The clinical application value of combined prediction model for ROSC in patients with OHCA
-
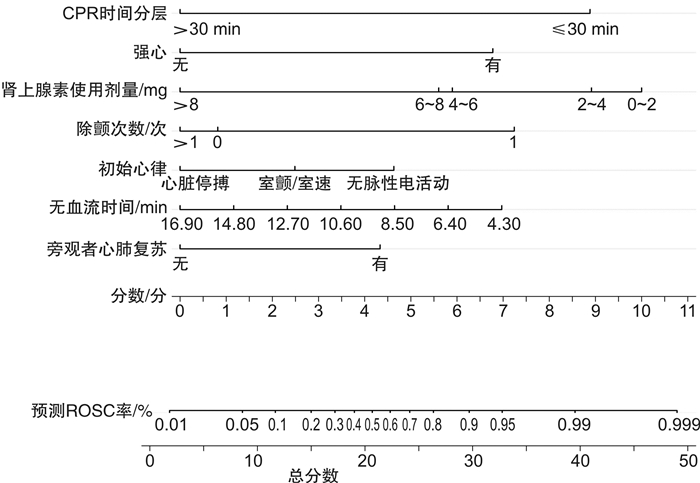
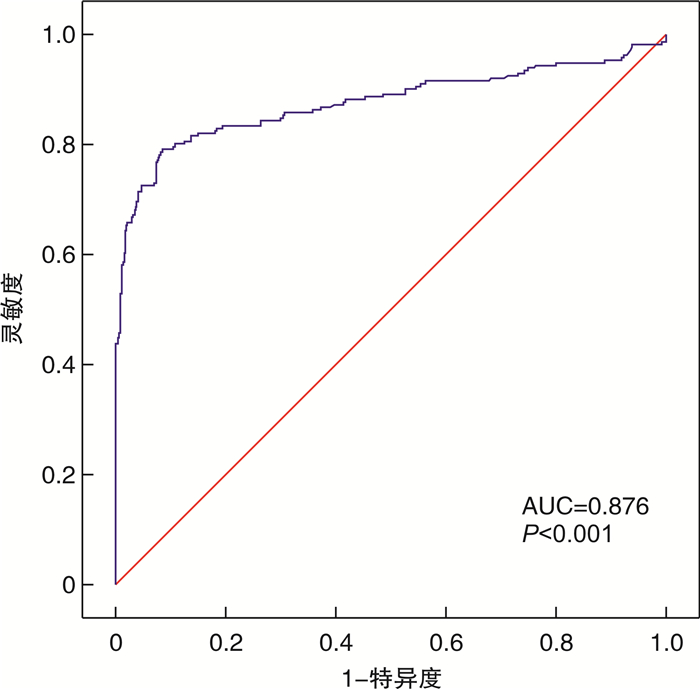
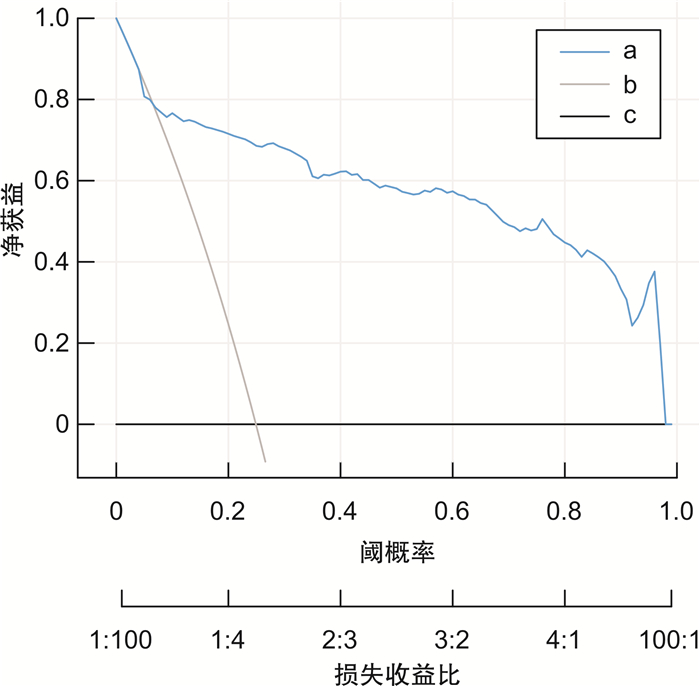
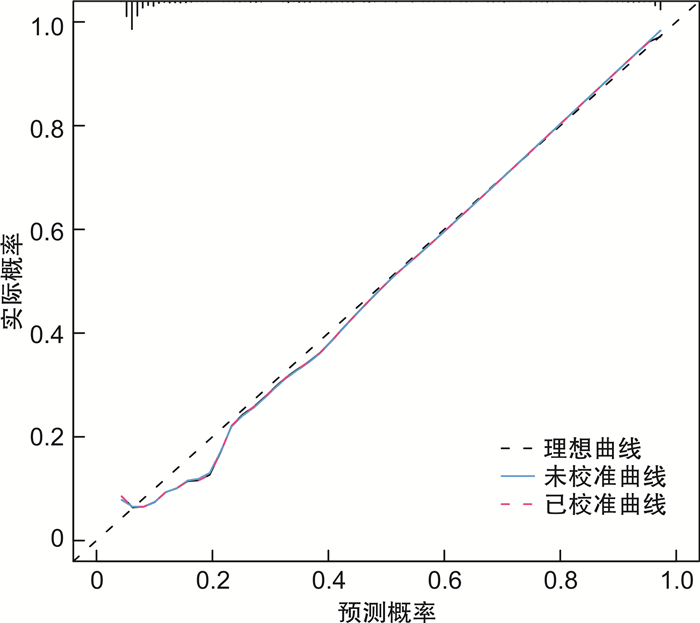
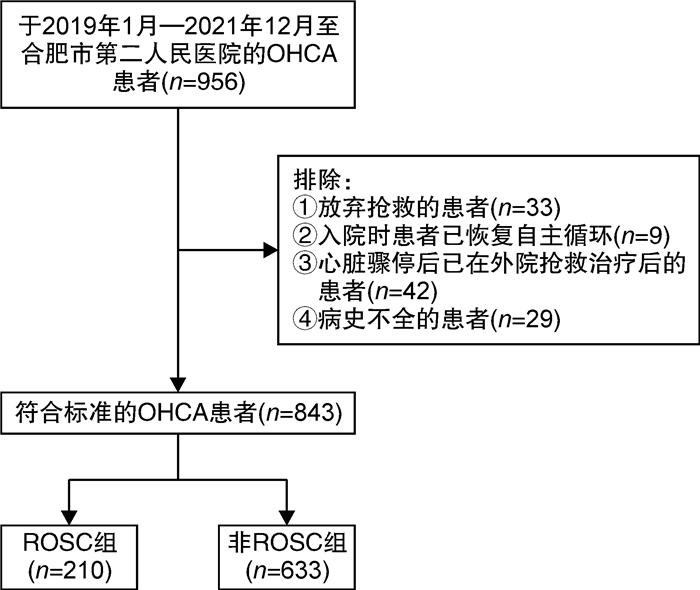
摘要: 目的 探索多指标联合预测模型对院外心脏骤停(out-of-hospital cardiac arrest,OHCA)患者自主循环恢复(return of spontaneous circulation,ROSC)的临床应用价值。方法 选择2019年1月-2021年12月在合肥市第二人民医院急诊科救治的843例OHCA患者为研究对象,根据复苏结果分为ROSC组210例(24.9%),非ROSC组633例(75.1%)。采用单因素分析和二元logistic回归分析筛选独立影响因素,构建列线图,采用校准图、临床决策曲线评估模型,并对模型进行内部验证。结果 无血流时间越短、初始心律为室颤和无脉电活动、有旁观者心肺复苏、除颤次数≤1次、肾上腺素总使用剂量越小、强心药物的使用、CPR时间 < 30 min的OHCA患者更易获得自主循环恢复,由此构建的联合预测模型曲线下面积(area under curve, AUC)为0.876,内部验证校准AUC值为0.876,校准曲线接近预测曲线,决策曲线分析阈概率为8%~100%,表明有良好临床获益。结论 本研究构建的联合预测模型,对OHCA自主循环恢复的预测有一定的临床价值,有助于对OHCA患者进行早期评估及治疗过程中诊疗计划的制定。Abstract: Objective To explore the clinical application value of multi-index combined prediction model for return of spontaneous circulation(ROSC) in patients with out-of-hospital cardiac arrest(OHCA).Methods Eight hundred and forty-three patients with OHCA who were treated in the Emergency Department of the Second People's Hospital of Hefei from January 2019 to December 2021 were selected as the research objects. According to the resuscitation results, there were 210 cases (24.9%) in the ROSC group and 633 cases (75.1%) in the non ROSC group.Univariate analysis and binary logistic regression analysis were used to screen the independent influencing factors, and a nomogram was constructed. The calibration chart and clinical decision curve were used to evaluate the model, and the model was internally validated.Results OHCA patients with shorter no-flow time, ventricular fibrillation and pulseless electrical activity as initial rhythm, bystander cardiopulmonary resuscitation, defibrillation frequency ≤1 time, lower total dose of epinephrine, use of inotropic drugs and cardiopulmonary resuscitation time < 30 min are more likely to obtain return of spontaneous circulation. The area under curve(AUC) area of the combined prediction model was 0.876, and the internal validation calibration AUC value was 0.876. The calibration curve was close to the prediction curve, and the DCA analysis threshold probability was 8%-100%, indicating good clinical benefit.Conclusion The combined prediction model constructed in this study has certain clinical value in predicting the return of spontaneous circulation in OHCA, which is helpful for the early evaluation of patients with OHCA and the formulation of diagnosis and treatment plans during the treatment process.
-

-
表 1 ROSC组和非ROSC组一般资料对比
例(%),X±S 资料 ROSC组(210例) 非ROSC组(633例) t/χ2 P 性别 7.771 0.005 男 128(61.0) 451(71.2) 女 82(39.0) 182(28.8) 年龄/岁 1.925 0.750 < 60 75(35.7) 233(36.8) 60~70 32(15.2) 105(16.6) >70~80 48(22.9) 118(18.6) >80~90 45(21.4) 148(23.4) >90 10(0.5) 29(4.6) 无血流时间 10.52±1.62 11.21±1.97 -5.041 < 0.001 初始心律 127.618 < 0.001 室颤/室速 67(31.9) 32(5.1) 无脉性电活动 36(17.1) 63(10.0) 心脏停搏 107(60.0) 538(85.0) 旁观者 15.323 < 0.001 有 177(84.3) 447(70.6) 无 33(15.7) 186(29.4) 旁观者心肺复苏 43.681 < 0.001 有 55(26.2) 54(8.5) 无 155(73.8) 579(91.5) 病因 7.182 0.066 心源性 176(83.8) 504(79.6) 创伤性 14(6.7) 83(13.1) 低氧 10(4.8) 25(3.9) 其他 10(4.8) 21(3.3) 既往基础疾病 心脏病 34(16.2) 71(11.2) 3.578 0.059 高血压 29(13.8) 60(9.5) 3.132 0.077 肿瘤晚期 7(3.3) 34(5.4) 1.415 0.234 脑卒中 10(4.8) 21(3.3) 0.929 0.335 肺部疾病 9(4.3) 23(3.6) 0.184 0.668 糖尿病 13(6.2) 28(4.4) 1.064 0.302 其他 6(2.9) 18(2.8) < 0.001 0.992 地点 38.449 < 0.001 疗养院 10(4.8) 16(2.5) 工作地点 7(8.1) 15(2.4) 医生办公室 50(23.8) 60(9.5) 公共场所 47(22.4) 186(29.4) 家 85(40.5) 279(44.1) 其他 11(5.2) 77(12.2) 电除颤次数/次 136.943 < 0.001 0 117(55.7) 518(81.8) 1 76(36.2) 32(5.1) >1 17(8.1) 83(13.1) 肾上腺素使用剂量/mg 237.105 < 0.001 0~2 63(30.0) 23(3.6) >2~4 60(28.6) 41(6.5) >4~6 38(18.1) 109(17.2) >6~8 23(11.0) 152(24.0) >8 26(12.4) 308(48.7) 胺碘酮使用 1.606 0.205 有 7(3.3) 35(5.5) 无 203(96.7) 598(94.5) 强心药物使用a) 53.240 < 0.001 有 59(28.1) 53(8.4) 无 151(71.9) 580(91.6) 纠酸药物使用 0.909 0.340 有 68(32.4) 183(28.9) 无 142(67.6) 450(71.1) 入院时血压/mmHgb) 17.126 < 0.001 < 90 40(19.0) 89(14.1) 正在心肺复苏 145(69.0) 513(81.0) >90 25(11.9) 31(4.9) CPR时间分层/min 259.827 < 0.001 < 30 171(81.4) 127(20.1) ≥30 39(18.6) 506(79.9) 注:a)强心药物包括多巴胺、多巴酚丁胺;b)1 mmHg=0.133 kPa。 表 2 二元logistic回归分析结果
因素 β SE P OR 95%CI 无血流时间 -0.135 0.062 0.030 0.874 0.774~0.987 初始心律 心脏停搏 0.034 室颤/室速 0.607 0.664 0.361 1.834 0.499~6.745 无脉电活动 1.130 0.451 0.012 3.094 1.278~7.494 有旁观者心肺复苏 1.057 0.467 0.023 2.878 1.153~7.182 除颤次数/次 0 0.005 1 1.567 0.512 0.002 4.791 1.758~13.056 >1 -0.199 0.445 0.654 0.820 0.343~1.959 肾上腺素剂量/mg 0~2 2.439 0.426 < 0.001 11.457 4.968~26.421 >2~4 2.174 0.386 < 0.001 8.792 4.124~18.741 >4~6 1.439 0.346 < 0.001 4.215 2.140~8.302 >6~8 1.367 0.340 < 0.001 3.922 2.140~7.643 >8 < 0.001 使用强心药物 1.652 0.360 < 0.001 5.220 2.013~10.562 CPR时间 < 30min 2.166 0.249 < 0.001 8.726 5.361~14.203 常量 -2.564 0.716 < 0.001 0.077 表 3 分数X的计算
因素 分数X 分类 -2.5 常数 无血流时间 -0.1 每分钟 初始心律 +0.6 室颤/室速 +1.1 无脉性电活动 旁观者心肺复苏 +1.1 有 除颤次数 +1.6 1次 -0.2 >1次 肾上腺素使用剂量 +2.4 0~2 mg +2.1 >2~4 mg +1.4 >4~6 mg +1.4 >6~8 mg 强心药物应用 -1.7 是 CPR时间 +2.2 < 30 min 表 4 OHCA患者ROSC的各独立预测指标及联合预测模型的预测效果比较
指标 曲线下面积 截断值 灵敏度 特异度 阳性预测值/% 阴性预测值/% 无血流时间 0.611 12.05 min 0.379 0.867 31.7 89.6 初始心律 0.682 0.490 0.850 52.0 83.4 旁观者心肺复苏 0.588 0.355 0.915 50.5 78.9 除颤次数 0.609 0.443 0.818 44.7 81.6 肾上腺素 0.804 0.767 0.727 48.2 90.4 强心药物的使用 0.599 0.281 0.916 52.7 79.3 CPR时间分层 0.807 0.814 0.800 57.4 92.8 联合预测模型 0.876 0.791 0.916 75.8 92.9 -
[1] Kiguchi T, Okubo M, Nishiyama C, et al. Out-of-hospital cardiac arrest across the World: First report from the International Liaison Committee on Resuscitation(ILCOR)[J]. Resuscitation, 2020, 152: 39-49. doi: 10.1016/j.resuscitation.2020.02.044
[2] Virani SS, Alonso A, Benjamin EJ, et al. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association[J]. Circulation, 2020, 141(9): e139-e596.
[3] Grasner JT, Herlitz J, Tjelmeland IBM, et al. European Resuscitation Council Guidelines 2021: Epidemiology of cardiac arrest in Europe[J]. Resuscitation, 2021, 161: 61-79. doi: 10.1016/j.resuscitation.2021.02.007
[4] Xie X, Zheng J, Zheng W, et al. Efforts to Improve Survival Outcomes of Out-of-Hospital Cardiac Arrest in China: BASIC-OHCA[J]. Circ Cardiovasc Qual Outcomes, 2023, 16(2): e008856.
[5] Gamberini L, Mazzoli C A, Allegri D, et al. Factors influencing prehospital physicians' decisions to initiate advanced resuscitation for asystolic out-of-hospital cardiac arrest patients[J]. Resuscitation, 2022, 177: 19-27. doi: 10.1016/j.resuscitation.2022.06.015
[6] Seewald S, Wnent J, Lefering R, et al. CaRdiac Arrest Survival Score(CRASS)-A tool to predict good neurological outcome after out-of-hospital cardiac arrest[J]. Resuscitation, 2020, 146: 66-73. doi: 10.1016/j.resuscitation.2019.10.036
[7] Grasner JT, Meybohm P, Lefering R, et al. ROSC after cardiac arrest--the RACA score to predict outcome after out-of-hospital cardiac arrest[J]. Eur Heart J, 2011, 32(13): 1649-1656. doi: 10.1093/eurheartj/ehr107
[8] Amnuaypattanapon K, Thanachartwet V, Desakorn V, et al. Predictive model of return of spontaneous circulation among patients with out-of-hospital cardiac arrest in Thailand: The WATCH-CPR Score[J]. Int J Clin Pract, 2020, 74(7): e13502.
[9] Huabbangyang T, Silakoon A, Papukdee P, et al. Sustained Return of Spontaneous Circulation Following Out-of-Hospital Cardiac Arrest; Developing a Predictive Model Based on Multivariate Analysis[J]. Arch Acad Emerg Med, 2023, 11(1): e33.
[10] Adnet F, Triba M N, Borron SW, et al. Cardiopulmonary resuscitation duration and survival in out-of-hospital cardiac arrest patients[J]. Resuscitation, 2017, 111: 74-81. doi: 10.1016/j.resuscitation.2016.11.024
[11] 张华忠, 梅勇, 吕金如, 等. 40例体外膜肺氧合辅助心肺复苏治疗成人院外心脏骤停的回顾性分析[J]. 中华急诊医学杂志, 2022, 31(12): 1618-1622.
[12] 朱瑞秋, 叶志钢, 刘长智, 等. 区域性复苏中心体外心肺复苏治疗难治性心脏骤停的回顾性分析[J]. 中国急救医学, 2023, 43(8): 643-646. https://www.cnki.com.cn/Article/CJFDTOTAL-ZJJY202308010.htm
[13] 武小娟, 孟舰, 刘红新, 等. 心脏骤停心肺复苏术中"生存链"实施现状及患者预后因素分析[J]. 临床急诊杂志, 2022, 23(3): 198-203. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2022.03.007
[14] Tanguay-Rioux X, Grunau B, Neumar R, et al. Is initial rhythm in OHCA a predictor of preceding no flow time? Implications for bystander response and ECPR candidacy evaluation[J]. Resuscitation, 2018, 128: 88-92. doi: 10.1016/j.resuscitation.2018.05.002
[15] Callans DJ. Out-of-hospital cardiac arrest--the solution is shocking[J]. N Engl J Med, 2004, 351(7): 632-634. doi: 10.1056/NEJMp048174
[16] Hagihara A, Onozuka D, Ono J, et al. Interaction of defibrillation waveform with the time to defibrillation or the number of defibrillation attempts on survival from out-of-hospital cardiac arrest[J]. Resuscitation, 2018, 122: 54-60. doi: 10.1016/j.resuscitation.2017.11.053
[17] Tateishi K, Saito Y, Kitahara H, et al. Impact of number of defibrillation attempts on neurologically favourable survival rate in patients with Out-of-Hospital cardiac arrest[J]. Resuscitation, 2023, 186: 109779. doi: 10.1016/j.resuscitation.2023.109779
[18] 李博, 王旭垠, 房磊, 等. 心脏骤停后综合征患者72 h死亡危险因素分析[J]. 宁夏医学杂志, 2021, 43(7): 632-633. https://www.cnki.com.cn/Article/CJFDTOTAL-NXYX202107022.htm
[19] Holmen J, Hollenberg J, Claesson A, et al. Survival in ventricular fibrillation with emphasis on the number of defibrillations in relation to other factors at resuscitation[J]. Resuscitation, 2017, 113: 33-38. doi: 10.1016/j.resuscitation.2017.01.006
[20] Ong ME, Shin SD, De Souza NN, et al. Outcomes for out-of-hospital cardiac arrests across 7 countries in Asia: The Pan Asian Resuscitation Outcomes Study(PAROS)[J]. Resuscitation, 2015, 96: 100-108.
[21] Cournoyer A, Grunau B, Cheskes S, et al. Clinical outcomes following out-of-hospital cardiac arrest: The minute-by-minute impact of bystander cardiopulmonary resuscitation[J]. Resuscitation, 2023, 185: 109693. doi: 10.1016/j.resuscitation.2023.109693
[22] Song J, Guo W, Lu X, et al. The effect of bystander cardiopulmonary resuscitation on the survival of out-of-hospital cardiac arrests: a systematic review and meta-analysis[J]. Scand J Trauma Resusc Emerg Med, 2018, 26(1): 86. doi: 10.1186/s13049-018-0552-8
[23] Zhou G, Wang Y, Sun Z, et al. Survival outcome among patients with out-of-hospital cardiac arrest who received cardiopulmonary resuscitation in China: a systematic review and meta-analysis[J]. Eur J Med Res, 2023, 28(1): 8. doi: 10.1186/s40001-022-00955-x
[24] Perkins GD, Ji C, Deakin CD, et al. A Randomized Trial of Epinephrine in Out-of-Hospital Cardiac Arrest[J]. N Engl J Med, 2018, 379(8): 711-721. doi: 10.1056/NEJMoa1806842
[25] Lin S, Callaway CW, Shah PS, et al. Adrenaline for out-of-hospital cardiac arrest resuscitation: a systematic review and meta-analysis of randomized controlled trials[J]. Resuscitation, 2014, 85(6): 732-740. doi: 10.1016/j.resuscitation.2014.03.008
[26] 王立祥, 孟庆义, 余涛. 2016中国心肺复苏专家共识[J]. 中华危重病急救医学, 2016, 28(12): 1059-1079. https://www.cnki.com.cn/Article/CJFDTOTAL-ZJJY202308002.htm
[27] 兰超, 王超, 吕震宇, 等. 多巴胺对兔心肺复苏早期血流动力学及脑氧代谢的影响[J]. 中华急诊医学杂志, 2018, 27(1): 51-56. https://cdmd.cnki.com.cn/Article/CDMD-10459-1018109828.htm
-




 下载:
下载: