-
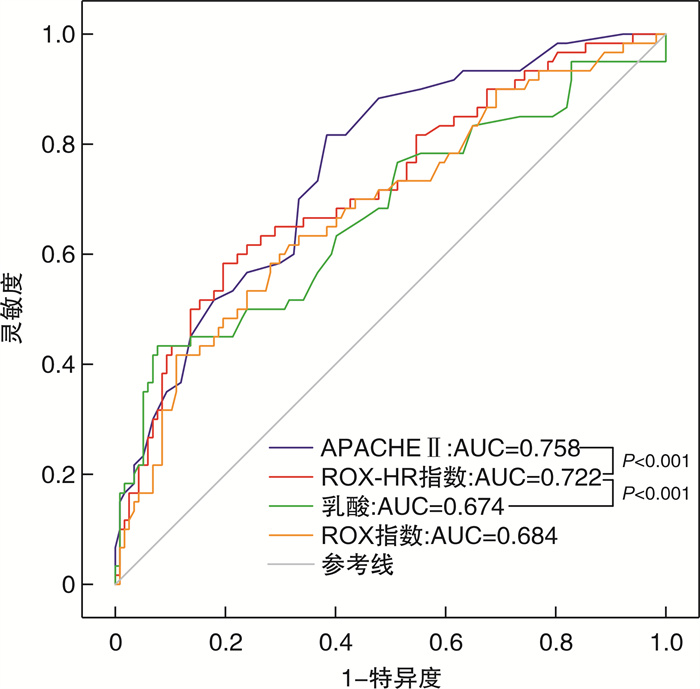
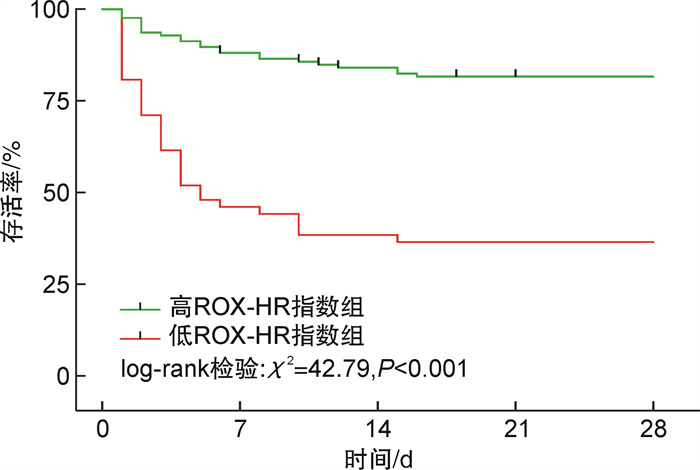
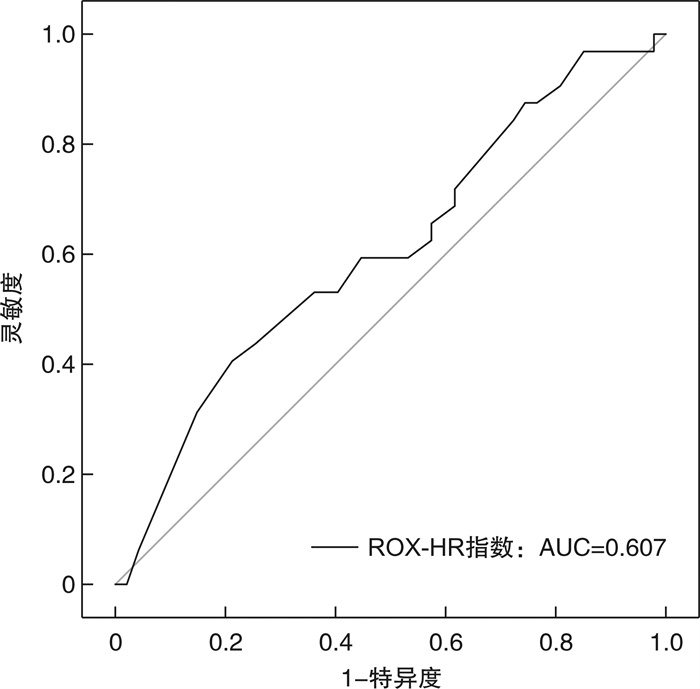
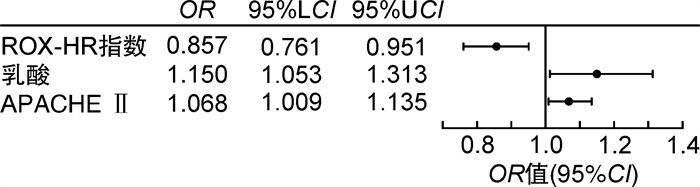
摘要: 目的 探讨ROX-HR指数对于脓毒症患者28 d死亡率的预测价值。方法 选取我院2022年10月—2023年10月收治的178例脓毒症患者和79例脓毒性休克患者,进行回顾性研究。通过入院后2 h内所记录的呼吸、心率、氧饱和度、吸入氧浓度计算ROX-HR指数及ROX指数。记录2 h内最差的ROX-HR指数及ROX指数。采用logistic回归模型确定与脓毒症28 d死亡率相关的独立预测因素。采用受试者工作特征(receiver operator characteristic,ROC)曲线评价ROX-HR指数对脓毒症患者的预测价值。用约登指数确定ROX-HR指数对脓毒症患者死亡率的预测价值。根据约登指数确定的ROX-HR指数最佳截点值(6.3),将所有脓毒症患者分为高ROX-HR指数组(ROX-HR指数≥6.3)和低ROX-HR指数组(ROX-HR指数<6.3),绘制Kaplan-Meier生存曲线分析ROX-HR指数与两组患者生存状态的关系。结果 通过logistic回归分析提示更高的APACHE Ⅱ评分、乳酸及更低的ROX-HR指数与脓毒症患者的28 d死亡率发生独立相关。通过ROC的结果得出,ROX-HR指数、APACHE Ⅱ评分、乳酸和ROX指数的ROC曲线下面积(area under curve,AUC)分别为0.722(95%CI:0.641~0.802)、0.758(95%CI:0.685~0.830)、0.674(95%CI:0.585~0.762)和0.684(95%CI: 0.600~0.768)。通过Kaplan-Meier生存曲线分析显示,高ROX-HR指数组累计生存率明显高于低ROX-HR指数组(79.37% vs 34.62%,P<0.01)。ROX-HR指数与脓毒性休克患者的28 d死亡率的AUC为0.607。结论 ROX-HR指数在死亡组中明显低于存活组,ROX-HR指数<6.3是脓毒症患者28 d死亡风险的独立预测因素。ROX-HR指数对于脓毒性休克患者的预测能力较差。Abstract: Objective To investigate the predictive value of the ROX-HR index for 28-day mortality in sepsis patients.Methods A total of 178 patients with sepsis admitted to our hospital from October 2022 to October 2023 were selected for this retrospective study. ROX-HR index and ROX index were calculated from respiration, heart rate, oxygen saturation, and inspired oxygen concentration recorded within 2 hours after admission. The worst ROX-HR index and ROX index within 2 hours were recorded. Logistic regression modeling was used to determine the independent predictors associated with 28-day mortality in sepsis patients. The predictive value of the ROX-HR index for sepsis patients was evaluated using the Receiver operator characteristic(ROC) curve. The predictive value of ROX-HR index for mortality in sepsis patients was determined using the Youden index. Based on the optimal cut-off value of ROX-HR index determined by the Youden index, all sepsis patients were divided into the high ROX-HR index group and the low ROX-HR index, and the Kaplan-Meier survival curves were plotted to analyze the relationship between ROX-HR index and the survival status of the two groups of patients.Results Higher APACHE Ⅱ score, higher lactate and lower ROX-HR index were suggested to be independently associated with the 28-day mortality in sepsis patients by logistic regression analysis. The results of area under curve(AUC) of ROX-HR index, APACHE Ⅱ, lactate and ROX index were 0.722(95%CI: 0.641-0.802)、0.758(95%CI: 0.685-0.830)、0.674(95%CI: 0.585-0.762) and 0.684(95%CI: 0.600-0.768), respectively. Patients were categorized into high and low ROX-HR groups based on the best cut-off value(6.3) of ROX-HR for predicting 28-day mortality in sepsis patients, and analysis of the Kaplan-Meier curves showed that the cumulative survival rate in the high ROX-HR index group was significantly higher than that in the low ROX-HR index group(79.37% vs 34.62%, P < 0.01). The AUC of ROX-HR index for patients with septic shock was 0.607.Conclusion ROX-HR index was significantly lower in the death group than in the survival group, and ROX-HR index < 6.3 was an independent predictor of 28-day mortality in sepsis patients. The ROX-HR index has poor predictive value in patients with septic shock.
-
Key words:
- sepsis /
- ROX index /
- ROX-HR index
-

-
表 1 生存组和死亡组患者基线资料比较
变量 生存组(118例) 死亡组(60例) P 年龄/岁 66.0(56.0~73.0) 69.0(60.0~76.0) 0.182 性别/例(%) 0.684 男 70(59.32) 38(62.29) 女 48(40.68) 22(37.71) 基础疾病/例(%) 高血压 34(28.81) 21(35.00) 0.401 糖尿病 37(31.36) 26(43.33) 0.116 慢性肾疾病 16(13.56) 9(15.00) 0.796 冠心病 11(9.32) 5(8.33) 0.747 脑卒中 4(3.39) 2(3.33) 0.830 COPD 3(2.54) 2(3.33) 0.768 其他 39(33.05) 16(26.67) 0.386 感染部位/例(%) 肺部感染 46(38.98) 31(51.67) 0.108 腹腔感染 23(19.49) 14(23.33) 0.553 泌尿系统感染 42(35.59) 13(21.67) 0.031 皮肤软组织感染 6(5.08) 8(14.81) 0.054 其他 9(7.63) 1(1.67) 0.104 APACHE Ⅱ评分/分 15.0(10.0~22.0) 25.0(18.0~30.0) <0.001 SOFA评分/分 8.0(4.0~11.0) 12.0(9.0~15.0) <0.001 GCS评分/分 15.0(9.0~15.0) 8.0(3.0~9.0) <0.001 IL-6/(pg·mL-1) 165.6(47.6~1177.6) 3296.2(283.4~13765.6) <0.001 IL-10/(pg·mL-1) 11.0(4.8~91.6) 206.6(24.6~979.4) <0.001 乳酸/(mmol·L-1) 2.3(1.5~3.7) 3.6(2.1~8.8) <0.001 呼吸频率/(次·min-1) 20.0(17.0~25.0) 25.0(18.0~32.0) 0.030 心率/(次·min-1) 88.0(76.0~100.0) 106.0(90.0~133.0) <0.001 吸入氧浓度/% 41.0(41.0~50.0) 50.0(41.0~60.0) 0.017 ROX指数 11.89(7.90~14.17) 6.31(4.66~11.07) <0.001 ROX-HR指数 13.27(8.84~18.49) 5.37(3.99~10.98) <0.001 表 2 单因素logistic回归分析
变量 OR 95%CI P 年龄 0.991 0.961~1.021 0.189 APACHE Ⅱ 1.120 1.076~1.172 <0.001 SOFA 1.202 1.118~1.303 <0.001 GCS 0.754 0.687~0.820 <0.001 IL-6 1.000 1.000~1.000 0.001 IL-10 1.000 1.000~1.000 0.103 乳酸 1.250 1.136~1.392 <0.001 ROX指数 0.848 0.781~0.914 <0.001 ROX-HR指数 0.842 0.786~0.896 <0.001 表 3 根据ROX-HR指数的截断点分组后的患者基线特征
变量 高ROX-HR指数组(126例) 低ROX-HR指数组(52例) P 年龄/岁 66.0(55.0~73.0) 69.0(60.0~76.0) 0.182 男性/例(%) 70(59.32) 38(62.29) 0.185 基础疾病/例(%) 高血压 39(30.95) 16(30.77) 0.982 糖尿病 44(34.92) 19(36.54) 0.839 慢性肾疾病 20(15.87) 5(9.62) 0.278 冠心病 11(9.32) 5(9.62) 0.854 脑卒中 4(3.39) 2(3.85) 0.826 COPD 1(0.79) 4(7.69) 0.012 其他 40(31.75) 15(28.85) 0.706 感染部位/例(%) 肺部感染 48(38.10) 29(55.77) 0.031 腹腔感染 27(21.43) 10(19.23) 0.749 泌尿系统感染 45(35.71) 10(19.23) 0.031 皮肤软组织感染 8(6.35) 6(11.54) 0.244 其他 10(7.94) 2(3.85) 0.513 APACHE Ⅱ评分/分 17.0(11.0~23.0) 23.0(15.0~29.0) <0.001 SOFA评分/分 9.0(4.0~12.0) 12.0(8.0~14.0) <0.001 GCS评分/分 15.0(9.0~15.0) 8.0(3.0~10.0) <0.001 IL-6/(pg/mL) 267.3(58.7~4926.3) 1004.9(161.5~14630.1) <0.001 IL-10/(pg/mL) 18.3(6.6~218.8) 56.7(6.6~1045.5) <0.001 乳酸/(mmol/L) 2.4(1.5~3.9) 3.4(1.9~8.1) <0.001 呼吸频率/(次/min) 18.0(16.0~22.0) 32.0(28.0~34.0) <0.001 心率/(次/min) 87.0(76.0~96.0) 120.0(103.0~140.0) <0.001 吸入氧浓度/% 41.0(41.0~41.0) 60.0(50.0~60.0) <0.001 ROX指数 12.41(9.15~14.20) 4.73(4.26~5.50) <0.001 ROX-HR指数 14.55(10.55~18.56) 4.12(3.70~4.83) <0.001 -
[1] Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock(Sepsis-3)[J]. JAMA, 2016, 315(8): 801-810. doi: 10.1001/jama.2016.0287
[2] Weng L, Xu Y, Yin P, et al. National incidence and mortality of hospitalized sepsis in China[J]. Crit Care, 2023, 27(1): 84. doi: 10.1186/s13054-023-04385-x
[3] Machado FR, Azevedo L. Sepsis: A Threat That Needs a Global Solution[J]. Crit Care Med, 2018, 46(3): 454-459. doi: 10.1097/CCM.0000000000002899
[4] Pepper DJ, Sun J, Cui X, et al. Antibiotic-and Fluid-Focused Bundles Potentially Improve Sepsis Management, but High-Quality Evidence Is Lacking for the Specificity Required in the Centers for Medicare and Medicaid Service's Sepsis Bundle(SEP-1)[J]. Crit Care Med, 2019, 47(10): 1290-1300. doi: 10.1097/CCM.0000000000003892
[5] Pierrakos C, Velissaris D, Bisdorff M, et al. Biomarkers of sepsis: time for a reappraisal[J]. Crit Care, 2020, 24(1): 287. doi: 10.1186/s13054-020-02993-5
[6] 陈卫, 石齐芳, 陈嵩, 等. qSOFA评分联合休克指数评估脓毒症患者预后的价值[J]. 临床急诊杂志, 2023, 24(3): 126-130. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2023.03.004?viewType=HTML
[7] 陈正钢, 刘励军. 急诊脓毒症患者早期筛查生物标志物的研究现状与展望[J]. 临床急诊杂志, 2023, 24(2): 99-104. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2023.02.010?viewType=HTML
[8] Goh KJ, Chai HZ, Ong TH, et al. Early prediction of high flow nasal cannula therapy outcomes using a modified ROX index incorporating heart rate[J]. J Intensive Care, 2020, 8: 41. doi: 10.1186/s40560-020-00458-z
[9] Roca O, Messika J, Caralt B, et al. Predicting success of high-flow nasal cannula in pneumonia patients with hypoxemic respiratory failure: The utility of the ROX index[J]. J Crit Care, 2016, 35: 200-205. doi: 10.1016/j.jcrc.2016.05.022
[10] Roca O, Caralt B, Messika J, et al. An Index Combining Respiratory Rate and Oxygenation to Predict Outcome of Nasal High-Flow Therapy[J]. Am J Respir Crit Care Med, 2019, 199(11): 1368-1376. doi: 10.1164/rccm.201803-0589OC
[11] Colaianni-Alfonso N, Montiel GC, Castro-Sayat M, et al. ROX index to predict CPAP outcome in hypoxemic respiratory failure due to COVID-19[J]. Intensive Care Med, 2022, 48(12): 1818-1819. doi: 10.1007/s00134-022-06913-9
[12] Prower E, Grant D, Bisquera A, et al. The ROX index has greater predictive validity than NEWS2 for deterioration in Covid-19[J]. EClinicalMedicine, 2021, 35: 100828. doi: 10.1016/j.eclinm.2021.100828
[13] Ruangsomboon O, Jirathanavichai S, Phanprasert N, et al. Ratio of Oxygen Saturation to Inspired Oxygen, ROX Index, Modified ROX Index to Predict High Flow Cannula Success in COVID-19 Patients: Multicenter Validation Study[J]. West J Emerg Med, 2023, 24(3): 511-521.
[14] Nascimento MS, Zólio BA, Vale LAPA, et al. ROX index as a predictor of failure of high-flow nasal cannula in infants with bronchiolitis[J]. Sci Rep, 2024, 14(1): 389. doi: 10.1038/s41598-024-51214-4
[15] Lee CU, Jo YH, Lee JH, et al. The index of oxygenation to respiratory rate as a prognostic factor for mortality in Sepsis[J]. Am J Emerg Med, 2021, 45: 426-432. doi: 10.1016/j.ajem.2020.09.052
[16] 唐瑜, 吕健, 张丽茹, 等. 脓毒症早期识别的研究进展[J]. 临床急诊杂志, 2022, 23(7): 513-518. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2022.07.011?viewType=HTML
[17] 王重阳, 王璐, 郭仁楠, 等. ROX指数预测老年重症社区获得性肺炎患者气管插管的有效性分析[J]. 临床急诊杂志, 2022, 23(12): 854-858. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2022.12.010?viewType=HTML
[18] Vasquez-Hoyos P, Jacome-Orozco AL, Rodriguez-Mayorga AP, et al. Can the ROX index predict high-flow nasal cannula failure in children under 2 with lower respiratory tract infection?[J]. Pediatr Pulmonol, 2024, 2024: 1-10.
[19] Jiang Y, Jiang FQ, Kong F, et al. Inflammatory anemia-associated parameters are related to 28-day mortality in patients with sepsis admitted to the ICU: a preliminary observational study[J]. Ann Intensive Care, 2019, 9(1): 67. doi: 10.1186/s13613-019-0542-7
[20] Goligorsky MS, Sun D. Glycocalyx in Endotoxemia and Sepsis[J]. Am J Pathol, 2020, 190(4): 791-798. doi: 10.1016/j.ajpath.2019.06.017
[21] Hoover DB, Ozment TR, Wondergem R, et al. Impaired heart rate regulation and depression of cardiac chronotropic and dromotropic function in polymicrobial sepsis[J]. Shock, 2015, 43(2): 185-191. doi: 10.1097/SHK.0000000000000272
[22] De Backer D, Hajjar L, Monnet X. Vasoconstriction in septic shock[J]. Intensive Care Med, 2024, 50(3): 459-462. doi: 10.1007/s00134-024-07332-8
-

| 引用本文: | 曹卫健, 王言理. ROX-HR指数对于脓毒症患者死亡率的预测价值[J]. 临床急诊杂志, 2024, 25(5): 229-234. doi: 10.13201/j.issn.1009-5918.2024.05.004 |
| Citation: | CAO Weijian, WANG Yanli. Predictive value of the ROX-HR index for mortality in patients with sepsis[J]. J Clin Emerg, 2024, 25(5): 229-234. doi: 10.13201/j.issn.1009-5918.2024.05.004 |
- Figure 1.
- Figure 2.
- Figure 3.
- Figure 4.



 下载:
下载: