Early risk factor analysis and prediction of the risk of persistent inflammatory-immunosuppressive-catabolic syndrome in the ICU
-
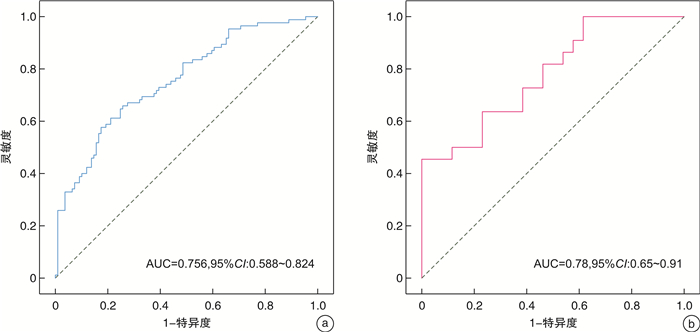
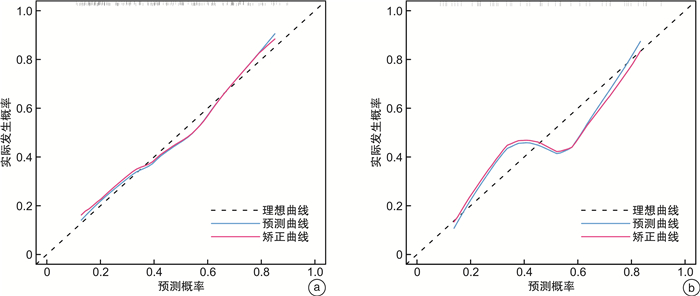
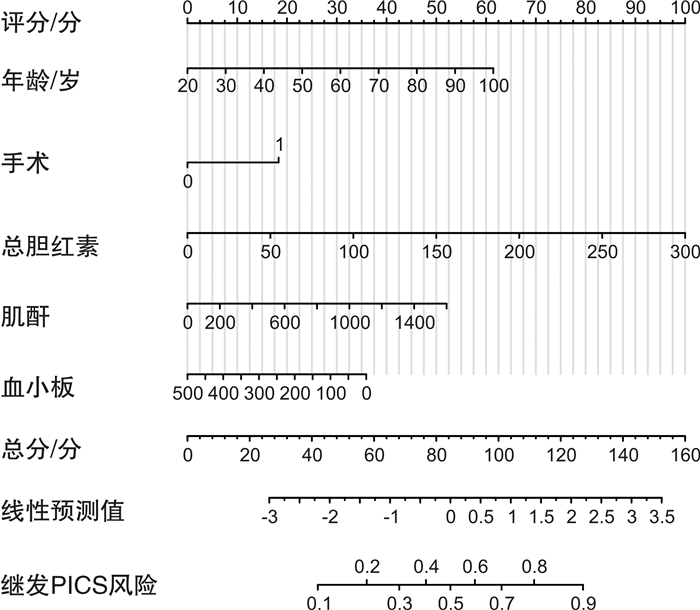
摘要: 目的 探讨重症医学科(intensive care unit, ICU)滞留患者发生持续炎症-免疫-代谢综合征(persistent inflammatory-immunosuppression-catabolic syndrome,PICS)的早期危险因素并构建预测模型。方法 回顾性分析2021年7月-2022年7月蚌埠医学院第一附属医院ICU收治的住院时间≥14 d患者(共计242例)的临床资料。根据是否发生PICS分为PICS组(107例)和非PICS组(135例)进行组间比较。再按照4:1比例,随机将242例患者分为模型建立组(194例)和模型验证组(48例),通过分析模型建立组的临床数据指标,构建PICS的早期预测模型。结果 纳入分析的242例患者中,PICS发生率为44.21%。对模型建立组数据进行单因素分析显示:年龄、手术、血小板计数、总胆红素、肌酐、C-反应蛋白、前白蛋白、高密度脂蛋白与PICS的发生有关(P < 0.05)。筛选患者入院初期即可获得的危险因素并经二元logistic回归分析显示年龄、手术、肌酐、总胆红素、血小板为PICS发生的独立危险因素(P < 0.05),依据早期数据构建ICU滞留患者发生PICS的列线图预测模型,并对预测模型进行评估,模型建立组与验证组的曲线下面积分别为:0.756(95%CI:0.588~0.824)、0.780(95%CI:0.650~0.910)。结论 年龄、手术、肌酐、总胆红素和血小板计数是急危重症患者早期即可获得的危险因素指标,基于此构建的PICS风险预测模型有着良好的区分度及校准度,可以有效评估急危重症患者PICS发病风险,为重症患者的治疗提供参考意见。
-
关键词:
- 重症医学科 /
- 持续炎症免疫抑制分解代谢综合征 /
- 危险因素 /
- 列线图模型
Abstract: Objective To explore the early risk factors of persistent inflammatory-immunosuppression-catabolic syndrome(PICS) in stranded patients in intensive care unit(ICU) and construct a prediction model.Methods Clinical data of 242 patients(in total) admitted to the ICU of a large tertiary Class A hospital from July 1, 2021 to July 31, 2022 was retrospectively analyzed. They were divided into PICS group and non-PICS groups according to whether PICS had occurred. According to the ratio of 4 : 1, 242 patients were randomly divided into model building group(n=194) and model verification group(n=48). By analyzing the clinical data indicators of the model building group, construct the early prediction model of PICS was constructed.Results The 242 patients included in the analysis were divided into the PICS group(107 patients) and in the non-PICS group(135 patients), and the incidence of PICS was 44.21%. Univariate analysis to the data of the model building group showed that age, surgery, platelet, total bilirubin, creatinine, C-reactive protein, pro-albumin, and high-density lipoprotein were related with the occurrence of PICS(P < 0.05). Screen those risk factors that could be obtained at early admission period. Binary Logistic regression analysis showed that, age, surgery, creatinine, total bilirubin, and platelets were independent risk factors for PICS(P < 0.05). Constructed the nomogram prediction model of PICS in ICU retention patients based on early data, and evaluated the prediction model. AUC of the model building group and the model verification group were 0.756(95%CI: 0.588-0.824), 0.780(95%CI: 0.650-0.910), respectively.Conclusion Age, surgery, creatinine value, total bilirubin and platelet are risk factors that can be obtained in the early stage in patients with critical diseases. The PICS risk prediction model constructed based on this has good differentiation and calibration, which can effectively assess the risk of PICS in acute and critical patients and provide reference for the treatment of severe patients. -

-
表 1 纳入患者一般情况分析
X±S 组别 总例数(242例) PICS组(107例) 非PICS组(135例) P 男/例(%) 143(59.09) 68(63.55) 75(55.55) 0.209 年龄/岁 61.45±15.49 66.12±13.03 57.76±16.31 < 0.001 APACHEⅡ评分/分 21.12±6.10 23.28±5.34 19.47±6.08 < 0.001 高血压/例(%) 118(48.76) 47(43.93) 71(52.59) 0.180 糖尿病/例(%) 51(21.07) 27(25.23) 24(17.77) 0.158 脓毒症/例(%) 105(43.39) 55(51.4) 50(37.03) 0.025 机械通气时间/h 237.50±274.55 328.71±271.49 165.21±255.65 < 0.001 ICU住院时间/d 25.81±14.26 28.21±14.17 23.90±14.10 0.019 ICU住院费用/千元 176.85±120.34 229.16±135.13 135.39±87.67 < 0.001 28d继发感染/例(%) 166(68.60) 82(76.64) 84(62.22) 0.016 28d存活/例(%) 174(71.90) 65(60.75) 109(80.74) 0.001 表 2 对模型建立组数据进行单因素logistic回归分析
危险因素 β SE χ2 OR 95%CI P 降钙素原 0.009 0.006 1.466 1.009 0.998~1.023 0.143 高密度脂蛋白 -1.301 0.464 -2.805 0.272 0.104~0.640 0.005 前白蛋白 -0.005 0.002 -2.685 0.995 0.991~0.999 0.007 血磷 0.094 0.210 0.447 1.098 0.724~1.667 0.655 C-反应蛋白 0.004 0.002 2.064 1.004 1.000~1.008 0.039 肌酐 0.002 0.001 2.085 1.002 1.000~1.003 0.037 白蛋白计数 -0.028 0.019 -1.444 0.972 0.935~1.009 0.149 总胆红素 0.015 0.007 2.231 1.015 1.004~1.030 0.026 血小板计数 -0.005 0.002 -3.094 0.995 0.992~0.998 0.002 淋巴细胞计数 -0.163 0.140 -1.162 0.849 0.630~1.102 0.245 中性粒细胞计数 0.010 0.021 0.474 1.010 0.968~1.054 0.636 白细胞计数 0.010 0.019 0.506 1.010 0.972~1.049 0.613 脓毒症 0.349 0.293 1.191 1.418 0.799~2.526 0.234 手术 0.769 0.295 2.606 2.158 1.216~3.875 0.009 年龄 0.031 0.010 3.026 1.031 1.011~1.053 0.002 表 3 多因素logistic回归分析确定PICS发生的危险因素
危险因素 β SE χ2 OR 95%CI P 年龄 0.038 0.012 3.253 1.039 1.016~1.064 0.001 手术 0.842 0.335 2.512 2.321 1.212~4.527 0.012 总胆红素 0.015 0.007 2.317 1.016 1.004~1.031 0.020 血小板计数 -0.004 0.002 -2.059 0.996 0.993~1.000 0.039 肌酐 0.002 0.001 2.013 1.002 1.000~1.003 0.044 -
[1] Gentile LF, Cuenca AG, Efron PA, et al. Persistent inflammation and immunosuppression: a common syndrome and new horizon for surgical intensive care[J]. J Trauma Acute Care Surg, 2012, 72(6): 1491-1501. doi: 10.1097/TA.0b013e318256e000
[2] Mira JC, Gentile LF, Mathias BJ, et al. Sepsis Pathophysiology, Chronic Critical Illness, and Persistent Inflammation-Immunosuppression and Catabolism Syndrome[J]. Crit Care Med, 2017, 45(2): 253-262. doi: 10.1097/CCM.0000000000002074
[3] Hawkins RB, Raymond SL, Stortz JA, et al. Chronic Critical Illness and the Persistent Inflammation, Immunosuppression, and Catabolism Syndrome[J]. Front Immunol, 2018, 9: 1511. doi: 10.3389/fimmu.2018.01511
[4] 夏然, 童兴瑜, 张成密, 等. 持续炎症-免疫抑制-分解代谢综合征研究进展[J]. 中华危重症医学杂志(电子版), 2020, 13(2): 149-153. https://www.cnki.com.cn/Article/CJFDTOTAL-ZWZD202002017.htm
[5] 李娅, 李辉凤, 王铭, 等. 严重创伤并发持续炎症-免疫抑制-分解代谢综合征的研究进展[J]. 中国急救医学, 2021, 41(4): 365-368, 封3. https://www.cnki.com.cn/Article/CJFDTOTAL-ZJJY202104017.htm
[6] Gardner AK, Ghita GL, Wang Z, et al. The Development of Chronic Critical Illness Determines Physical Function, Quality of Life, and Long-Term Survival Among Early Survivors of Sepsis in Surgical ICUs[J]. Crit Care Med, 2019, 47(4): 566-573. doi: 10.1097/CCM.0000000000003655
[7] Rhee C, Dantes R, Epstein L, et al. Incidence and Trends of Sepsis in US Hospitals Using Clinical vs Claims Data, 2009-2014[J]. JAMA, 2017, 318(13): 1241-1249. doi: 10.1001/jama.2017.13836
[8] Rosenthal MD, Vanzant EL, Moore FA. Chronic Critical Illness and PICS Nutritional Strategies[J]. J Clin Med, 2021, 10(11): 2294. doi: 10.3390/jcm10112294
[9] Suzuki G, Ichibayashi R, Masuyama Y, et al. Association of red blood cell and platelet transfusions with persistent inflammation, immunosuppression, and catabolism syndrome in critically ill patients[J]. Sci Rep, 2022, 12(1): 629. doi: 10.1038/s41598-021-04327-z
[10] 徐蓉, 刘军. ICU滞留患者的临床特征及预后分析[J]. 中华危重症医学杂志(电子版), 2021, 14(2): 137-141. https://www.cnki.com.cn/Article/CJFDTOTAL-ZWZD202102008.htm
[11] 吴媛, 王小闯, 侯彦丽, 等. 脓毒症患者并发持续炎症-免疫抑制-分解代谢综合征的危险因素分析[J]. 浙江医学, 2019, 41(16): 1772-1775, 1787. https://www.cnki.com.cn/Article/CJFDTOTAL-ZJYE201916025.htm
[12] Chen X, Lei X, Xu X, et al. Intensive Care Unit-Acquired Weakness in Patients With Extracorporeal Membrane Oxygenation Support: Frequency and Clinical Characteristics[J]. Front Med(Lausanne), 2022, 9: 792201.
[13] Nakamura K, Ogura K, Ohbe H, et al. Clinical Criteria for Persistent Inflammation, Immunosuppression, and Catabolism Syndrome: An Exploratory Analysis of Optimal Cut-Off Values for Biomarkers[J]. J Clin Med, 2022, 11(19): 5790. doi: 10.3390/jcm11195790
[14] Mankowski RT, Anton SD, Ghita GL, et al. Older Adults Demonstrate Biomarker Evidence of the Persistent Inflammation, Immunosuppression, and Catabolism Syndrome(PICS)After Sepsis[J]. J Gerontol A Biol Sci Med Sci, 2022, 77(1): 188-196. doi: 10.1093/gerona/glab080
[15] 杨艳梅, 杨栋梁, 赵文涛, 等. 加重老年急性心肌梗死患者冠状动脉病变风险的列线图预测模型建立[J]. 中华危重病急救医学, 2021, 33(8): 967-972.
[16] 王晶晶, 李竞, 王勇强. 老年脓毒症患者急性肾损伤的临床特征和预后[J]. 中华危重病急救医学, 2019, 31(7): 837-841. https://cdmd.cnki.com.cn/Article/CDMD-11810-1023643263.htm
[17] 唐庭轩, 张聪, 李松波, 等. 多发伤并发持续炎症-免疫抑制-分解代谢综合征患者的临床特征及预后分析[J]. 中华急诊医学杂志, 2021, 30(7): 862-865.
[18] Claushuis TA, van Vught LA, Scicluna BP, et al. Thrombocytopenia is associated with a dysregulated host response in critically ill sepsis patients[J]. Blood, 2016, 127(24): 3062-3072.
[19] Koyama K, Katayama S, Muronoi T, et al. Time course of immature platelet count and its relation to thrombocytopenia and mortality in patients with sepsis[J]. PLoS One, 2018, 13(1): e192064.
[20] Dewitte A, Lepreux S, Villeneuve J, et al. Correction to: Blood platelets and sepsis pathophysiology: A new therapeutic prospect in critically ill patients?[J]. Ann Intensive Care, 2018, 8(1): 32.
[21] Ghimire S, Ravi S, Budhathoki R, et al. Current understanding and future implications of sepsis-induced thrombocytopenia[J]. Eur J Haematol, 2021, 106(3): 301-305.
[22] 王娜, 秦卓, 刘慧珍, 等. 营养风险评分对脓毒症相关性急性肾损伤患者预后的临床价值[J]. 中华危重病急救医学, 2022, 34(3): 245-249.
[23] Peerapornratana S, Manrique-Caballero CL, Gómez H, et al. Acute kidney injury from sepsis: current concepts, epidemiology, pathophysiology, prevention and treatment[J]. Kidney Int, 2019, 96(5): 1083-1099.
[24] Moreno R, Rhodes A, Singer M, et al. Real-world inter-observer variability of the sequential organ failure assessment(SOFA)score in intensive care medicine: the time has come for an update: authors' reply[J]. Crit Care, 2023, 27(1): 182.
[25] Hamoud AR, Weaver L, Stec DE, et al. Bilirubin in the Liver-Gut Signaling Axis[J]. Trends Endocrinol Metab, 2018, 29(3): 140-150.
[26] Gazzin S, Vitek L, Watchko J, et al. A Novel Perspective on the Biology of Bilirubin in Health and Disease[J]. Trends Mol Med, 2016, 22(9): 758-768.
-




 下载:
下载: