The value of dynamic ultrasound measurement of optic nerve sheath diameter in guiding the application of mannitol in pre hospital traumatic brain injury
-
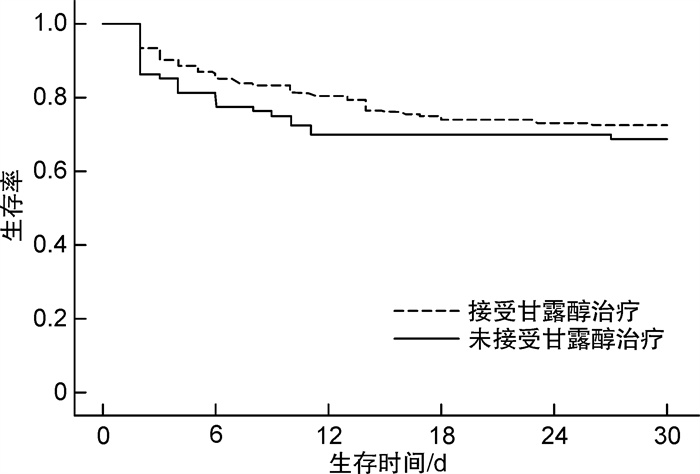
摘要: 目的 通过超声测量视神经鞘直径(optic nerve sheath diameter,ONSD)监测颅内压,以指导院前创伤性脑外伤患者甘露醇的应用。方法 选取2022年12月至2023年7月院前接诊的160例创伤性颅脑外伤患者为研究对象。在120救护车上测量第0、60和120分钟ONSD,根据患者临床结局、是否使用甘露醇及意识水平改变情况进行分组,回顾性收集患者年龄、性别、头部CT结果、发病后第0、60和120分钟ONSD结果、同期格拉斯哥昏迷量表、意识水平改变、是否应用甘露醇降颅压和死亡率等相关数据。评估不同时间段(第0、60和120分钟)ONSD水平与临床结局、是否使用甘露醇、意识水平改变的关系。以ONSD≥5 mm定义为存在高颅压情况,采用Kaplan-Meier曲线分析ONSD≥5 mm的患者是否使用甘露醇与30 d死亡率的相关性。结果 共有160例创伤性脑外伤患者纳入本研究,其中存活患者150例,死亡患者10例。死亡患者的ONSD值在第120分钟为6.79(4.19,8.87) mm,较第0分钟与第60分钟显著增加(P < 0.001)。未接受甘露醇治疗患者的ONSD值在第120分钟为6.51(4.09,8.71) mm,较第0分钟与第60分钟显著增加(P=0.002)。意识障碍加重患者的ONSD值在第120分钟为6.61(4.11,8.83) mm,较第0分钟与第60分钟显著增加(P < 0.001),而意识障碍改善患者的ONSD值在第120分钟为5.91(3.99,8.02) mm,较第0分钟与第60分钟显著降低(P=0.003)。通过生存分析发现,对于ONSD增高(ONSD≥5 mm)的创伤性脑外伤患者,接受甘露醇治疗较未接受甘露醇治疗30 d生存率显著提高(P < 0.01)。结论 院前ONSD动态观察有助于指导创伤性脑外伤患者甘露醇的应用。Abstract: Objective To monitor the intracranial pressure by measuring the optical nerve sheath diameter(ONSD) using ultrasound, in order to guide the application of mannitol in pre hospital patients with traumatic brain injury.Methods A total of 160 patients with traumatic brain injury who were admitted from December 2022 to July 2023 were selected as the study subjects. The ONSD at 0, 60, and 120 minutes were measured on the 120 ambulances. Patients were grouped based on their clinical outcomes, whether mannitol was used, and changes in consciousness levels. Relevant data including age, gender, head CT results, ONSD results at 0, 60, and 120 minutes after onset, Glasgow Coma Scale during the same period, changes in consciousness, use of mannitol to reduce intracranial pressure, and mortality were retrospectively collected. The relationship between ONSD levels and clinical outcomes, use of mannitol, and changes in consciousness levels at different time periods(0, 60, and 120 minutes) were evaluated. Defining ONSD≥5 mm as the presence of high intracranial pressure, Kaplan-Meier curves were used to analyze the correlation between mannitol use and mortality within 30 days in patients with ONSD≥5 mm.Results A total of 160 patients with traumatic brain injury were included in this study, of which 150 cases survived and 10 cases died. Among the patients with death, the ONSD value at 120 minutes was 6.79(4.19, 8.87) mm, which was significantly increased compared to those at 0 and 60 minutes(P < 0.001). For patients who did not receive mannitol treatment, the ONSD value at 120 minutes was 6.51(4.09, 8.71) mm, which was significantly increased compared to those at 0 and 60 minutes(P=0.002). The ONSD value in patients with worsening consciousness disorders at 120 minutes was 6.61(4.11, 8.83) mm, which was significantly increased compared to those at 0 and 60 minutes(P < 0.001), while the ONSD value in patients with improved consciousness disorders at 120 minutes was 5.91(3.99, 8.02) mm, which was significantly decreased compared to those at 0 and 60 minutes(P=0.003). Through survival analysis, it was found that for traumatic brain injury patients with increased ONSD(ONSD≥5 mm), receiving mannitol treatment could significantly improve the survival rate with 30 days compared to not receiving mannitol treatment(P < 0.01).Conclusion Pre hospital ONSD dynamic observation helps guide the application of mannitol in traumatic brain patients with injury.
-
Key words:
- traumatic brain injury /
- optic nerve sheath diameter /
- mannitol /
- survival rate
-

-
表 1 颅脑外伤患者中存活组与死亡组基本资料比较
变量 全队列(160例) 存活组(150例) 死亡组(10例) P 年龄/岁 52.8±3.2 50.8±1.2 56.4±2.5 0.771 男∶女/例 103∶57 96∶54 7∶3 0.409 致伤原因/例(%) <0.001 交通事故 83(51.9) 81(54.0) 2(20.0) 高处坠落 21(13.1) 20(13.3) 1(10.0) 打伤 18(11.3) 16(10.7) 2(20.0) 意外跌倒 24(15.0) 23(15.3) 1(10.0) 其他 14(8.8) 10(6.7) 4(40.0) CT表现/例(%) 颅骨骨折 55(34.4) 51(34.0) 4(40.0) 0.880 硬膜外血肿 54(33.8) 51(34.0) 3(30.0) 0.649 硬膜下血肿 63(39.4) 57(38.0) 6(60.0) 0.005 蛛网膜下腔出血 110(68.8) 104(69.3) 6(60.0) 0.001 意识水平改变/例(%) 0.002 无变化 138(86.3) 133(88.7) 5(50.0) 改善 9(5.6) 8(5.3) 1(10.0) 恶化 13(8.1) 9(6.0) 4(40.0) 使用甘露醇/例(%) 0.001 是 110(68.8) 108(72.0) 2(20.0) 否 50(31.2) 42(28.0) 8(80.0) ONSD/mm 0~60 min 0.31(0.02,0.61) 0.38(0.03,0.67) 0.41(0.05,0.81) 0.001 60~120 min 0.47(0.03,0.91) 0.51(0.04,0.99) 0.61(0.12,1.13) 0.003 0~120 min 0.52(0.04,1.03) 0.57(0.03,1.09) 0.63(0.15,1.19) <0.001 表 2 2 h内ONSD变化与各指标间的关系
变量 Ⅲ类型平方和 df 均方 F P 全队列 0.071 1.491 0.041 1.071 0.918 死亡 2.031 1.630 1.240 38.019 <0.001 使用甘露醇 0.210 1.471 0.139 3.377 <0.001 意识水平改变 2.313 3.267 0.700 22.910 <0.001 表 3 各指标中ONSD在不同时间段的变化
mm 变量 第0分钟 第60分钟 第120分钟 P 全队列 5.33(3.03,7.22) 5.79(3.11,7.88) 5.71(3.09,7.83) 0.199 临床结局 存活 5.55(3.19,7.83) 5.51(3.18,7.96) 5.77(3.29,7.99) 0.192 死亡 6.43(4.01,8.19) 6.71(4.17,8.61) 6.79(4.19,8.87) <0.001 使用甘露醇 是 5.53(3.17,7.82) 5.52(3.16,7.96) 5.76(3.27,7.98) 0.781 否 5.91(4.01,8.03) 6.13(4.08,8.41) 6.51(4.09,8.71) 0.002 意识水平改变 未改变 5.62(3.16,7.90) 5.51(3.71,7.89) 6.44(4.01,8.76) 0.371 加重 6.54(4.14,8.86) 6.60(4.44,8.83) 6.61(4.11,8.83) <0.001 改善 6.33(4.12,8.78) 6.28(4.01,8.69) 5.91(3.99,8.02) 0.003 -
[1] Carney N, Totten AM, O'Reilly C, et al. Guidelines for the Management of Severe Traumatic Brain Injury, Fourth Edition[J]. Neurosurgery, 2017, 80(1): 6-15. doi: 10.1227/NEU.0000000000001432
[2] Fan TH, Huang M, Gedansky A, et al. Prevalence and Outcome of Acute Respiratory Distress Syndrome in Traumatic Brain Injury: A Systematic Review and Meta-Analysis[J]. Lung, 2021, 199(6): 603-610. doi: 10.1007/s00408-021-00491-1
[3] Jiang JY, Gao GY, Feng JF, et al. Traumatic brain injury in China[J]. Lancet Neurol, 2019, 18(3): 286-295. doi: 10.1016/S1474-4422(18)30469-1
[4] 顾帅鹏, 龚嵩, 高伟. 颅内压监测在颅脑损伤中的应用进展[J]. 临床急诊杂志, 2024, 25(2): 87-92, 98. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2024.02.007?viewType=HTML
[5] Khellaf A, Khan DZ, Helmy A. Recent advances in traumatic brain injury[J]. Neurol, 2019, 266(11): 2878-2889. doi: 10.1007/s00415-019-09541-4
[6] 郑曙光, 项彦斌. 床旁即时超声测量视神经鞘直径与重型颅脑损伤患者术后颅内压增高的关系研究[J]. 临床急诊杂志, 2022, 23(10): 715-719. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2022.10.006?viewType=HTML
[7] Stevens RRF, Gommer ED, Aries MJH, et al. Optic nerve sheath diameter assessment by neurosonology: A review of methodologic discrepancies[J]. Neuroimaging, 2021, 31(5): 814-825. doi: 10.1111/jon.12906
[8] Pansell J, Bell M, Rudberg P, et al. Optic nerve sheath diameter measurement by ultrasound: Evaluation of a standardized protocol[J]. Neuroimaging, 2022, 32(1): 104-110. doi: 10.1111/jon.12936
[9] Geeraerts T, Launey Y, Martin L, et al. Ultrasonography of the optic nerve sheath may be useful for detecting raised intracranial pressure after severe brain injury[J]. Intens Care Med, 2007, 33(10): 1704-1711. doi: 10.1007/s00134-007-0797-6
[10] Shokoohi H, Pyle M, Kuhl E, et al. Optic nerve sheath diameter measured by point-of-care ultrasound and MRI[J]. J Neuroimaging, 2020, 30(6): 793-799. doi: 10.1111/jon.12764
[11] Raval R, Shen J, Lau D, et al. Comparison of three point-of-care ultrasound views and MRI measurements for optic nerve sheath diameter: a prospective validity study[J]. Neurocrit Care, 2020, 33(1): 173-181. doi: 10.1007/s12028-019-00881-7
[12] 陈必耀, 陈征, 雷燕妮, 等. 自发性脑出血患者视神经鞘直径与颅内压相关性研究[J]. 中国卒中杂志, 2023, 18(7): 799-804. doi: 10.3969/j.issn.1673-5765.2023.07.009
[13] Robba C, Graziano F, Rebora P, et al. Intracranial pressure monitoring in patients with acute brain injury in the intensive care unit(SYNAPSE-ICU): an international, prospective observational cohort study[J]. Lancet Neurol, 2021, 20(7): 548-558. doi: 10.1016/S1474-4422(21)00138-1
[14] Kochanek PM, Tasker RC, Carney N, et al. Guidelines for the Management of Pediatric Severe Traumatic Brain Injury, Third Edition: Update of the Brain Trauma Foundation Guidelines, Executive Summary[J]. Neurosurgery, 2019, 84(6): 1169-1178. doi: 10.1093/neuros/nyz051
[15] Glushakova OY, Glushakov AV, Yang L, et al. Intracranial Pressure Monitoring in Experimental Traumatic Brain Injury: Implications for Clinical Management[J]. Neurotrauma, 2020, 37(22): 2401-2413. doi: 10.1089/neu.2018.6145
[16] Hawryluk GWJ, Citerio G, Hutchinson P, et al. Intracranial pressure: current perspectives on physiology and monitoring[J]. Intensive Care Med, 2022, 48(10): 1471-1481. doi: 10.1007/s00134-022-06786-y
[17] Gouvêa Bogossian E, Diosdado A, Barrit S, et al. The Impact of Invasive Brain Oxygen Pressure Guided Therapy on the Outcome of Patients with Traumatic Brain Injury: A Systematic Review and Meta-Analysis[J]. Neurocrit Care, 2022, 37(3): 779-789. doi: 10.1007/s12028-022-01613-0
[18] Denchev K, Gomez J, Chen P, et al. Traumatic Brain Injury: Intraoperative Management and Intensive Care Unit Multimodality Monitoring[J]. Anesthesiol Clin, 2023, 41(1): 39-78. doi: 10.1016/j.anclin.2022.11.003
[19] Bernard F, Barsan W, Diaz-Arrastia R, et al. Brain Oxygen Optimization in Severe Traumatic Brain Injury(BOOST-3): a multicentre, randomised, blinded-endpoint, comparative effectiveness study of brain tissue oxygen and intracranial pressure monitoring versus intracranial pressure alone[J]. BMJ Open, 2022, 12(3): e060188. doi: 10.1136/bmjopen-2021-060188
[20] Houzé-Cerfon CH, Bounes V, Guemon J, et al. Quality And Feasibility of Sonographic Measurement of the Optic Nerve Sheath Diameter to Estimate the Risk of Raised Intracranial Pressure After Traumatic Brain Injury in Prehospital Setting[J]. Prehosp Emerg Care, 2019, 23(2): 277-283. doi: 10.1080/10903127.2018.1501444
[21] Canac N, Jalaleddini K, Thorpe SG, et al. Review: pathophysiology of intracranial hypertension and noninvasive intracranial pressure monitoring[J]. Fluids Barriers CNS, 2020, 17(1): 40. doi: 10.1186/s12987-020-00201-8
[22] Lochner P, Czosnyka M, Naldi A, et al. Optic nerve sheath diameter: present and future perspectives for neurologists and critical care physicians[J]. Neurol Sci, 2019, 40(12): 2447-2457. doi: 10.1007/s10072-019-04015-x
[23] Hirzallah MI, Lochner P, Hafeez MU, et al. Quality assessment of optic nerve sheath diameter ultrasonography: Scoping literature review and Delphi protocol[J]. J Neuroimaging, 2022, 32(5): 808-824. doi: 10.1111/jon.13018
[24] Oliveira BDD, Lima FO, Homem HDC, et al. Optic Nerve Sheath Diameter Detects Intracranial Hypertension in Acute Malignant Middle Cerebral Artery Infarction[J]. Stroke Cerebrovasc Dis, 2022, 31(3): 106276. doi: 10.1016/j.jstrokecerebrovasdis.2021.106276
[25] Schroeder C, Katsanos AH, Richter D, et al. Quantification of Optic Nerve and Sheath Diameter by Transorbital Sonography: A Systematic Review and Metanalysis[J]. Neuroimaging, 2020, 30(2): 165-174. doi: 10.1111/jon.12691
[26] Hawryluk GWJ, Citerio G, Hutchinson P, et al. Intracranial pressure: current perspectives on physiology and monitoring[J]. Intensive Care Med, 2022, 48(10): 1471-1481. doi: 10.1007/s00134-022-06786-y
[27] Cooper DJ, Rosenfeld JV, Murray L, et al. Patient Outcomes at Twelve Months after Early Decompressive Craniectomy for Diffuse Traumatic Brain Injury in the Randomized DECRA Clinical Trial[J]. Neurotrauma, 2020, 37(5): 810-816. doi: 10.1089/neu.2019.6869
[28] Bernard F. Neurotrauma and Intracranial Pressure Management[J]. Crit Care Clin, 2023, 39(1): 103-121. doi: 10.1016/j.ccc.2022.08.002
[29] Rubiano AM, Figaji A, Hawryluk GW, et al. Intracranial pressure management: moving beyond guidelines[J]. Curr Opin Crit Care, 2022, 28(2): 101-110. doi: 10.1097/MCC.0000000000000920
-

计量
- 文章访问数: 295
- 施引文献: 0



 下载:
下载: