-
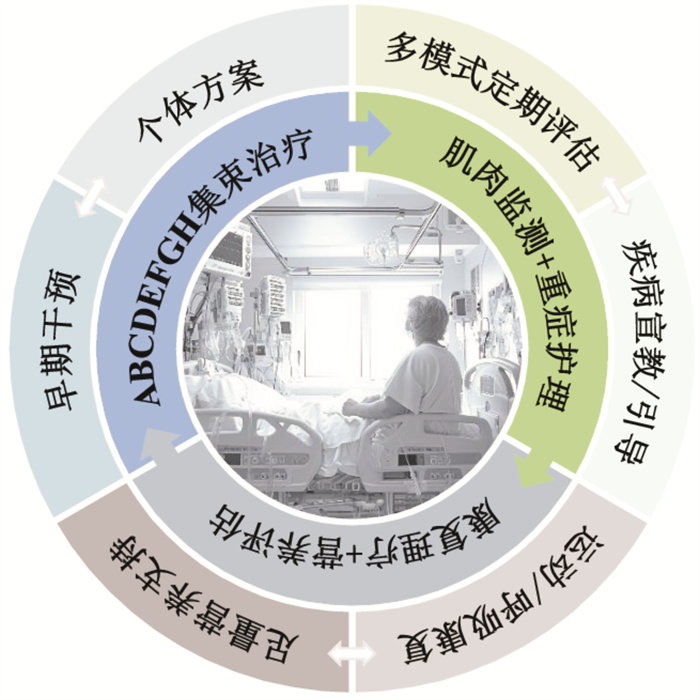
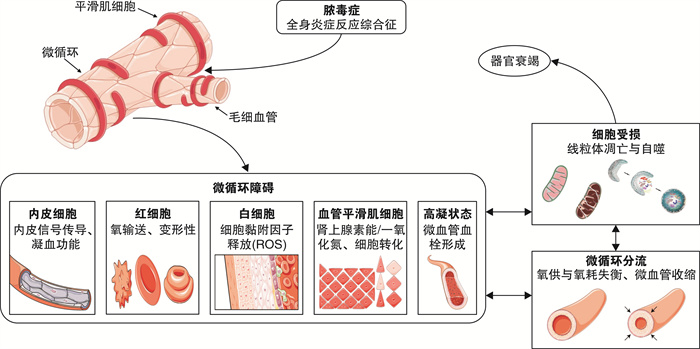
摘要: ICU获得性衰弱(intensive care unit acquired weakness,ICU-AW)作为重症监护室脓毒症患者的常见并发症,多累及骨骼肌、呼吸肌及平滑肌等,会导致脱机困难、住院时间延长、医疗费用剧增,并严重影响患者远期生活质量。但脓毒症ICU-AW的发病机制尚不明确、诊断评估标准缺乏统一、治疗时机和方案选择仍无具体标准。鉴于该病发病机制和诊疗选择存在争议,本文结合国内外文献资料,对脓毒症患者ICU-AW的发病机制及诊疗措施相关研究进展进行综述,以期加深临床多学科对该病的认知并针对性提高疾病的早期认识、诊断及诊疗协作能力。Abstract: Intensive care unit acquired weakness(ICU-AW), as a common complication of patients with sepsis in intensive care unit, mostly involves skeletal muscle, respiratory muscle and smooth muscle, which will lead to difficulty in weaning from mechanical ventilation, prolonged hospital stay, sharp increase in medical costs, and seriously affect the long-term quality of life of patients. However, the pathogenesis of sepsis ICU-AW is still unclear, the diagnostic and evaluation criteria are lack of unity, and there is still no specific standard for the choice of treatment timing and regimen. In view of the controversy about the pathogenesis, diagnosis and treatment of this disease, this article reviews the research progress on the pathogenesis, diagnosis and treatment of ICU-AW in patients with sepsis based on domestic and foreign literature, in order to deepen the clinical multidisciplinary understanding of this disease and improve the early recognition, diagnosis and treatment collaboration ability.
-
Key words:
- sepsis /
- intensive care unit acquired weakness /
- muscle weakness /
- pathogenesis /
- diagnostic evaluation
-

-
表 1 各诊断评估技术对脓毒症ICU-AW的实施方式及优缺点
技术 方式 优点 缺点 患者无法配合 超声技术[45-49] 评估目标肌肉质量、厚度和肌肉强度;观察运动过程中肌肉的收缩情况和力量变化;筛查肌肉坏死和筋膜炎 ①非侵入性床旁检测、安全便捷且方便动态测量,测量设备ICU内常见;②可与MRI和CT结果综合评估;③可早期筛查和预后判断 ①对肌无力的判断容易受评估者主观影响;②易受肥胖和水肿的影响;③不能直接测量评估肌肉力量变化;④对深层肌群的评估准确度不佳 CT技术与MRI技术[46-47, 50-51] 评估脂肪组织有无浸润肌肉组织 ①非侵入性检测;②精确定位、可靠性高;③不受肥胖和水肿的影响;④可评估深层肌群 ①便捷性差,需转运患者;②对检测设备硬件及软件要求度高;③CT存在辐射暴露因素 身体成分测定技术[47, 52-53] 双能X射线吸收测量法(脂肪、骨骼和肌肉);中子活化分析法(中子和原子);生物电阻抗测量法(躯体水分) 非侵入性检测 ①易受肥胖和水肿的影响(双能X射线吸收测量、生物电阻抗测量);②对检测设备要求度高(双能X射线吸收测量、中子活化分析);③辐射暴露(双能X射线吸收测量法、中子活化分析法) 疾病预测模型[49, 54-55] 利用不同数据采用不同模型预测疾病风险因素 ①非侵入性检测;②适用于不同目标人群;③不同测评方式间的互补 ①内容较为烦琐;②部分未进行外部验证、结果可能存在偏倚;③需大样本、大数据进一步验证模型稳定性 直接肌肉刺激与神经、肌肉活检技术[46, 56-57] 肉眼直接观察目标的肌肉兴奋性;镜下观察神经、肌肉组织有无萎缩、坏死、炎症、脂肪浸润、纤维化等 ①无须患者配合;②可用于鉴别诊断危重症多发肌病与危重症神经肌肉病变;③有利于发病机制的研究 ①活检技术为侵入性,有并发症风险;②对疾病本身预后无明显价值 患者可部分配合 神经传导检查与针状肌电图[45-46, 58] ≥两个神经SNAP振幅小于正常值80%;(无传导阻滞)≥两个神经CMAP振幅小于正常正常值80% ①可用于鉴别诊断危重症多发肌病;②适用于无法直接手动测试肌力患者 ①侵入性检查(肌电图);②需要患者部分合作(肌电图);③凝血功能障碍患者不适用 患者清醒且配合,理解测评方式 MRC六分级[59-60](60分):0级,未见肌肉收缩;1级,可见肌肉收缩,未见肢体运动;2级,可见肢体运动,无法抵抗重力;3级,仅可抵抗重力;4级,可抗阻力运动;5级,正常力量 需双侧对称测量肩外展、肘屈曲、腕伸曲、髋屈曲、膝伸展、足背曲显著虚弱,>48分严重无力,<36分 ①非侵入性床旁检测且安全便捷;②在遵循严格的标准化测试流程和位置指南前提下可靠性较高;③便于评估患者整体肌肉功能状态 ①受患者体位和肢体功能状态影响(如:疼痛、敷料、固定装置的限制);②对肌肉功能细微变化的区分敏感性较低,对临界值的判断易受评估者主观影响 MRC四分级[60-61](36分):0级,完全瘫痪;1级,>50%力量丧失;2级,<50%力量丧失;3级,正常肌力 测量方式部位同上,肌无力<24分 同MRC六分级,但相比6级测量更为便捷 同MRC六分级 手持式肌力测量仪[60, 62] 双侧对称测量肌无力:男<11 kg,女<7 kg ①非侵入性床旁检测且安全便捷;②金标准,客观性评价;③高灵敏度、特异度 ①若评估整体肌肉力量需借助其他装置;②应鉴别是否因其他原因引起的肌力下降;③肢体功能状态影响 PFIT-s评分[63-65](每项0~3分) ICU功能状态评分(每项0~7分) 肩屈曲强度、膝伸展力量、每分钟踏频、坐立协助滚动躯体、翻身到坐起、坐立于床边、坐姿到站立、正常走动 ①非侵入性床旁检测且安全便捷;②评估患者的功能能力经过验证 ①存在高限、低限效应;②对临界值的判断容易受评估者主观影响 六分钟步行实验[66-67] 步行6 min ①非侵入性床旁检测且安全便捷;②对部分疾病预后具有一定预测能力 仅适用于可行走患者 注:CMAP,复合肌肉运动动作电位反应;SNAP,感觉神经动作电位;PFIT-s,重症监护身体功能测试评分。 -
[1] Bolton C, Brown J, Sibbald W. The electrophysiologic investigation of respiratory paralysis in critically ill patients[J]. Neurology, 1983, 33(suppl 2): 186.
[2] Bellaver P, Schaeffer AF, Leitao CB, et al. Association between neuromuscular blocking agents and the development of intensive care unit-acquired weakness(ICU-AW): A systematic review with meta-analysis and trial sequential analysis[J]. Anaesth Crit Care Pain Med, 2023, 42(3): 101202. doi: 10.1016/j.accpm.2023.101202
[3] Bouglé A, Rocheteau P, Sharshar T, et al. Muscle regeneration after sepsis[J]. Crit Care, 2016, 20(1): 131. doi: 10.1186/s13054-016-1308-3
[4] Van Aerde N, Meersseman P, Debaveye Y, et al. Five-year impact of ICU-acquired neuromuscular complications: a prospective, observational study[J]. Intensive Care Med, 2020, 46(6): 1184-1193. doi: 10.1007/s00134-020-05927-5
[5] Vanhorebeek I, Latronico N, Van Den Berghe G. ICU-acquired weakness[J]. Intensive Care Med, 2020, 46(4): 637-653. doi: 10.1007/s00134-020-05944-4
[6] Chen J, Huang M. Intensive care unit-acquired weakness: Recent insights[J]. J Intensive Med, 2024, 4(1): 73-80. doi: 10.1016/j.jointm.2023.07.002
[7] 唐宁健, 刘丹, 刘佳雨, 等. 严重创伤患者外周血Th1/Th2细胞平衡和细胞因子水平变化及对发生脓毒症的预测价值[J]. 中国急救医学, 2023, 43(7): 510-517. doi: 10.3969/j.issn.1002-1949.2023.07.002
[8] Park EJ, Kim YM, Kim HJ, et al. Degradation of histone deacetylase 4 via the TLR4/JAK/STAT1 signaling pathway promotes the acetylation of high mobility group box 1(HMGB1) in lipopolysaccharide-activated macrophages[J]. FEBS Open Bio, 2018, 8(7): 1119-1126. doi: 10.1002/2211-5463.12456
[9] Luan YY, Jia M, Zhang H, et al. The potential mechanism of extracellular high mobility group box-1 protein mediated p53 expression in immune dysfunction of T lymphocytes[J]. Oncotarget, 2017, 8(68): 112959-112971. doi: 10.18632/oncotarget.22913
[10] Thoma A, Lightfoot AP. NF-κB and Inflammatory Cytokine Signalling: Role in Skeletal Muscle Atrophy[J]. Adv Exp Med Biol, 2018, 1088: 267-279.
[11] 向朝雪, 李福祥, 朱忠立, 等. NLRP3炎症小体在ICU获得性衰弱大鼠呼吸肌和下肢肌中的表达[J]. 中华肺部疾病杂志(电子版), 2020, 13(2): 198-203. doi: 10.3877/cma.j.issn.1674-6902.2020.02.014
[12] Wang H, Yang Y, Zhang X, et al. Liensinine attenuates inflammation and oxidative stress in spleen tissue in an LPS-induced mouse sepsis model[J]. J Zhejiang Univ Sci B, 2023, 24(2): 185-190. doi: 10.1631/jzus.B2200340
[13] Szentesi P, Csernoch L, Dux L, et al. Changes in Redox Signaling in the Skeletal Muscle with Aging[J]. Oxid Med Cell Longev, 2019, 2019: 4617801.
[14] Swash M, De Carvalho M. Intensive Care Unit-Acquired Weakness: Neuropathology[J]. J Clin Neurophysiol, 2020, 37(3): 197-199. doi: 10.1097/WNP.0000000000000660
[15] Klawitter F, Ehler J, Bajorat R, et al. Mitochondrial Dysfunction in Intensive Care Unit-Acquired Weakness and Critical Illness Myopathy: A Narrative Review[J]. Int J Mol Sci, 2023, 24(6): 5516. doi: 10.3390/ijms24065516
[16] Singh A, Yadav A, Phogat J, et al. Dynamics and Interplay between Autophagy and Ubiquitin-proteasome system Coordination in Skeletal Muscle Atrophy[J]. Curr Mol Pharmacol, 2022, 15(3): 475-486. doi: 10.2174/1874467214666210806163851
[17] 李天梅, 刘力, 王晓斌. 脓毒症通过抑制AKT/GSK3β磷酸化导致骨骼肌细胞膜nAChRs聚集障碍[J]. 南方医科大学学报, 2019, 39(11): 1337-1343. https://www.cnki.com.cn/Article/CJFDTOTAL-DYJD201911012.htm
[18] Liu L, Xie F, Wei K, et al. Sepsis induced denervation-like changes at the neuromuscular junction[J]. J Surg Res, 2016, 200(2): 523-532. doi: 10.1016/j.jss.2015.09.012
[19] 王小军. 炎症反应及细胞内钙浓度异常升高在脓毒症发展中的作用分析[J]. 中南医学科学杂志, 2020, 48(2): 209-213. https://www.cnki.com.cn/Article/CJFDTOTAL-HYYY202002027.htm
[20] Jaber S, Petrof B J, Jung B, et al. Rapidly progressive diaphragmatic weakness and injury during mechanical ventilation in humans[J]. Am J Respir Crit Care Med, 2011, 183(3): 364-371. doi: 10.1164/rccm.201004-0670OC
[21] Latronico N, Bertolini G, Guarneri B, et al. Simplified electrophysiological evaluation of peripheral nerves in critically ill patients: the Italian multi-centre CRIMYNE study[J]. Crit Care, 2007, 11(1): R11. doi: 10.1186/cc5671
[22] 邱昱, 姜利, 席修明. 机械通气患者ICU获得性肌无力早期发病率及预后研究[J]. 中华危重病急救医学, 2019, 31(7): 821-826. doi: 10.3760/cma.j.issn.2095-4352.2019.07.005
[23] Van Aerde N, Van Den Berghe G, Wilmer A, et al. Intensive care unit acquired muscle weakness in COVID-19 patients[J]. Intensive Care Med, 2020, 46(11): 2083-2085. doi: 10.1007/s00134-020-06244-7
[24] Smuder AJ, Nelson WB, Hudson MB, et al. Inhibition of the ubiquitin-proteasome pathway does not protect against ventilator-induced accelerated proteolysis or atrophy in the diaphragm[J]. Anesthesiology, 2014, 121(1): 115-126. doi: 10.1097/ALN.0000000000000245
[25] Azuelos I, Jung B, Picard M, et al. Relationship between Autophagy and Ventilator-induced Diaphragmatic Dysfunction[J]. Anesthesiology, 2015, 122(6): 1349-1361. doi: 10.1097/ALN.0000000000000656
[26] Smuder AJ, Sollanek KJ, Min K, et al. Inhibition of forkhead boxO-specific transcription prevents mechanical ventilation-induced diaphragm dysfunction[J]. Crit Care Med, 2015, 43(5): e133-142. doi: 10.1097/CCM.0000000000000928
[27] Agten A, Maes K, Thomas D, et al. Bortezomib partially protects the rat diaphragm from ventilator-induced diaphragm dysfunction[J]. Crit Care Med, 2012, 40(8): 2449-255. doi: 10.1097/CCM.0b013e3182553a88
[28] Smuder AJ, Sollanek KJ, Nelson WB, et al. Crosstalk between autophagy and oxidative stress regulates proteolysis in the diaphragm during mechanical ventilation[J]. Free Radic Biol Med, 2018, 115: 179-190. doi: 10.1016/j.freeradbiomed.2017.11.025
[29] 高志伟, 刘玲, 谢剑锋, 等. 急性呼吸窘迫综合征机械通气患者人机不同步的研究进展[J]. 中华医学杂志, 2015, 95(26): 2126-2128. doi: 10.3760/cma.j.issn.0376-2491.2015.26.022
[30] 李金徽, 缪红军. 急性呼吸窘迫综合征患者以驱动压为导向的机械通气策略研究进展[J]. 中国小儿急救医学, 2020, 27(10): 758-761. doi: 10.3760/cma.j.issn.1673-4912.2020.10.010
[31] 张倩, 周静, 朱冬梅, 等. 镇痛镇静对延长机械通气患者膈肌萎缩的影响[J]. 南京医科大学学报(自然科学版), 2021, 41(2): 244-247. https://www.cnki.com.cn/Article/CJFDTOTAL-NJYK202102018.htm
[32] Li SP, Zhou XL, Zhao Y. Sedation with midazolam worsens the diaphragm function than dexmedetomidine and propofol during mechanical ventilation in rats[J]. Biomed Pharmacother, 2020, 121: 109405. doi: 10.1016/j.biopha.2019.109405
[33] Preiser JC, Van Zanten AR, Berger MM, et al. Metabolic and nutritional support of critically ill patients: consensus and controversies[J]. Crit Care, 2015, 19(1): 35. doi: 10.1186/s13054-015-0737-8
[34] Preiser JC. High protein intake during the early phase of critical illness: yes or no?[J]. Crit Care, 2018, 22(1): 261. doi: 10.1186/s13054-018-2196-5
[35] 李治丰. 脓毒症患者ICU获得性肌无力相关影响因素分析[J]. 青岛医药卫生, 2021, 53(2): 121-123. https://www.cnki.com.cn/Article/CJFDTOTAL-QDYW202102012.htm
[36] Nunes EA, Colenso-Semple L, Mckellar SR, et al. Systematic review and meta-analysis of protein intake to support muscle mass and function in healthy adults[J]. J Cachexia Sarcopenia Muscle, 2022, 13(2): 795-810. doi: 10.1002/jcsm.12922
[37] 王宁, 丁显飞, 崔玉青, 等. 甲磺酸加贝酯改善脓毒症急性肺损伤大鼠的代谢组学研究[J]. 中华急诊医学杂志, 2022, 31(2): 6.
[38] Cervantes-Barragan L, Chai JN, Tianero MD, et al. Lactobacillus reuteri induces gut intraepithelial CD4(+)CD8α(+)T cells[J]. Science, 2017, 357(6353): 806-810. doi: 10.1126/science.aah5825
[39] Krishnan S, Ding Y, Saedi N, et al. Gut Microbiota-Derived Tryptophan Metabolites Modulate Inflammatory Response in Hepatocytes and Macrophages[J]. Cell Rep, 2018, 23(4): 1099-111. doi: 10.1016/j.celrep.2018.03.109
[40] Mankowski RT, Laitano O, Darden D, et al. Sepsis-Induced Myopathy and Gut Microbiome Dysbiosis: Mechanistic Links and Therapeutic Targets[J]. Shock, 2022, 57(1): 15-23. doi: 10.1097/SHK.0000000000001843
[41] Liu Y, Xu L, Yang Z, et al. Gut-muscle axis and sepsis-induced myopathy: The potential role of gut microbiota[J]. Biomed Pharmacother, 2023, 163: 114837. doi: 10.1016/j.biopha.2023.114837
[42] Pun BT, Balas MC, Barnes-Daly MA, et al. Caring for Critically Ill Patients with the ABCDEF Bundle: Results of the ICU Liberation Collaborative in Over 15, 000 Adults[J]. Crit Care Med, 2019, 47(1): 3-14.
[43] Benoussaad M, Rotella F, Chaibi I. Flatness of musculoskeletal systems under functional electrical stimulation[J]. Med Biol Eng Comput, 2020, 58(5): 1113-1126. doi: 10.1007/s11517-020-02139-3
[44] Park T, Lee M, Jeong T, et al. Quantitative Analysis of EEG Power Spectrum and EMG Median Power Frequency Changes after Continuous Passive Motion Mirror Therapy System[J]. Sensors(Basel), 2020, 20(8): 2354.
[45] Kelmenson DA, Quan D, Moss M. What is the diagnostic accuracy of single nerve conduction studies and muscle ultrasound to identify critical illness polyneuromyopathy: a prospective cohort study[J]. Crit Care, 2018, 22(1): 342.
[46] Formenti P, Umbrello M, Coppola S, et al. Clinical review: peripheral muscular ultrasound in the ICU[J]. Ann Intensive Care, 2019, 9(1): 57.
[47] Joskova V, Patkova A, Havel E, et al. Critical evaluation of muscle mass loss as a prognostic marker of morbidity in critically ill patients and methods for its determination[J]. J Rehabil Med, 2018, 50(8): 696-704.
[48] Fisse AL, May C, Motte J, et al. New Approaches to Critical Illness Polyneuromyopathy: High-Resolution Neuromuscular Ultrasound Characteristics and Cytokine Profiling[J]. Neurocrit Care, 2021, 35(1): 139-152.
[49] Hernández-Socorro CR, Saavedra P, López-Fernández JC, et al. Assessment of Muscle Wasting in Long-Stay ICU Patients Using a New Ultrasound Protocol[J]. Nutrients, 2018, 10(12): 1849.
[50] Rehmann R, Enax-Krumova E, Meyer-Frießem CH, et al. Quantitative muscle MRI displays clinically relevant myostructural abnormalities in long-term ICU-survivors: a case-control study[J]. BMC Med Imaging, 2023, 23(1): 38.
[51] Albano D, Messina C, Vitale J, et al. Imaging of sarcopenia: old evidence and new insights[J]. Eur Radiol, 2020, 30(4): 2199-2208.
[52] Messina C, Albano D, Gitto S, et al. Body composition with dual energy X-ray absorptiometry: from basics to new tools[J]. Quant Imaging Med Surg, 2020, 10(8): 1687-1698.
[53] Ko SJ, Cho J, Choi SM, et al. Phase Angle and Frailty Are Important Prognostic Factors in Critically Ill Medical Patients: A Prospective Cohort Study[J]. J Nutr Health Aging, 2021, 25(2): 218-223.
[54] 钟富秀. 体外循环术后患者ICU获得性衰弱现况调查及列线图的构建[D]. 福州: 福建医科大学, 2022.
[55] Yang Z, Wang X, Chang G, et al. Development and validation of an intensive care unit acquired weakness prediction model: A cohort study[J]. Front Med(Lausanne), 2023, 10: 1122936.
[56] Friedrich O, Reid MB, Van Den Berghe G, et al. The Sick and the Weak: Neuropathies/Myopathies in the Critically Ill[J]. Physiol Rev, 2015, 95(3): 1025-1109.
[57] 戴廷军. 肌肉活检技术在神经肌肉疾病诊断中的应用[J]. 重庆医科大学学报, 2021, 46(7): 786-788. https://www.cnki.com.cn/Article/CJFDTOTAL-ZQYK202107014.htm
[58] Juel VC. Clinical neurophysiology of neuromuscular junction disease[J]. Handb Clin Neurol, 2019, 161: 291-303.
[59] Larson ST, Wilbur J. Muscle Weakness in Adults: Evaluation and Differential Diagnosis[J]. Am Fam Physician, 2020, 101(2): 95-108.
[60] Parry SM, Berney S, Granger CL, et al. A new two-tier strength assessment approach to the diagnosis of weakness in intensive care: an observational study[J]. Crit Care, 2015, 19(1): 52.
[61] Vanhoutte EK, Faber CG, Van Nes SI, et al. Modifying the Medical Research Council grading system through Rasch analyses[J]. Brain, 2012, 135(Pt 5): 1639-1649.
[62] Muscular weakness assessment: use of normal isometric strength data. The National Isometric Muscle Strength(NIMS)Database Consortium[J]. Arch Phys Med Rehabil, 1996, 77(12): 1251-1255.
[63] Parry SM, Baldwin CE. Clinimetrics: The Physical Function in ICU test-scored[J]. J Physiother, 2022, 68(1): 73.
[64] Garcia D, De Sousa Neto IV, De Souza Monteiro Y, et al. Reliability and Validity of a Portable Traction Dynamometer in Knee-Strength Extension Tests: An Isometric Strength Assessment in Recreationally Active Men[J]. Healthcare(Basel), 2023, 11(10): 1466.
[65] Dos Santos JSF, Silva GAG, Lima N, et al. Linking Intensive Care Unit functional scales to the International Classification of Functioning: proposal of a new assessment approach[J]. BMC Health Serv Res, 2023, 23(1): 871.
[66] Chan KS, Pfoh ER, Denehy L, et al. Construct validity and minimal important difference of 6-minute walk distance in survivors of acute respiratory failure[J]. Chest, 2015, 147(5): 1316-1326.
[67] Parry SM, Nalamalapu SR, Nunna K, et al. Six-Minute Walk Distance After Critical Illness: A Systematic Review and Meta-Analysis[J]. J Intensive Care Med, 2021, 36(3): 343-351.
-

计量
- 文章访问数: 83
- 施引文献: 0



 下载:
下载: