Correlation analysis of lactate dehydrogenase/albumin ratio, monocyte/lymphocyte ratio with disease and prognosis of trauma-related ARDS patients
-
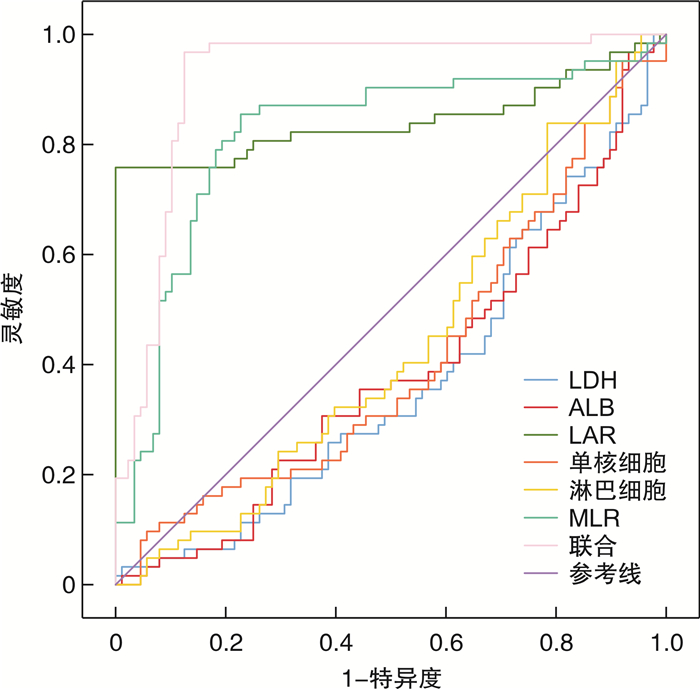
摘要: 目的 探讨乳酸脱氢酶/白蛋白比值(lactate dehydrogenase/albumin ratio,LAR)、单核细胞/淋巴细胞比值(monocyte/lymphocyte ratio,MLR)与创伤相关急性呼吸窘迫综合征(acute respiratory distress syndrome, ARDS)患者病情以及预后的关系。方法 回顾性选取2020年2月—2023年2月我院收治的150例创伤相关ARDS患者,根据氧合指数(oxygenation index, OI)分为轻度组(51例)、中度组(63例)、重度组(36例),收集临床和实验室资料,计算LAR、MLR,统计住院28 d内ARDS组患者存活情况。分析影响创伤相关ARDS预后的因素以及LAR、MLR预测创伤相关ARDS预后的价值。结果 ARDS组LAR和MLR高于对照组(P<0.05),重度组LAR和MLR高于中度组和轻度组(P<0.05)。多因素logistic回归分析显示高APACHE Ⅱ评分、重度ARDS、高LAR、MLR是创伤相关ARDS患者预后不良的危险因素(P<0.05)。联合LAR和MLR预测创伤相关ARDS患者预后的曲线下面积为0.920,高于LAR、MLR的0.843、0.818(Z=2.035、2.537,P<0.05)。结论 高LAR和MLR与创伤相关ARDS病情加重以及预后不良有关。
-
关键词:
- 急性呼吸窘迫综合征 /
- 乳酸脱氢酶与白蛋白比值 /
- 单核细胞/淋巴细胞比值 /
- 创伤 /
- 预后
Abstract: Objective To investigate the relationship between lactate dehydrogenase/albumin ratio(LAR), monocyte/lymphocyte ratio(MLR) and the condition and prognosis of patients with trauma-related acute respiratory distress syndrome(ARDS).Methods One hundred and fifty patients with trauma-related ARDS admitted to our hospital from February 2020 to February 2023 were retrospectively selected. According to oxygenation index(OI), ARDS patients were divided into mild group(51 cases), moderate group(63 cases) and severe group(36 cases). Clinical and laboratory data were collected, LAR and MLR were calculated, and the survival of ARDS patients within 28 days of hospitalization was analyzed. The prognostic factors of trauma-related ARDS and the prognostic value of LAR and MLR in trauma-related ARDS were analyzed.Results LAR and MLR in ARDS group were higher than those in control group(P < 0.05), LAR and MLR in severe group were higher than those in moderate and mild groups(P < 0.05). Multivariate logistic regression analysis showed that high APACHE Ⅱ score, severe ARDS, high LAR and MLR were risk factors for poor prognosis in trauma-related ARDS patients(P < 0.05). The area under the curve of LAR and MLR in predicting the prognosis of trauma-related ARDS patients was 0.920, which was higher than 0.843 and 0.818 of LAR and MLR(Z=2.035, 2.537, P < 0.05).Conclusion High LAR and MLR are associated with the aggravation and poor prognosis of trauma-related ARDS. -

-
表 1 不同病情严重程度分组LAR、MLR比较
X±S 组别 例数 LDH/(U/L) ALB/(g/L) LAR 单核细胞计数/(×109/L) 淋巴细胞计数/(×109/L) MLR 轻度组 51 379.51±9.32 28.12±1.23 13.50±1.02 1.72±0.13 1.80±0.05 0.96±0.08 中度组 63 436.29±12.691) 30.65±2.031) 14.23±1.151) 2.06±0.331) 2.06±0.121) 1.00±0.101) 重度组 36 470.31±14.121)2) 32.15±1.191)2) 14.63±0.911)2) 2.33±0.061)2) 2.22±0.051)2) 1.05±0.131)2) F 32.652 42.659 15.956 20.491 22.157 19.428 P <0.001 <0.001 <0.001 <0.001 <0.001 <0.001 与轻度组比较,1)P<0.05;与中度组比较,2)P<0.05。 表 2 影响创伤相关ARDS患者预后的单因素
X±S 因素 死亡组(62例) 存活组(88例) t/χ2 P 年龄/岁 48.15±10.29 45.09±8.17 2.027 0.044 性别/例(%) 0.055 0.814 男 39(62.90) 57(64.77) 女 23(37.10) 31(35.23) 创伤类型/例(%) 0.081 0.994 车祸 22(35.48) 33(37.50) 跌打伤 17(27.42) 23(26.14) 割伤 9(14.52) 13(14.77) 挫伤 14(22.58) 19(21.59) ISS评分/分 17.32±3.11 16.53±2.21 1.819 0.071 GOS评分/分 9.21±2.01 9.03±1.86 0.564 0.573 APACHE Ⅱ评分/分 16.32±3.06 13.09±2.37 7.280 <0.001 SOFA评分/分 12.15±2.15 11.79±2.06 1.035 0.303 心率/(次/min) 79.35±6.29 78.04±6.11 1.277 0.204 收缩压/mmHg 129.35±11.27 130.04±11.36 0.368 0.714 舒张压/mmHg 77.04±6.59 77.12±7.32 0.069 0.945 ARDS严重程度/例(%) 7.820 0.020 轻度 19(30.65) 32(36.36) 中度 21(33.87) 42(47.73) 重度 22(35.48) 14(15.91) LDH/(U/L) 439.65±51.31 414.93±42.19 3.229 0.002 ALB/(g/L) 28.65±2.04 31.21±1.97 7.723 <0.001 LAR 14.91±2.02 13.53±2.15 3.968 <0.001 BUN/(mmol/L) 6.32±2.18 6.19±2.05 0.373 0.710 Scr/(μmol/L) 106.24±11.72 105.21±10.69 0.558 0.578 单核细胞计数/(×109/L) 2.19±0.23 1.88±0.20 8.783 <0.001 淋巴细胞计数/(×109/L) 1.93±0.19 2.07±0.23 3.938 <0.001 MLR 1.13±0.11 0.91±0.14 10.327 <0.001 白细胞计数/(×109/L) 12.15±2.06 12.03±2.11 0.347 0.730 是否使用机械通气/例(%) 0.530 0.467 是 43(69.35) 56(63.64) 否 19(30.65) 32(36.36) 是否使用血管加压药/例(%) 11.409 0.001 是 33(53.23) 23(26.14) 否 29(46.77) 65(73.86) 表 3 影响创伤相关ARDS患者预后的logistic回归方程
因素 β SE Wald χ2 OR(95%CI) P 常数项 10.426 3.195 10.649 - <0.001 APACHE Ⅱ评分 0.652 0.274 5.662 1.919(1.122~3.284) 0.012 ARDS病情 1.152 0.412 7.818 3.165(1.411~7.096) 0.002 LAR 0.701 0.298 5.534 2.016(1.124~3.615) 0.018 MLR 0.502 0.156 10.355 1.652(1.217~2.243) <0.001 表 4 LAR、MLR预测创伤相关ARDS患者预后的效能
因素 曲线下面积(95%CI) 临界值 灵敏度/% 特异度/% 约登指数 LDH 0.629(0.546~0.706) 425.13 U/L 33.87 44.32 -0.218 1 ALB 0.613(0.531~0.692) 30.62 g/L 37.10 47.73 -0.151 7 LAR 0.843(0.775~0.897) 14.21 75.81 79.55 0.553 6 单核细胞 0.588(0.505~0.668) 2.03×109/L 37.10 42.05 -0.208 5 淋巴细胞 0.564(0.481~0.645) 2.01×109/L 40.32 45.45 -0.142 3 MLR 0.818(0.747~0.876) 1.06 79.03 81.82 0.608 5 联合 0.920(0.864~0.958) - 96.77 87.50 0.842 7 -
[1] Lupu L, Palmer A, Huber-Lang M. Inflammation, Thrombosis, and Destruction: The Three-Headed Cerberus of Trauma-and SARS-CoV-2-Induced ARDS[J]. Front Immunol, 2020, 11: 584514. doi: 10.3389/fimmu.2020.584514
[2] Spadaro S, Park M, Turrini C, et al. Biomarkers for Acute Respiratory Distress syndrome and prospects for personalised medicine[J]. J Inflamm(Lond), 2019, 16: 1. doi: 10.1186/s12950-018-0202-y
[3] 孔程祥, 李莉, 金萍, 等. 血清白蛋白、乳酸脱氢酶及乳酸脱氢酶/白蛋白比值检测在儿童急性呼吸窘迫综合征诊治中的临床意义[J]. 中国实用医药, 2020, 15(15): 19-21. https://www.cnki.com.cn/Article/CJFDTOTAL-ZSSA202015007.htm
[4] 王梦瑶, 张薇, 郭友芳, 等. 单核细胞/淋巴细胞比值与呼吸系统疾病评估相关性的研究进展[J]. 医学综述, 2021, 27(15): 3045-3049. doi: 10.3969/j.issn.1006-2084.2021.15.025
[5] ARDS Definition Task Force, Ranieri VM, Rubenfeld GD, et al. Acute respiratory distress syndrome: the Berlin Definition[J]. JAMA, 2012, 307(23): 2526-2533.
[6] Hancock A. Parkinsonism together with the "APACHE type" in encephalitis lethargica[J]. Br Med J, 1925, 1(3360): 966. doi: 10.1136/bmj.1.3360.966
[7] Vincent JL, Moreno R, Takala J, et al. The SOFA(Sepsis-related Organ Failure Assessment)score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine[J]. Intensive Care Med, 1996, 22(7): 707-710. doi: 10.1007/BF01709751
[8] Cheng Q, Lai X, Yang L, et al. Serum CD5 L predicts acute lung parenchymal injury and acute respiratory distress syndrome in trauma patients[J]. Medicine(Baltimore), 2021, 100(39): e27219.
[9] Yang L, Gao C, Li F, et al. Monocyte-to-lymphocyte ratio is associated with 28-day mortality in patients with acute respiratory distress syndrome: a retrospective study[J]. J Intensive Care, 2021, 9(1): 49. doi: 10.1186/s40560-021-00564-6
[10] Ding J, Karp JE, Emadi A. Elevated lactate dehydrogenase(LDH)can be a marker of immune suppression in cancer: Interplay between hematologic and solid neoplastic clones and their microenvironments[J]. Cancer Biomark, 2017, 19(4): 353-363. doi: 10.3233/CBM-160336
[11] Kuang ZS, Yang YL, Wei W, et al. Clinical characteristics and prognosis of community-acquired pneumonia in autoimmune disease-induced immunocompromised host: A retrospective observational study[J]. World J Emerg Med, 2020, 11(3): 145-151. doi: 10.5847/wjem.j.1920-8642.2020.03.003
[12] Wu C, Chen X, Cai Y, et al. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China[J]. JAMA Intern Med, 2020, 180(7): 934-943. doi: 10.1001/jamainternmed.2020.0994
[13] Godinez-Vidal AR, Correa-Montoya A, Enríquez-Santos D, et al. Is albumin a predictor of severity and mortality in patients with abdominal sepsis?[J]. Cir Cir, 2019, 87(5): 485-489. http://doc.paperpass.com/foreign/rgArti20194989948.html
[14] Yin M, Si L, Qin W, et al. Predictive Value of Serum Albumin Level for the Prognosis of Severe Sepsis Without Exogenous Human Albumin Administration: A Prospective Cohort Study[J]. J Intensive Care Med, 2018, 33(12): 687-694. doi: 10.1177/0885066616685300
[15] Bou Chebl R, Jamali S, Sabra M, et al. Lactate/Albumin Ratio as a Predictor of In-Hospital Mortality in Septic Patients Presenting to the Emergency Department[J]. Front Med(Lausanne), 2020, 7: 550182.
[16] Jeon SY, Ryu S, Oh SK, et al. Lactate dehydrogenase to albumin ratio as a prognostic factor for patients with severe infection requiring intensive care[J]. Medicine(Baltimore), 2021, 100(41): e27538.
[17] Dang W, Tao Y, Xu X, et al. The role of lung macrophages in acute respiratory distress syndrome[J]. Inflamm Res, 2022, 71(12): 1417-1432. doi: 10.1007/s00011-022-01645-4
[18] Zhang Y, Zhang S. Prognostic value of glucose-to-lymphocyte ratio in critically ill patients with acute respiratory distress syndrome: A retrospective cohort study[J]. J Clin Lab Anal, 2022, 36(5): e24397.
[19] Song C, Li H, Li Y, et al. NETs promote ALI/ARDS inflammation by regulating alveolar macrophage polarization[J]. Exp Cell Res, 2019, 382(2): 111486. doi: 10.1016/j.yexcr.2019.06.031
[20] Zhang S, Chu C, Wu Z, et al. IFIH1 Contributes to M1 Macrophage Polarization in ARDS[J]. Front Immunol, 2020, 11: 580838.
-




 下载:
下载: