查影像学表现及临床诊治价值对比[J]. 中国CT和MRI杂志, 2022, 20(2): 143-145.
[20] 刘晏佐, 王晓霞, 郭海峰. B超诊断急性阑尾炎疾病的研究进展[J]. 影像研究与医学应用, 2018, 2(1): 3-4.
[21] 姚秀芬, 赵妮, 延艳娜. 高频超声联合临床Alvarado评分在降低阑尾炎误漏诊率中的价值[J]. 临床急诊杂志, 2017, 18(1): 51-54. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2017.01.015
[22] Stringer MD. Acute appendicitis[J]. J Paediatr Child Health, 2017, 53(11): 1071-1076.
[23] 金丽虹, 张林娟, 於林军, 等. 台州地区穿孔性阑尾炎患儿流行病学调查及相关影响因素分析[J]. 中国医药导报, 2023, 20(12): 60-63, 69.
-




 下载:
下载: