Expert consensus on the diagnosis and treatment of traumatic hemorrhagic shock in China(2023)
-
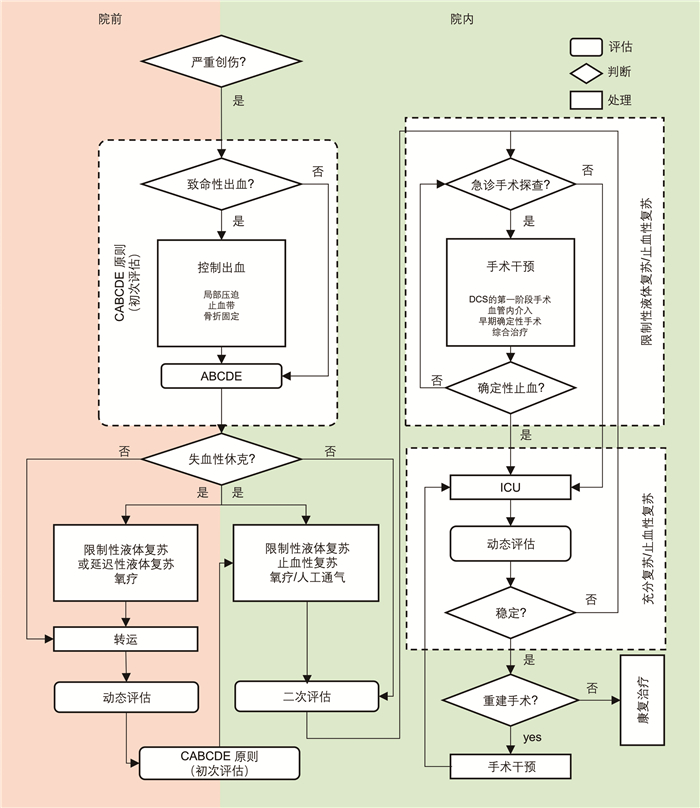
摘要: 创伤失血性休克是严重创伤后“可预防性死亡”的主要原因。目前我国创伤失血性休克诊疗的规范性仍有待提高,为此我们组织了国内多个学术组织的急诊专家,基于最新的临床与基础研究证据,权衡患者获益程度,编写了适用于院前急救、院内救治等创伤失血性休克不同阶段的专家共识,旨在为中国急诊医生规范救治创伤失血性休克患者提供系统、全面的参考依据。Abstract: Hemorrhagic shock remains a leading cause of "potentially preventable death" among severe traumatic injured patients. However, the current situation regarding the diagnosis and treatment of traumatic hemorrhagic shock in our country is not ideal. To standardize and improve the level of diagnosis and treatment of traumatic hemorrhagic shock in China, it is necessary to establish a consensus that is practical and adapted to the conditions in China. We estimated value of the latest clinical and research evidence in given clinical scenarios by a joint committee of multidisciplinary experts. This expert consensus addresses the diagnosis, on-site emergency procedures, in-hospital treatment, and complications prevention of traumatic hemorrhagic shock.
-
Key words:
- traumatic hemorrhagic shock /
- diagnosis /
- treatment /
- expert consensus
-

-
表 1 本共识中采用的临床证据分级标准
推荐等级 各等级代表的意义 收益、风险与负担之间的关系 支持证据的文献质量 1A 推荐力度大;证据质量高 收益明显大于风险和负担,反之亦然 无重要限制的随机对照研究或具有压倒性证据的观察研究 1B 推荐力度大;证据质量中等 收益明显大于风险和负担,反之亦然 有重要限制的随机对照研究或具有高质量证据的观察研究 1C 推荐力度大;证据质量低或极低 收益明显大于风险和负担,反之亦然 观察性研究或病例分析 2A 推荐力度小;证据质量高 收益与风险、负担持平 无重要限制的随机对照研究或具有压倒性证据的观察研究 2B 推荐力度小;证据质量中等 收益与风险、负担持平 有重要限制的随机对照研究或具有高质量证据的观察研究 2C 推荐力度小;证据质量低或极低 无法评估收益、风险与负担之间的关系;收益、风险与负担之间可能持平 观察性研究或病例分析 表 2 创伤失血性休克严重程度分级
SI 预计失血量/% 严重程度 ≥1.0 20~30 轻度 ≥1.5 30~50 中度 ≥2.0 50~70 重度 -
[1] Celso B, Tepas J, Langland-Orban B, et al. A systematic review and meta-analysis comparing outcome of severely injured patients treated in trauma centers following the establishment of trauma systems[J]. J Trauma, 2006, 60(2): 371-378, discussion 378. doi: 10.1097/01.ta.0000197916.99629.eb
[2] 中国医师协会急诊分会, 中国人民解放军急救医学专业委员会, 中国人民解放军重症医学专业委员会, 等. 创伤失血性休克诊治中国急诊专家共识[J]. 临床急诊杂志, 2017, 18(12): 881-889. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2017.12.001
[3] Warren J, Moazzez A, Chong V, et al. Narrowed pulse pressure predicts massive transfusion and emergent operative intervention following penetrating trauma[J]. Am J Surg, 2019, 218(6): 1185-1188. doi: 10.1016/j.amjsurg.2019.08.022
[4] Cannon JW. Hemorrhagic Shock[J]. N Engl J Med, 2018, 378(4): 370-379. doi: 10.1056/NEJMra1705649
[5] Olaussen A, Blackburn T, Mitra B, et al. Review article: shock index for prediction of critical bleeding post-trauma: a systematic review[J]. Emerg Med Australas, 2014, 26(3): 223-228. doi: 10.1111/1742-6723.12232
[6] Drew B, Montgomery HR, Butler FK Jr. Tactical Combat Casualty Care(TCCC)Guidelines for Medical Personnel: 05 November 2020[J]. J Spec Oper Med, 2020, 20(4): 144-151. doi: 10.55460/RBRA-WMWV
[7] Mutschler M, Nienaber U, Brockamp T, et al. A critical reappraisal of the ATLS classification of hypovolaemic shock: does it really reflect clinical reality?[J]. Resuscitation, 2013, 84(3): 309-313. doi: 10.1016/j.resuscitation.2012.07.012
[8] Bulger EM, Snyder D, Schoelles K, et al. An evidence-based prehospital guideline for external hemorrhage control: American College of Surgeons Committee on Trauma[J]. Prehosp Emerg Care, 2014, 18(2): 163-173. doi: 10.3109/10903127.2014.896962
[9] Van Waes OJ, Cheriex KC, Navsaria PH, et al. Management of penetrating neck injuries[J]. Br J Surg, 2012, 99(Suppl 1): 149-154.
[10] Nowicki JL, Stew B, Ooi E. Penetrating neck injuries: a guide to evaluation and management[J]. Ann R Coll Surg Engl, 2018, 100(1): 6-11. doi: 10.1308/rcsann.2017.0191
[11] Eilertsen KA, Winberg M, Jeppesen E, et al. Prehospital Tourniquets in Civilians: A Systematic Review[J]. Prehosp Disaster Med, 2021, 36(1): 86-94. doi: 10.1017/S1049023X20001284
[12] Doyle GS, Taillac PP. Tourniquets: a review of current use with proposals for expanded prehospital use[J]. Prehosp Emerg Care, 2008, 12(2): 241-256. doi: 10.1080/10903120801907570
[13] Levy MJ, Pasley J, Remick KN, et al. Removal of the Prehospital Tourniquet in the Emergency Department[J]. J Emerg Med, 2021, 60(1): 98-102. doi: 10.1016/j.jemermed.2020.10.018
[14] Coccolini F, Stahel PF, Montori G, et al. Pelvic trauma: WSES classification and guidelines[J]. World J Emerg Surg, 2017, 12(1): 5. doi: 10.1186/s13017-017-0117-6
[15] Mayglothling J, Duane TM, Gibbs M, et al. Emergency tracheal intubation immediately following traumatic injury: an Eastern Association for the Surgery of Trauma practice management guideline[J]. J Trauma Acute Care Surg, 2012, 73(5 Suppl 4): S333-S340.
[16] Page D, Ablordeppey E, Wessman BT, et al. Emergency department hyperoxia is associated with increased mortality in mechanically ventilated patients: a cohort study[J]. Crit Care, 2018, 22(1): 9. doi: 10.1186/s13054-017-1926-4
[17] Bernard SA, Nguyen V, Cameron P, et al. Prehospital rapid sequence intubation improves functional outcome for patients with severe traumatic brain injury: a randomized controlled trial[J]. Ann Surg, 2010, 252(6): 959-965. doi: 10.1097/SLA.0b013e3181efc15f
[18] Chu DK, Kim LH, Young PJ, et al. Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy(IOTA): a systematic review and meta-analysis[J]. Lancet, 2018, 391(10131): 1693-1705. doi: 10.1016/S0140-6736(18)30479-3
[19] Davis DP. Early ventilation in traumatic brain injury[J]. Resuscitation, 2008, 76(3): 333-340. doi: 10.1016/j.resuscitation.2007.08.004
[20] Ruelas OS, Tschautscher CF, Lohse CM, et al. Analysis of Prehospital Scene Times and Interventions on Mortality Outcomes in a National Cohort of Penetrating and Blunt Trauma Patients[J]. Prehosp Emerg Care, 2018, 22(6): 691-697. doi: 10.1080/10903127.2018.1448494
[21] Nasser A, Nederpelt C, El Hechi M, et al. Every minute counts: The impact of pre-hospital response time and scene time on mortality of penetrating trauma patients[J]. Am J Surg, 2020, 220(1): 240-244. doi: 10.1016/j.amjsurg.2019.11.018
[22] Harmsen AM, Giannakopoulos GF, Moerbeek PR, et al. The influence of prehospital time on trauma patients outcome: a systematic review[J]. Injury, 2015, 46(4): 602-609. doi: 10.1016/j.injury.2015.01.008
[23] Caputo LM, Salottolo KM, Slone DS, et al. The relationship between patient volume and mortality in American trauma centres: a systematic review of the evidence[J]. Injury, 2014, 45(3): 478-486. doi: 10.1016/j.injury.2013.09.038
[24] Benz D, Balogh ZJ. Damage control surgery: current state and future directions[J]. Curr Opin Crit Care, 2017, 23(6): 491-497. doi: 10.1097/MCC.0000000000000465
[25] Ball CG. Damage control surgery[J]. Curr Opin Crit Care, 2015, 21(6): 538-543. doi: 10.1097/MCC.0000000000000252
[26] Roberts DJ, Bobrovitz N, Zygun DA, et al. Evidence for use of damage control surgery and damage control interventions in civilian trauma patients: a systematic review[J]. World J Emerg Surg, 2021, 16(1): 10. doi: 10.1186/s13017-021-00352-5
[27] Hagiwara A, Fukushima H, Murata A, et al. Blunt splenic injury: usefulness of transcatheter arterial embolization in patients with a transient response to fluid resuscitation[J]. Radiology, 2005, 235(1): 57-64. doi: 10.1148/radiol.2351031132
[28] Manzano Nunez R, Naranjo MP, Foianini E, et al. A meta-analysis of resuscitative endovascular balloon occlusion of the aorta(REBOA)or open aortic cross-clamping by resuscitative thoracotomy in non-compressible torso hemorrhage patients[J]. World J Emerg Surg, 2017, 12: 30. doi: 10.1186/s13017-017-0142-5
[29] Kinslow K, Shepherd A, McKenney M, et al. Resuscitative Endovascular Balloon Occlusion of Aorta: A Systematic Review[J]. Am Surg, 2022, 88(2): 289-296. doi: 10.1177/0003134820972985
[30] Jamal L, Saini A, Quencer K, et al. Emerging approaches to pre-hospital hemorrhage control: a narrative review[J]. Ann Transl Med, 2021, 9(14): 1192. doi: 10.21037/atm-20-5452
[31] 张沂南, 叶雄俊, 闫伟, 等. 注射用白眉蛇毒血凝酶局部应用对泌尿外科腹腔镜手术: 创面止血效果的多中心研究[J]. 泌尿外科杂志(电子版), 2020, 12(3): 13-20. doi: 10.3969/j.issn.1674-7410.2020.03.003
[32] Toth L, King KL, McGrath B, et al. Efficacy and safety of emergency non-invasive pelvic ring stabilisation[J]. Injury, 2012, 43(8): 1330-1334. doi: 10.1016/j.injury.2012.05.014
[33] Tötterman A, Madsen JE, Skaga NO, et al. Extraperitoneal pelvic packing: a salvage procedure to control massive traumatic pelvic hemorrhage[J]. J Trauma, 2007, 62(4): 843-852.
[34] Matsumoto H, Hara Y, Yagi T, et al. Impact of urgent resuscitative surgery for life-threatening torso trauma[J]. Surg Today, 2017, 47(7): 827-835. doi: 10.1007/s00595-016-1451-0
[35] Thorson CM, Van Haren RM, Ryan ML, et al. Admission hematocrit and transfusion requirements after trauma[J]. J Am Coll Surg, 2013, 216(1): 65-73. doi: 10.1016/j.jamcollsurg.2012.09.011
[36] Thorson CM, Ryan ML, Van Haren RM, et al. Change in hematocrit during trauma assessment predicts bleeding even with ongoing fluid resuscitation[J]. Am Surg, 2013, 79(4): 398-406. doi: 10.1177/000313481307900430
[37] Kobayashi L, Coimbra R, Goes A Jr, et al. American Association for the Surgery of Trauma-World Society of Emergency Surgery guidelines on diagnosis and management of abdominal vascular injuries[J]. J Trauma Acute Care Surg, 2020, 89(6): 1197-1211. doi: 10.1097/TA.0000000000002968
[38] Mutschler M, Nienaber U, Brockamp T, et al. Renaissance of base deficit for the initial assessment of trauma patients: a base deficit-based classification for hypovolemic shock developed on data from 16, 305 patients derived from the TraumaRegister DGU®[J]. Crit Care, 2013, 17(2): R42. doi: 10.1186/cc12555
[39] Herbert HK, Dechert TA, Wolfe L, et al. Lactate in trauma: a poor predictor of mortality in the setting of alcohol ingestion[J]. Am Surg, 2011, 77(12): 1576-1579. doi: 10.1177/000313481107701224
[40] Mohamed M, Majeske K, Sachwani GR, et al. The impact of early thromboelastography directed therapy in trauma resuscitation[J]. Scand J Trauma Resusc Emerg Med, 2017, 25(1): 99. doi: 10.1186/s13049-017-0443-4
[41] Albert V, Subramanian A, Pati HP, et al. Efficacy of Thromboelastography(TEG)in Predicting Acute Trauma-Induced Coagulopathy(ATIC)in Isolated Severe Traumatic Brain Injury(iSTBI)[J]. Indian J Hematol Blood Transfus, 2019, 35(2): 325-331. doi: 10.1007/s12288-018-1003-4
[42] Dixon AL, McCully BH, Rick EA, et al. Tranexamic acid administration in the field does not affect admission thromboelastography after traumatic brain injury[J]. J Trauma Acute Care Surg, 2020, 89(5): 900-907. doi: 10.1097/TA.0000000000002932
[43] Murao S, Yamakawa K, Kabata D, et al. Effect of Earlier Door-to-CT and Door-to-Bleeding Control in Severe Blunt Trauma: A Retrospective Cohort Study[J]. J Clin Med, 2021, 10(7): 1522. doi: 10.3390/jcm10071522
[44] Magyar C, Maeder F, Diepers M, et al. Detailed information gain and therapeutic impact of whole body computed tomography supplementary to conventional radiological diagnostics in blunt trauma emergency treatment: a consecutive trauma centre evaluation[J]. Eur J Trauma Emerg Surg, 2022, 48(2): 921-931. doi: 10.1007/s00068-020-01502-1
[45] Do WS, Chang R, Fox EE, et al. Too fast, or not fast enough? The FAST exam in patients with non-compressible torso hemorrhage[J]. Am J Surg, 2019, 217(5): 882-886. doi: 10.1016/j.amjsurg.2019.02.012
[46] Moore CL, Copel JA. Point-of-care ultrasonography[J]. N Engl J Med, 2011, 364(8): 749-757. doi: 10.1056/NEJMra0909487
[47] Mercer CB, Ball M, Cash RE, et al. Ultrasound Use in the Prehospital Setting for Trauma: A Systematic Review[J]. Prehosp Emerg Care, 2021, 25(4): 566-582. doi: 10.1080/10903127.2020.1811815
[48] Barbar SD, Clere-Jehl R, Bourredjem A, et al. Timing of Renal-Replacement Therapy in Patients with Acute Kidney Injury and Sepsis[J]. N Engl J Med, 2018, 379(15): 1431-1442. doi: 10.1056/NEJMoa1803213
[49] Samuels JM, Moore HB, Moore EE. Damage Control Resuscitation[J]. Chirurgia(Bucur), 2017, 112: 514-523.
[50] Cole E, Weaver A, Gall L, et al. A Decade of Damage Control Resuscitation: New Transfusion Practice, New Survivors, New Directions[J]. Ann Surg, 2021, 273(6): 1215-1220. doi: 10.1097/SLA.0000000000003657
[51] Leibner E, Andreae M, Galvagno SM, et al. Damage control resuscitation[J]. Clin Exp Emerg Med, 2020, 7(1): 5-13. doi: 10.15441/ceem.19.089
[52] Abdelmalik PA, Draghic N, Ling GSF. Management of moderate and severe traumatic brain injury[J]. Transfusion, 2019, 59(S2): 1529-1538. doi: 10.1111/trf.15171
[53] Geeraerts T, Velly L, Abdennour L, et al. Management of severe traumatic brain injury(first 24hours)[J]. Anaesth Crit Care Pain Med, 2018, 37(2): 171-186. doi: 10.1016/j.accpm.2017.12.001
[54] Eastridge BJ, Holcomb JB, Shackelford S. Outcomes of traumatic hemorrhagic shock and the epidemiology of preventable death from injury[J]. Transfusion, 2019, 59(S2): 1423-1428. doi: 10.1111/trf.15161
[55] Siegemund M, Hollinger A, Gebhard EC, et al. The value of volume substitution in patients with septic and haemorrhagic shock with respect to the microcirculation[J]. Swiss Med Wkly, 2019, 149: w20007.
[56] Hussmann B, Lefering R, Kauther MD, et al. Influence of prehospital volume replacement on outcome in polytraumatized children[J]. Crit Care, 2012, 16(5): R201. doi: 10.1186/cc11809
[57] Hussmann B, Lefering R, Waydhas C, et al. Does increased prehospital replacement volume lead to a poor clinical course and an increased mortality? A matched-pair analysis of 1896 patients of the Trauma Registry of the German Society for Trauma Surgery who were managed by an emergency doctor at the accident site[J]. Injury, 2013, 44(5): 611-617. doi: 10.1016/j.injury.2012.02.004
[58] Hussmann B, Schoeneberg C, Jungbluth P, et al. Enhanced prehospital volume therapy does not lead to improved outcomes in severely injured patients with severe traumatic brain injury[J]. BMC Emerg Med, 2019, 19(1): 13. doi: 10.1186/s12873-019-0221-x
[59] 王坤, 杨萍芬, 严浩. 骨髓腔穿刺输液在院外创伤失血性休克患者抢救中的应用效果[J]. 中国急救复苏与灾害医学杂志, 2020, 15(3): 288-290.
[60] Crowe E, DeSantis SM, Bonnette A, et al. Whole blood transfusion versus component therapy in trauma resuscitation: a systematic review and meta-analysis[J]. J Am Coll Emerg Physicians Open, 2020, 1(4): 633-641. doi: 10.1002/emp2.12089
[61] Crombie N, Doughty HA, Bishop J, et al. Resuscitation with blood products in patients with trauma-related haemorrhagic shock receiving prehospital care(RePHILL): a multicentre, open-label, randomised, controlled, phase 3 trial[J]. Lancet Haematol, 2022, 9(4): e250-e261. doi: 10.1016/S2352-3026(22)00040-0
[62] Sperry JL, Guyette FX, Brown JB, et al. Prehospital Plasma during Air Medical Transport in Trauma Patients at Risk for Hemorrhagic Shock[J]. N Engl J Med, 2018, 379(4): 315-326. doi: 10.1056/NEJMoa1802345
[63] Hilbert-Carius P, Schwarzkopf D, Reinhart K, et al. Synthetic colloid resuscitation in severely injured patients: analysis of a nationwide trauma registry(TraumaRegister DGU)[J]. Sci Rep, 2018, 8(1): 11567. doi: 10.1038/s41598-018-30053-0
[64] Semler MW, Self WH, Wanderer JP, et al. Balanced Crystalloids versus Saline in Critically Ill Adults[J]. N Engl J Med, 2018, 378(9): 829-839. doi: 10.1056/NEJMoa1711584
[65] Didwania A, Miller J, Kassel D, et al. Effect of intravenous lactated Ringer's solution infusion on the circulating lactate concentration: Part 3. Results of a prospective, randomized, double-blind, placebo-controlled trial[J]. Crit Care Med, 1997, 25(11): 1851-1854. doi: 10.1097/00003246-199711000-00024
[66] Zitek T, Skaggs ZD, Rahbar A, et al. Does Intravenous Lactated Ringer's Solution Raise Serum Lactate?[J]. J Emerg Med, 2018, 55(3): 313-318. doi: 10.1016/j.jemermed.2018.05.031
[67] Wang L, Lou J, Cao J, et al. Bicarbonate Ringer's solution for early resuscitation in hemorrhagic shock rabbits[J]. Ann Transl Med, 2021, 9(6): 462. doi: 10.21037/atm-21-97
[68] Rowell SE, Fair KA, Barbosa RR, et al. The Impact of Pre-Hospital Administration of Lactated Ringer's Solution versus Normal Saline in Patients with Traumatic Brain Injury[J]. J Neurotrauma, 2016, 33(11): 1054-1059. doi: 10.1089/neu.2014.3478
[69] Zampieri FG, Machado FR, Biondi RS, et al. Effect of Intravenous Fluid Treatment With a Balanced Solution vs 0.9% Saline Solution on Mortality in Critically Ill Patients: The BaSICS Randomized Clinical Trial[J]. JAMA, 2021, 326(9): 1-12.
[70] Foster JC, Sappenfield JW, Smith RS, et al. Initiation and Termination of Massive Transfusion Protocols: Current Strategies and Future Prospects[J]. Anesth Analg, 2017, 125(6): 2045-2055. doi: 10.1213/ANE.0000000000002436
[71] Callcut RA, Cripps MW, Nelson MF, et al. The Massive Transfusion Score as a decision aid for resuscitation: Learning when to turn the massive transfusion protocol on and off[J]. J Trauma Acute Care Surg, 2016, 80(3): 450-456. doi: 10.1097/TA.0000000000000914
[72] Kheirbek T, Martin TJ, Cao J, et al. Prehospital shock index outperforms hypotension alone in predicting significant injury in trauma patients[J]. Trauma Surg Acute Care Open, 2021, 6(1): e000712. doi: 10.1136/tsaco-2021-000712
[73] Black JA, Pierce VS, Kerby JD, et al. The Evolution of Blood Transfusion in the Trauma Patient: Whole Blood Has Come Full Circle[J]. Semin Thromb Hemost, 2020, 46(2): 215-220. doi: 10.1055/s-0039-3402426
[74] Holcomb JB, Tilley BC, Baraniuk S, et al. Transfusion of plasma, platelets, and red blood cells in a 1 : 1 : 1 vs a 1 : 1 : 2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial[J]. JAMA, 2015, 313(5): 471-482. doi: 10.1001/jama.2015.12
[75] Kelly JM, Callum JL, Rizoli SB. 1 : 1 : 1-Warranted or wasteful? Even where appropriate, high ratio transfusion protocols are costly: early transition to individualized care benefits patients and transfusion services[J]. Expert Rev Hematol, 2013, 6(6): 631-633. doi: 10.1586/17474086.2013.859520
[76] Moore HB, Tessmer MT, Moore EE, et al. Forgot calcium? Admission ionized-calcium in two civilian randomized controlled trials of prehospital plasma for traumatic hemorrhagic shock[J]. J Trauma Acute Care Surg, 2020, 88(5): 588-596. doi: 10.1097/TA.0000000000002614
[77] Prat NJ, Meyer AD, Ingalls NK, et al. Rotational thromboelastometry significantly optimizes transfusion practices for damage control resuscitation in combat casualties[J]. J Trauma Acute Care Surg, 2017, 83(3): 373-380. doi: 10.1097/TA.0000000000001568
[78] Wikkelsø A, Wetterslev J, Møller AM, et al. Thromboelastography(TEG)or thromboelastometry(ROTEM) to monitor haemostatic treatment versus usual care in adults or children with bleeding[J]. Cochrane Database Syst Rev, 2016, 2016(8): CD007871.
[79] McQuilten ZK, Crighton G, Brunskill S, et al. Optimal Dose, Timing and Ratio of Blood Products in Massive Transfusion: Results from a Systematic Review[J]. Transfus Med Rev, 2018, 32(1): 6-15. doi: 10.1016/j.tmrv.2017.06.003
[80] Aoki M, Abe T, Saitoh D, et al. Use of Vasopressor Increases the Risk of Mortality in Traumatic Hemorrhagic Shock: A Nationwide Cohort Study in Japan[J]. Crit Care Med, 2018, 46(12): e1145-e1151. doi: 10.1097/CCM.0000000000003428
[81] Sims CA, Holena D, Kim P, et al. Effect of Low-Dose Supplementation of Arginine Vasopressin on Need for Blood Product Transfusions in Patients With Trauma and Hemorrhagic Shock: A Randomized Clinical Trial[J]. JAMA Surg, 2019, 154(11): 994-1003. doi: 10.1001/jamasurg.2019.2884
[82] Spahn DR, Bouillon B, Cerny V, et al. The European guideline on management of major bleeding and coagulopathy following trauma: fifth edition[J]. Crit Care, 2019, 23(1): 98. doi: 10.1186/s13054-019-2347-3
[83] Rhodes A, Evans LE, Alhazzani W, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016[J]. Crit Care Med, 2017, 45(3): 486-552. doi: 10.1097/CCM.0000000000002255
[84] Kutcher ME, Howard BM, Sperry JL, et al. Evolving beyond the vicious triad: Differential mediation of traumatic coagulopathy by injury, shock, and resuscitation[J]. J Trauma Acute Care Surg, 2015, 78(3): 516-523. doi: 10.1097/TA.0000000000000545
[85] Prevaldi C, Paolillo C, Locatelli C, et al. Management of traumatic wounds in the Emergency Department: position paper from the Academy of Emergency Medicine and Care(AcEMC)and the World Society of Emergency Surgery(WSES)[J]. World J Emerg Surg, 2016, 11: 30. doi: 10.1186/s13017-016-0084-3
[86] Schauer SG, Naylor JF, Maddry JK, et al. Trends in Prehospital Analgesia Administration by US Forces From 2007 Through 2016[J]. Prehosp Emerg Care, 2019, 23(2): 271-276. doi: 10.1080/10903127.2018.1489022
[87] Moore HB, Gando S, Iba T, et al. Defining trauma-induced coagulopathy with respect to future implications for patient management: Communication from the SSC of the ISTH[J]. J Thromb Haemost, 2020, 18(3): 740-747. doi: 10.1111/jth.14690
[88] Moore HB, Walsh M, Kwaan HC, et al. The Complexity of Trauma-Induced Coagulopathy[J]. Semin Thromb Hemost, 2020, 46(2): 114-115. doi: 10.1055/s-0040-1702202
[89] Moore EE, Moore HB, Kornblith LZ, et al. Trauma-induced coagulopathy[J]. Nat Rev Dis Primers, 2021, 7(1): 30. doi: 10.1038/s41572-021-00264-3
[90] Duque P, Calvo A, Lockie C, et al. Pathophysiology of Trauma-Induced Coagulopathy[J]. Transfus Med Rev, 2021, 35(4): 80-86. doi: 10.1016/j.tmrv.2021.07.004
[91] Petros S. Trauma-Induced Coagulopathy[J]. Hamostaseologie, 2019, 39(1): 20-27. doi: 10.1055/s-0039-1677853
[92] Shakur H, Roberts I, Bautista R, et al. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage(CRASH-2): a randomised, placebo-controlled trial[J]. Lancet, 2010, 376(9734): 23-32. doi: 10.1016/S0140-6736(10)60835-5
[93] CRASH-3 trial collaborators. Effects of tranexamic acid on death, disability, vascular occlusive events and other morbidities in patients with acute traumatic brain injury(CRASH-3): a randomised, placebo-controlled trial[J]. Lancet, 2019, 394(10210): 1713-1723. doi: 10.1016/S0140-6736(19)32233-0
[94] Moore EE, Moore HB, Gonzalez E, et al. Rationale for the selective administration of tranexamic acid to inhibit fibrinolysis in the severely injured patient[J]. Transfusion, 2016, 56 Suppl 2: S110-S114.
[95] Zhang P, Lv H, Qi X, et al. Effect of ulinastatin on post-operative blood loss and allogeneic transfusion in patients receiving cardiac surgery with cardiopulmonary bypass: a prospective randomized controlled study with 10-year follow-up[J]. J Cardiothorac Surg, 2020, 15(1): 98. doi: 10.1186/s13019-020-01144-9
[96] Moore HB, Moore EE. Temporal Changes in Fibrinolysis following Injury[J]. Semin Thromb Hemost, 2020, 46(2): 189-198. doi: 10.1055/s-0039-1701016
[97] Coleman JR, Kay AB, Moore EE, et al. It's sooner than you think: Blunt solid organ injury patients are already hypercoagulable upon hospital admission-Results of a bi-institutional, prospective study[J]. Am J Surg, 2019, 218(6): 1065-1073. doi: 10.1016/j.amjsurg.2019.08.024
-




 下载:
下载: