The timing and failure factors of endoscopic treatment in patients with non-varicose upper gastrointestinal bleeding
-
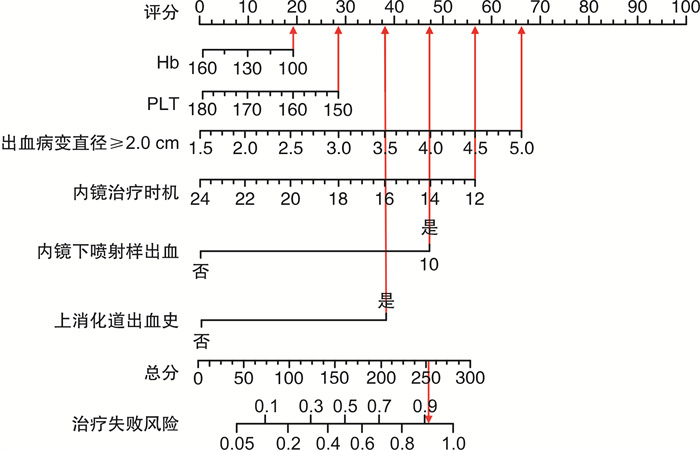
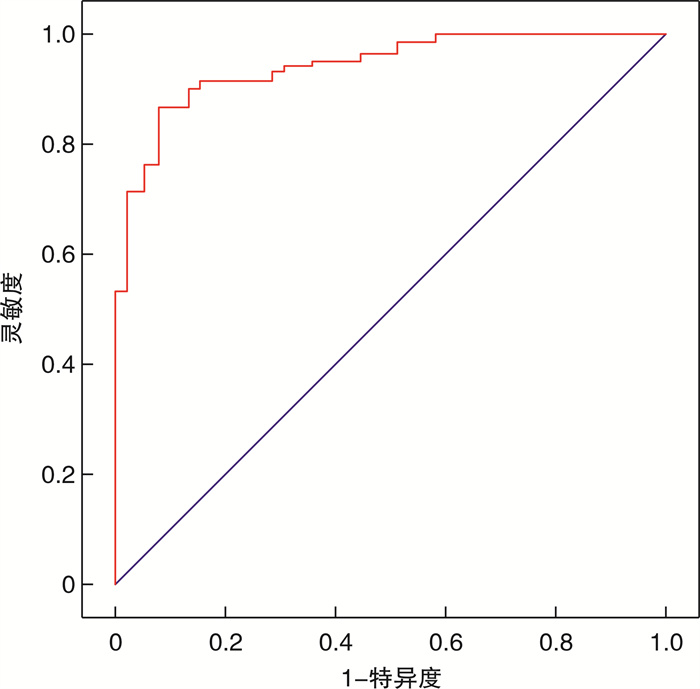
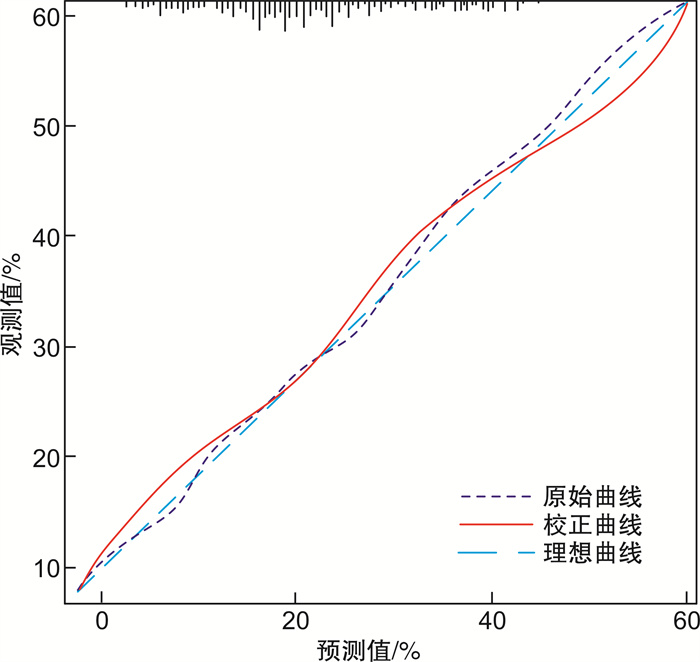
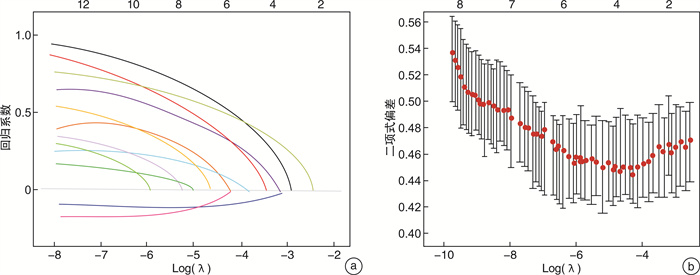
摘要: 目的 分析探讨非静脉曲张性上消化道出血患者内镜治疗时机的选择以及治疗失败的因素。 方法 选取连云港市第一人民医院2021年5月—2023年5月收治的340例非静脉曲张性上消化道出血患者作为研究对象,根据患者接受治疗的时间不同,将其分为3组:紧急组(治疗时间 < 12 h,100例),早期组(12 h≤治疗时间≤24 h,120例),延迟组(治疗时间>24 h,120例);根据术后情况将患者分为两组:成功止血的患者归为成功组(272例),术后再次出血、转入ICU、30 d后再入院以及院内死亡的患者归为失败组(68例)。采用LASSO回归分析法和logistic回归分析法进行内镜治疗失败的多因素分析,R软件构建治疗失败风险的预测模型,采用Bootstrap方法对该模型进行验证。 结果 成功组和失败组患者以及组内各亚组(紧急组、早期组、延迟组)之间,在血红蛋白(haemoglobin,Hb)、血清尿素氮(blood urea nitrogen,BUN)、血小板(blood platelet,PLT)、美国麻醉医师协会(American Society of Anesthesiologists, ASA)分级>Ⅱ、出血病变直径≥2.0 cm、内镜下喷射样出血、内镜治疗时机、住院时间、术中出血量、输血、输血量、上消化道出血史指标方面差异有统计学意义(P<0.05)。进行治疗后,紧急组患者在收缩压 < 90 mmHg(1 mmHg=0.133 kPa)、AIMS65评分、国际标准化比值(international normalized ratio, INR)、Hb、BUN、PLT指标方便均高于其他两组,差异有统计学意义(P<0.05),且早期组患者的各项指标更趋于正常值,治疗效果最佳。LASSO以及logistic回归分析可得,PLT、Hb和内镜治疗时机、上消化道出血史、出血病变直径≥2.0 cm、内镜下喷射样出血是内镜治疗失败的独立危险因素。联合以上5个因素构建的列线图模型,曲线下面积为0.905,灵敏度为92.2%,特异度为86.7%。校准曲线显示验证前后模型的预测概率与参考概率拟合度良好,Hosmer-Lemeshow检验结果差异无统计学意义(P>0.05),具有良好的预测精准度。 结论 患者内镜治疗的时间在12~24 h内效果较好。PLT、Hb、12 h≤内镜治疗时机≤24 h是内镜治疗失败的保护因素,具有上消化道出血史、出血病变直径≥2.0 cm、内镜下喷射样出血是内镜治疗失败的独立危险因素,临床上应密切关注。
-
关键词:
- 非静脉曲张性上消化道出血 /
- 内镜治疗 /
- 治疗时机 /
- 危险因素
Abstract: Objective To analyze the timing and failure factors of endoscopic treatment in patients with non-varicose upper gastrointestinal hemorrhage. Methods Three hunred and forty patients with non-varicose upper gastrointestinal bleeding admitted to our hospital from May 2021 to May 2023 were divided into three groups according to the different time of treatment: The general data and postoperative indexes of patients in the emergency group(treatment time < 12 h, n=100), the early group(12 h≤treatment time≤24 h, n=120) and the delayed group(treatment time>24 h, n=120) were compared. Patients were then divided into two groups according to postoperative conditions. Patients with successful hemostasis were classified as successful group(n=272), and patients with postoperative rebleeding, transfer to ICU, re-admission 30 days later, and in-hospital death were classified as failure group(n=68). LASSO regression analysis and logistic regression analysis were used to conduct multi-factor analysis of endoscopic treatment failure. R software built a prediction model of treatment failure risk, and Bootstrap method was used to verify the model. Results There were statistically significant differences(P < 0.05) in blood platelet(PLT), haemoglobin(Hb), blood urea nitrogen(BUN), American Society of Anesthesiologists(ASA)>Ⅱ, bleeding lesion diameter ≥ 2.0 cm, endoscopic jet like bleeding, endoscopic treatment timing, length of hospital stay, intraoperative bleeding volume, blood transfusion, blood transfusion volume, and history of upper gastrointestinal bleeding between the successful and failed groups, as well as among various subgroups within the group(emergency group, early group, delayed group). After treatment, systolic blood pressure < 90 mmHg(1 mmHg=0.133 kPa), AIMS65 score, INR, Hb, BUN and PLT indexes in the emergency group were higher than those in the other two groups, with statistical significance(P < 0.05). In addition, patients in the early group had more normal indicators, indicating the best treatment effect. LASSO and logistic regression analysis showed that PLT, Hb and endoscopic treatment timing, upper gastrointestinal bleeding history, bleeding lesion diameter ≥2.0 cm, and endoscopic jet bleeding were independent risk factors for endoscopic treatment failure. The area under curve, sensitivity and specificity of the nomogram model combined with the above 5 factors were 0.905, 92.2% and 86.7% respectively. The calibration curve showed that the prediction probability and reference probability of the model before and after verification had a good fit, and there was no statistical significance between the Hosmer-Lemeshow test results(P>0.05), indicating a good prediction accuracy. Conclusion Endoscopic therapy is best performed within 12 to 24 hours. PLT, Hb and 12 h≤endoscopic treatment time≤24 h were protective factor for endoscopic treatment failure. History of upper gastrointestinal bleeding, bleeding lesion diameter ≥2.0 cm, and endoscopic jet bleeding are independent risk factors for endoscopic treatment failure, which should be closely monitored clinically. -

-
表 1 基线资料比较
项目 成功组(272例) 失败组(68例) t/χ2 P 紧急组(66例) 早期组(110例) 延迟组(96例) F P 紧急组(34例) 早期组(10例) 延迟组(24例) F P 性别/例(%) 1.105 0.576 5.399 0.067 0.222 0.638 男 36(54.55) 67(60.91) 60(62.50) 24(70.59) 3(30.00) 15(62.50) 女 30(45.45) 43(39.09) 36(37.50) 10(29.41) 7(70.00) 9(37.50) 年龄/岁 65.20±5.03 64.13±4.41 63.72±3.28 2.476 0.086 68.04±4.11 67.97±3.92 65.56±4.78 2.485 0.091 1.850 0.065 体重指数/(kg/m2) 22.97±1.75 23.09±2.06 23.38±1.14 1.296 0.275 23.99±0.97 24.38±1.10 24.74±1.37 2.989 0.057 1.474 0.141 体温/℃ 37.82±3.20 37.46±3.35 37.08±4.27 0.811 0.446 38.04±3.33 37.72±3.40 37.30±2.29 0.420 0.659 1.245 0.214 吸烟史/例(%) 38(57.58) 60(54.55) 57(59.37) 0.500 0.779 16(47.06) 6(60.00) 12(50.00) 0.518 0.772 1.075 0.300 饮酒史/例(%) 30(45.45) 49(44.55) 46(47.92) 0.243 0.885 12(35.29) 5(50.00) 6(25.00) 2.037 0.361 3.453 0.063 主要症状/例(%) 6.927 0.328 2.611 0.856 1.524 0.064 黑便 23(34.85) 30(27.27) 27(28.13) 11(32.35) 4(40.00) 7(29.17) 腹痛 14(21.21) 10(9.09) 14(14.58) 4(11.76) 2(20.00) 1(4.17) 呕血 30(45.45) 17(15.45) 16(16.67) 10(29.41) 4(40.00) 4(16.67) 黑便+呕血 29(43.94) 15(13.64) 8(8.33) 7(20.59) 3(30.00) 1(4.17) 黑便+腹痛 16(24.24) 9(8.18) 5(5.21) 4(11.76) 2(20.00) 2(8.33) 其他 2(3.03) 4(3.64) 2(2.08) 2(5.88) 0(0) 1(4.17) 出血原因/例(%) 4.162 0.655 1.832 0.935 1.408 0.081 胃溃疡 48(72.73) 31(28.18) 15(15.63) 13(38.24) 4(40.00) 7(29.17) 十二指肠溃疡 18(27.27) 42(38.18) 20(20.83) 12(35.29) 5(50.00) 4(16.67) 急性胃黏膜病变 8(12.12) 30(27.27) 13(13.54) 6(17.65) 2(20.00) 5(20.83) 肿瘤 9(13.64) 14(12.73) 10(10.42) 4(11.76) 1(10.00) 2(8.33) 其他 2(3.03) 7(6.36) 6(6.25) 2(5.88) 0(0) 1(4.17) 用药史/例(%) 12(18.18) 33(30.00) 22(22.92) 3.339 0.188 9(26.47) 4(40.00) 6(25.00) 0.862 0.650 0.651 0.347 上消化道出血史/例(%) 15(22.73) 31(28.18) 25(26.04) 0.637 0.727 16(47.06) 6(60.00) 12(50.00) 0.518 0.772 4.351 0.014 冠心病/例(%) 12(18.18) 38(34.55) 30(31.25) 5.562 0.062 13(38.24) 3(30.00) 5(20.83) 2.000 0.368 0.962 0.203 糖尿病/例(%) 10(15.15) 32(29.09) 24(25.00) 4.910 0.086 9(26.47) 2(20.00) 6(25.00) 0.173 0.917 0.328 0.742 慢性肾脏病/例(%) 11(16.67) 24(21.82) 12(12.50) 3.137 0.208 8(23.53) 2(20.00) 4(16.67) 0.408 0.816 1.468 0.077 PLT/(×109/L) 190.20±10.55 192.17±11.23 196.38±12.07 2.592 0.010 187.37±7.14 190.26±10.09 192.53±11.66 2.088 0.041 4.038 0.016 Hb/(g/L) 130.16±10.83 132.58±11.29 136.02±12.56 2.070 0.040 127.68±8.23 130.15±11.41 133.07±12.20 2.109 0.039 4.623 0.012 BUN/(mmol/L) 9.01±1.04 8.89±1.23 8.81±1.19 1.977 0.049 9.21±1.10 9.02±1.57 8.87±1.66 3.148 0.003 3.517 0.034 AIMS65评分/分 1.98±0.24 1.90±0.16 1.87±0.15 2.283 0.024 2.15±0.19 2.02±0.21 1.97±0.23 2.541 0.014 1.351 0.072 INR 2.1(1.8,2.6) 1.8(1.4,2.3) 1.5(1.2,2.4) 3.262 0.001 2.3(2.1,2.7) 2.2(2.1,2.8) 2.0(1.8,2.3) 2.264 0.027 1.093 0.134 ASA>Ⅱ/例(%) 24(36.36) 29(26.36) 16(16.67) 8.112 0.017 18(52.94) 3(30.00) 5(20.83) 6.478 0.039 8.374 <0.001 出血病变直径≥2.0 cm/例(%) 14(21.21) 10(9.09) 7(7.29) 8.478 0.014 17(50.00) 4(40.00) 2(8.33) 11.112 0.004 11.205 <0.001 内镜下喷射样出血/例(%) 12(18.18) 9(8.18) 6(6.25) 6.856 0.032 16(47.06) 2(20.00) 3(12.50) 8.522 0.014 9.103 <0.001 收缩压<90 mmHg/例(%) 18(27.27) 32(29.09) 15(15.63) 5.657 0.059 14(41.18) 1(10.00) 4(16.67) 6.072 0.048 1.527 0.063 住院时间/d 10.31±1.20 9.20±1.93 8.14±1.45 2.633 0.010 12.34±1.56 11.24±1.63 9.47±1.72 2.209 0.031 1.797 0.048 术中出血量/mL 51.20±5.79 49.16±4.82 48.03±6.11 2.096 0.037 54.53±6.25 52.48±5.79 50.67±5.90 2.126 0.038 2.065 0.041 输血/例(%) 22(33.33) 30(27.27) 13(13.54) 9.581 0.008 16(47.06) 5(50.00) 3(12.50) 8.468 0.014 2.004 0.039 输血量/U 2.43±0.72 1.90±1.03 1.73±0.69 2.177 0.031 3.70±0.75 3.11±1.15 2.73±0.66 2.099 0.040 3.826 0.026 表 2 不同治疗时机术后效果比较
项目 紧急组(100例) 早期组(120例) 延迟组(120例) F P 收缩压<90 mmHg 治疗前 35(35.00) 43(35.83) 41(34.17) 4.861 0.503 治疗后 20(20.00) 16(13.33)1) 19(15.83)1)2) 12.651 <0.001 心率/(次/min) 治疗前 101.36±15.21 99.85±13.29 100.72±10.34 6.367 0.247 治疗后 87.35±12.63 79.56±12.08 82.41±11.52 7.651 0.105 AIMS65评分 治疗前 1.95±0.42 2.03±0.26 1.97±0.33 6.052 0.381 治疗后 1.41±0.23 1.16±0.251) 1.23±0.201)2) 10.546 0.033 INR 治疗前 2.2(2.3,2.7) 2.3(2.1,2.4) 2.1(2.0,2.3) 4.539 0.591 治疗后 1.4(1.2,1.6) 0.9(0.8,1.3)1) 1.1(1.0,1.5)1)2) 9.827 0.042 TC/(mmol/L) 治疗前 2.90±0.69 3.95±0.72 5.02±0.70 治疗后 5.12±0.37 4.89±0.53 4.95±0.46 5.547 0.410 TG/(mmol/L) 治疗前 1.68±0.11 1.66±0.10 1.71±0.14 6.305 0.218 治疗后 1.60±0.12 1.54±0.09 1.57±0.07 4.982 0.491 LDL-C/(mmol/L) 治疗前 2.65±0.12 2.70±0.21 2.68±0.14 5.120 0.483 治疗后 2.40±0.17 2.31±0.22 2.39±0.16 6.581 0.201 HDL-C/(mmol/L) 治疗前 1.13 ±0.12 1.14±0.09 1.10±0.22 4.857 0.605 治疗后 1.32±0.14 1.30±0.13 1.29±0.10 5.264 0.473 Hb/(g/L) 治疗前 131.66±11.06 133.72±10.41 130.11±13.82 6.851 0.185 治疗后 119.83±5.01 110.38±5.161) 115.67±4.521)2) 11.205 0.014 BUN/(mmol/L) 治疗前 8.95±1.76 9.05±2.03 9.08±0.75 5.574 0.431 治疗后 6.04±1.12 5.25±1.031) 5.68±1.171)2) 9.781 0.045 UA/(μmol/L) 治疗前 350.54±62.71 342.67±47.53 330.47±56.32 4.984 0.581 治疗后 341.21±26.28 317.05±24.01 337.52±31.54 6.549 0.223 PLT/(×109/L) 治疗前 193.75±11.03 195.08±10.61 195.11±11.53 7.591 0.193 治疗后 191.85±10.61 184.40±9.341) 189.32±10.171)2) 15.214 <0.001 AST/(U/L) 治疗前 31.05±4.82 33.81±4.05 31.97±5.06 4.950 0.593 治疗后 29.91±3.28 28.35±4.22 29.03±3.74 5.953 0.314 ALT/(U/L) 治疗前 33.48±2.53 33.12±3.26 34.84±4.71 3.547 0.609 治疗后 30.61±4.27 31.01±3.06 31.12±3.95 3.001 0.671 与紧急组相比,1)P<0.05;与早期组相比,2)P<0.05。 表 3 治疗失败的多因素分析
因素 β SE Wald χ2 OR(95%CI) P PLT -0.456 1.132 0.162 0.634(0.405~0.869) 0.031 Hb -0.679 1.053 0.416 0.462(0.300~0.932) 0.040 上消化道出血史 0.014 0.621 0.001 1.014(1.003~1.341) 0.024 出血病变直径≥2.0 cm 0.768 0.681 1.273 2.156(1.548~2.757) <0.001 内镜下喷射样出血 0.978 1.249 0.613 2.659(2.033~3.017) 0.021 12 h≤内镜治疗时机≤24 h -0.190 0.698 0.074 0.827(0.608~0.859) <0.001 表 4 临床因素在训练集上一致性指数
临床因素 P C指数 95%CI PLT 0.025 0.636 0.600~0.672 Hb 0.034 0.621 0.611~0.673 上消化道出血史 0.016 0.690 0.640~0.697 出血病变直径≥2.0 cm <0.001 0.736 0.685~0.748 内镜下喷射样出血 0.010 0.697 0.680~0.721 12 h≤内镜治疗时机≤24 h <0.001 0.712 0.651~0.724 -
[1] 李会龙, 张晓哲. 三黄泻心汤在肝脾血瘀型肝硬化合并非静脉曲张性上消化道出血患者中的应用效果研究[J]. 中国中西医结合消化杂志, 2022, 30(11): 794-798. doi: 10.3969/j.issn.1671-038X.2022.11.08
[2] Vasavi AL, Dm M, Ramana M, et al. A Study of Upper GI Endoscopic Findings in Patients Presented with Upper GI Bleed[J]. J Assoc Physicians India, 2023, 71(1): 1.
[3] 王蓉. 分析消化内镜治疗非静脉曲张性上消化道出血后再出血的危险因素[J]. 中国现代药物应用, 2021, 15(2): 63-65. https://www.cnki.com.cn/Article/CJFDTOTAL-ZWYY202102026.htm
[4] Candelli M, Lumare M, Riccioni ME, et al. Are short-stay units safe and effective in the treatment of non-variceal upper gastrointestinal bleeding?[J]. Medicina, 2023, 59(6): 1021. doi: 10.3390/medicina59061021
[5] Bapaye J, Chandan S, Naing LY, et al. Safety and efficacy of over-the-scope clips versus standard therapy for high-risk nonvariceal upper GI bleeding: systematic review and meta-analysis[J]. Gastrointest Endosc, 2022, 96(5): 712-720. e7. doi: 10.1016/j.gie.2022.06.032
[6] Farooq U, Tarar Z, Ashraf M, et al. No difference in mortality from nonvariceal upper gastrointestinal hemorrhage between racial groups: a nationwide time trend analysis, 2008-2018[J]. Mayo Clin Proc, 2023, 98(1): 203-205. doi: 10.1016/j.mayocp.2022.11.007
[7] Aydin H, Berikol GB, Erdogan MO, et al. CHAMPS score in predicting mortality of patients with acute nonvariceal upper gastrointestinal bleeding[J]. Rev Assoc Med Bras, 2023, 69(4): e20221052. doi: 10.1590/1806-9282.20221052
[8] Tarar ZI, Zafar MU, Farooq U, et al. Does performing endoscopy sooner have an impact on outcomes in patients with acute nonvariceal upper gastrointestinal hemorrhage?A systematic review[J]. Cureus, 2021, 13(7): e16092.
[9] Tanabe S. Endoscopic hemostasis for nonvariceal upper gastrointestinal bleeding[J]. Dig Endosc, 2022, 34(Suppl 2): 61-63.
[10] El-Dallal M, Walradt TJ, Stein DJ, et al. Pros and cons of performing early endoscopy in geriatric patients admitted with non-variceal upper gastrointestinal bleeding: analysis of the US national inpatient database[J]. Dig Dis Sci, 2022, 67(3): 826-833. doi: 10.1007/s10620-021-06924-4
[11] Weissman S, Aziz M, Bangolo AI, et al. Relationships of hospitalization outcomes and timing to endoscopy in non-variceal upper gastrointestinal bleeding: a nationwide analysis[J]. World J Gastrointest Endosc, 2023, 15(4): 285-296. doi: 10.4253/wjge.v15.i4.285
[12] 刘爱茹, 李昕, 张晓岚. 《2021年欧洲胃肠内镜学会非静脉曲张性上消化道出血的内镜诊断和管理指南》解读[J]. 中华消化内镜杂志, 2022, 39(3): 174-179. doi: 10.3760/cma.j.cn321436-20210622-00279
[13] 官佳轮, 王格, 韩莹莹, 等. 非静脉曲张性上消化道出血行急诊内镜止血患者病情严重且预后较差[J]. 内科急危重症杂志, 2022, 28(1): 20-23. https://www.cnki.com.cn/Article/CJFDTOTAL-NKJW202201005.htm
[14] 何帅, 王妍. 香砂六君子汤加味联合消化内镜治疗非静脉曲张性上消化道出血及对胃肠功能紊乱的影响[J]. 中国中西医结合消化杂志, 2020, 28(3): 219-222. https://www.cnki.com.cn/Article/CJFDTOTAL-ZXPW202003014.htm
[15] Nguyen C, Dang A, Baliss M, et al. Id: 3526578 predictors of poor outcomes in patients with non-variceal upper gastrointestinal bleeding undergoing upper endoscopy[J]. Gastrointest Endosc, 2021, 93(6): AB29-AB30.
[16] Freitas M, Macedo Silva V, Cúrdia Gonçalves T, et al. How can patient's risk dictate the timing of endoscopy in upper gastrointestinal bleeding?[J]. GE Port J Gastroenterol, 2022, 29(2): 96-105.
[17] 杨修玲, 蔡奉娟, 王巧珍, 等. 内镜检查时机对急性非静脉曲张性上消化道出血患者临床结局的影响[J]. 临床急诊杂志, 2023, 24(3): 149-154. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2023.03.008
[18] Alali AA, Barkun AN. An update on the management of non-variceal upper gastrointestinal bleeding[J]. Gastroenterol Rep(Oxf), 2023, 11: goad011.
[19] Li XX, Zheng XL, Wang YY, et al. Construction of a risk prediction model for non-variceal upper gastrointestinal bleeding and rebleeding based on multi-dimensional indicators and its application research[J]. Am J Transl Res, 2023, 15(5): 3697-3704.
[20] Yuan YZ, Sun LX, Zhou XY, et al. Risk factors for the failure of endoscopic resection of gastric submucosal tumors: a long-term retrospective case-control study[J]. Gastric Cancer, 2022, 25(5): 929-942.
-




 下载:
下载: