Quantitative parameters of phrenic muscle in ICU patients with mechanical ventilation for respiratory failure and their predictive value to the outcome of withdrawal
-
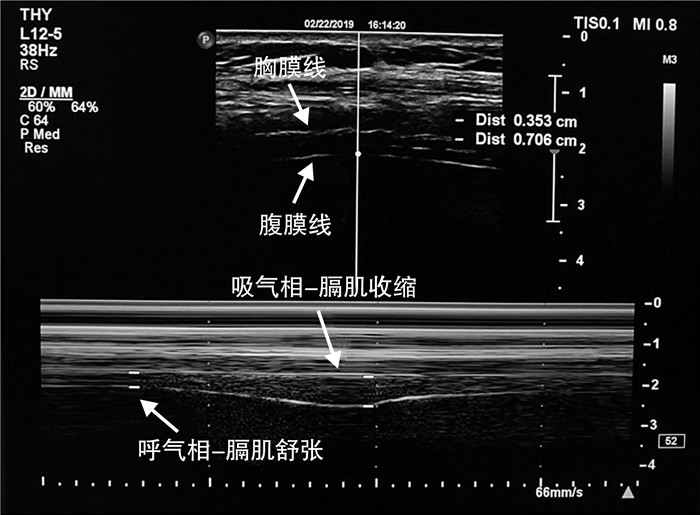
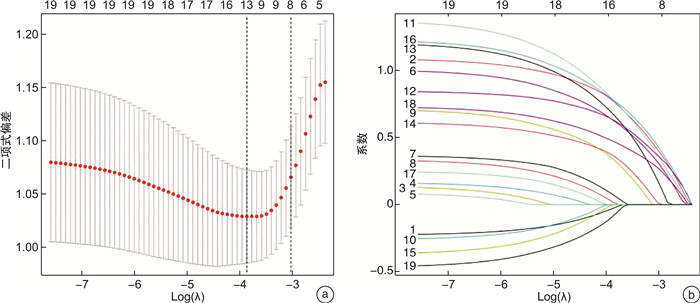
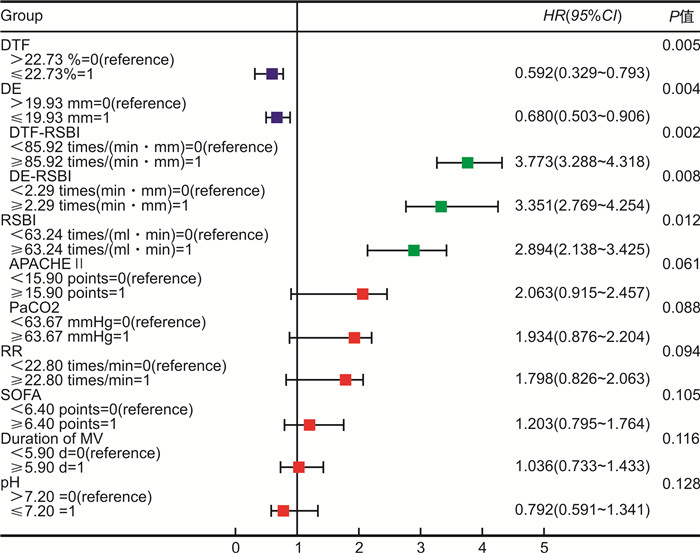
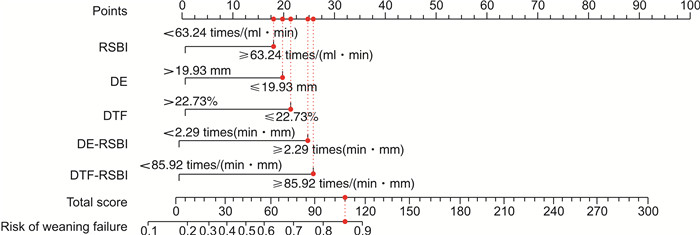
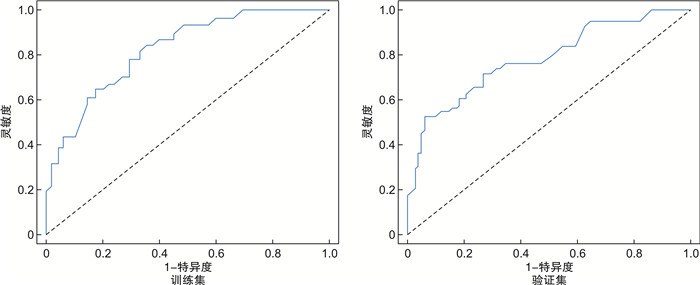
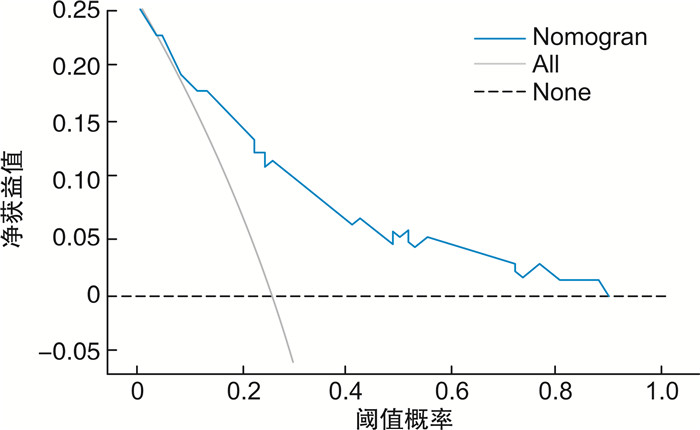
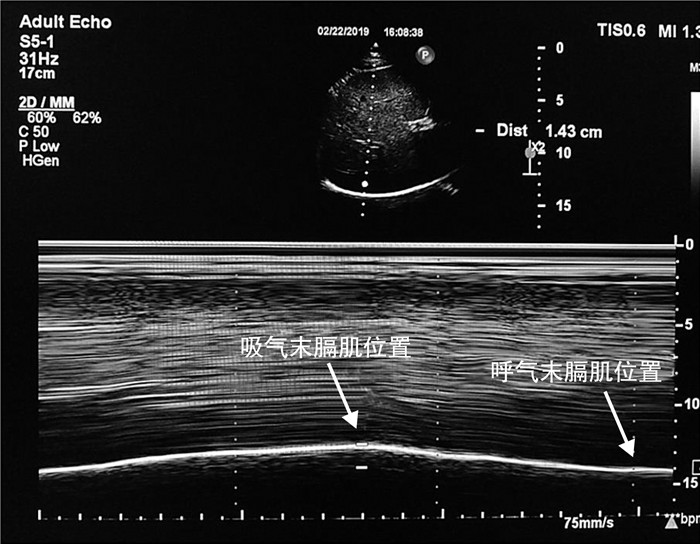
摘要: 目的 探讨重症超声膈肌定量参数对呼吸衰竭患者撤机结局的预测价值。方法 选取2018年1月—2022年6月于我院ICU接受机械通气(mechanical ventilation, MV)治疗的呼吸衰竭患者214例,按7∶3比例随机分为训练集和验证集,其中训练集150例,依据撤呼吸机情况将训练集数据分为撤机失败组(35例)和撤机成功组(115例)。验证集64例,其中撤机失败组(16例)和撤机成功组(48例)。比较训练集两组患者的一般临床资料,并通过LASSO和回归分析筛选危险因素,构建列线图模型,并对模型进行验证。受试者工作特征(receiver operating characteristic,ROC)曲线分析对浅快呼吸指数(rapid shallow breath index, RSBI)、膈肌增厚率(diaphragm thickening fraction,DTF)和膈肌移动度(diaphragmatic excursion,DE)对呼吸衰竭患者撤机结局的预测价值。结果 RSBI、DE、DTF、DE-RSBI、DTF-RSBI均是呼吸衰竭患者撤机失败的独立预测因素(P < 0.05)。RSBI、DE、DTF、DE-RSBI、DTF-RSBI的AUC分别为0.715(95%CI:0.681~0.855)、0.796(95%CI:0.729~0.860)、0.721(95%CI:0.648~0.788)、0.820(95%CI:0.756~0.880)和0.872(95%CI:0.823~0.920)。结论 膈肌超声定量参数DT、DTF联合传统RSBI指标可有效精确预测撤机结局,优于传统RSBI指标,可作为床旁超声评价呼吸衰竭患者撤机流程的新兴手段。Abstract: Objective To explore the prediction of weaning outcome in patients with respiratory failure by quantitative parameters of severe ultrasonic diaphragm.Methods In a prospective study, 214 patients with respiratory failure who were treated with mechanical ventilation(MV) in ICU from January 2018 to June 2022 were randomly divided into training set and verification set according to the proportion of 7∶3. According to the condition of ventilator withdrawal, the data of the training set were divided into failure group(n=35) and successful group(n=115). There were 64 cases in the verification set, including withdrawal failure group(n=16) and successful withdrawal group(n=48). The general clinical data of the two groups were compared, and the risk factors were screened by LASSO and logistic regression analysis. A Nomogram model was constructed based on the screened risk factors, and the model was verified. Receiver operating characteristic(ROC) curve was used to analyze the predictive value of rapid shallow breath index(RSBI), diaphragm thickening fraction(DTF) and diaphragmatic excursion(DE) on weaning outcomes in patients with respiratory failure.Results RSBI, DE, DTF, DE-RSBI and DTF-RSBI were independent predictors of weaning failure in patients with respiratory failure(P < 0.05). The AUC of RSBI, DE, DTF, DE-RSBI and DTF-RSBI was 0.715(95%CI: 0.681-0.855), 0.796(95%CI: 0.729-0.860), 0.721(95%CI: 0.648-0.788), 0.820(95%CI: 0.756-0.880) and 0.872(95%CI: 0.823-0.920), respectively.Conclusion Diaphragm ultrasound quantitative parameters DT and DTF combined with traditional RSBI index can effectively and accurately predict the outcome of weaning, which is better than traditional RSBI index. It can be used as a new method for bedside ultrasound to evaluate the weaning process of patients with respiratory failure.
-

-
表 1 2组一般资料比较
X±S 临床资料 撤机成功组(115例) 撤机失败组(35例) t/χ2 P 年龄/岁 67.66±13.29 68.41±12.07 0.298 0.766 性别/例(%) 0.298 0.585 男 78(67.83) 22(62.86) 女 37(32.17) 13(37.14) 疾病类型/例(%) 1.920 0.589 脑外伤 30(26.09) 9(25.71) 脑卒中 8(6.96) 5(14.29) 感染性休克 39(33.91) 10(28.57) 重症肺炎 38(33.04) 11(31.43) APACHEⅡ评分/分 13.24±8.83 18.56±9.79 3.042 0.003 SOFA评分/分 7.62±2.97 9.14±3.35 2.572 0.011 ICU住院时间/d 9.41±2.37 10.74±3.35 2.622 0.010 SBT前血气分析指标 pH 7.35±0.14 7.41±0.16 2.146 0.034 PaCO2/mmHg 41.47±8.51 37.87±7.04 2.275 0.024 PaO2/mmHg 97.02±6.55 98.16±6.34 0.908 0.365 PaO2/FiO2 243.49±35.03 236.11±33.18 1.104 0.271 MV时间/d 7.54±2.18 8.67±3.85 2.202 0.029 SBT 30 min时测量指标 HR/(次/min) 87.03±12.14 91.22±14.98 1.689 0.093 RR/(次/min) 22.10±3.01 25.50±3.62 5.573 < 0.001 Vt/L 0.39±0.13 0.40±0.16 0.377 0.707 MAP/mmHg 91.33±9.31 92.26±9.64 0.513 0.609 RSBI/[次/(mL·min)] 56.67±10.82 63.75±17.69 2.881 0.005 膈肌超声指标 DE/mm 12.32±2.36 10.54±2.25 3.949 < 0.001 DTF/% 25.23±3.31 19.60±3.07 8.956 < 0.001 DE-RSBI/[次/(min·mm)] 1.93±0.67 2.64±0.79 5.259 < 0.001 DTF-RSBI/[次/(min·mm)] 66.20±7.33 105.64±9.61 25.821 < 0.001 表 2 各定量参数对撤机失败的预测价值
项目 AUC 截断值 95%CI P 灵敏度/% 特异度/% 约登指数 RSBI 0.715 67.02次/(mL·min) 0.681~0.855 < 0.001 75.33 72.08 0.474 DE 0.796 10.9 mm 0.729~0.860 < 0.001 82.95 80.16 0.631 DTF 0.721 30.11% 0.648~0.788 < 0.001 76.21 87.65 0.639 DE-RSBI 0.820 2.04次/(min·mm) 0.756~0.880 < 0.001 88.36 84.73 0.731 DTF-RSBI 0.872 73.15次/(min·mm) 0.823~0.920 < 0.001 96.42 93.28 0.897 -
[1] 李睿, 宋秋鸣. 慢性阻塞性肺疾病急性加重期患者有创机械通气拔管失败的风险预测[J]. 临床急诊杂志, 2021, 22(10): 673-677. doi: 10.13201/j.issn.1009-5918.2021.10.007
[2] Neumann B, Angstwurm K, Mergenthaler P, et al. Myasthenic crisis demanding mechanical ventilation: A multicenter analysis of 250 cases[J]. Neurology, 2020, 94(3): e299-e313. doi: 10.1212/WNL.0000000000008688
[3] Trivedi V, Chaudhuri D, Jinah R, et al. The Usefulness of the Rapid Shallow Breathing Index in Predicting Successful Extubation: A Systematic Review and Meta-analysis[J]. Chest, 2022, 161(1): 97-111. doi: 10.1016/j.chest.2021.06.030
[4] 刘荃乐, 黄满花, 奚小土, 等. 肺部超声在严重急性低氧性呼吸衰竭中的应用进展[J]. 临床急诊杂志, 2022, 23(2): 154-160. doi: 10.13201/j.issn.1009-5918.2022.02.016
[5] Towner JE, Rahmani R, Zammit CG, et al. Mechanical ventilation in aneurysmal subarachnoid hemorrhage: systematic review and recommendations[J]. Crit Care, 2020, 24(1): e575. doi: 10.1186/s13054-020-03269-8
[6] Dadam MM, Gonçalves ARR, Mortari GL, et al. The Effect of Reconnection to Mechanical Ventilation for 1 Hour After Spontaneous Breathing Trial on Reintubation Among Patients Ventilated for More Than 12 Hours: A Randomized Clinical Trial[J]. Chest, 2021, 160(1): 148-156. doi: 10.1016/j.chest.2021.02.064
[7] Subirà C, Hernández G, Vázquez A, et al. Effect of Pressure Support vs T-Piece Ventilation Strategies During Spontaneous Breathing Trials on Successful Extubation Among Patients Receiving Mechanical Ventilation: A Randomized Clinical Trial[J]. JAMA, 2019, 321(22): 2175-2182. doi: 10.1001/jama.2019.7234
[8] Ziaka M, Exadaktylos A. Brain-lung interactions and mechanical ventilation in patients with isolated brain injury[J]. Crit Care, 2021, 25(1): e358. doi: 10.1186/s13054-021-03778-0
[9] Schepens T, Dres M, Heunks L, et al. Diaphragm-protective mechanical ventilation[J]. Curr Opin Crit Care, 2019, 25(1): 77-85. doi: 10.1097/MCC.0000000000000578
[10] 梁子坤, 黄远生, 杨勇. 超声评估膈肌功能在指导重症慢阻肺机械通气患者撤机中的应用价值分析[J]. 影像研究与医学应用, 2022, 6(5): 35-37. https://www.cnki.com.cn/Article/CJFDTOTAL-YXYY202205012.htm
[11] 赵浩天, 龙玲, 任珊, 等. 膈肌超声联合呼吸力学指标对ICU老年患者撤机预后评价功能[J]. 中国老年学杂志, 2021, 41(10): 2065-2069. doi: 10.3969/j.issn.1005-9202.2021.10.016
[12] Munshi FA, Bukhari ZM, Alshaikh H, et al. Rapid Shallow Breathing Index as a Predictor of Extubation Outcomes in Pediatric Patients Underwent Cardiac Surgeries at King Faisal Cardiac Center[J]. Cureus, 2020, 12(6): e8754.
[13] Figueroa-Casas JB, Montoya R, Garcia-Blanco J, et al. Effect of Using the Rapid Shallow Breathing Index as Readiness Criterion for Spontaneous Breathing Trials in a Weaning Protocol[J]. Am J Med Sci, 2020, 359(2): 117-122. doi: 10.1016/j.amjms.2019.11.002
[14] Fiatt M, Bosio AC, Neves D, et al. Accuracy of a spontaneous breathing trial for extubation of neonates[J]. J Neonatal Perinatal Med, 2021, 14(3): 375-382. doi: 10.3233/NPM-200573
[15] Sandoval Moreno LM, Casas Quiroga IC, Wilches Luna EC, et al. Efficacy of respiratory muscle training in weaning of mechanical ventilation in patients with mechanical ventilation for 48 hours or more: A Randomized Controlled Clinical Trial[J]. Med Intensiva(Engl Ed), 2019, 43(2): 79-89. doi: 10.1016/j.medin.2017.11.010
[16] Alam MJ, Roy S, Iktidar MA, et al. Diaphragm ultrasound as a better predictor of successful extubation from mechanical ventilation than rapid shallow breathing index[J]. Acute Crit Care, 2022, 37(1): 94-100. doi: 10.4266/acc.2021.01354
[17] Grassi A, Ferlicca D, Lupieri E, et al. Assisted mechanical ventilation promotes recovery of diaphragmatic thickness in critically ill patients: a prospective observational study[J]. Crit Care, 2020, 24(1): e85. doi: 10.1186/s13054-020-2761-6
[18] Cammarota G, Rossi E, Vitali L, et al. Effect of awake prone position on diaphragmatic thickening fraction in patients assisted by noninvasive ventilation for hypoxemic acute respiratory failure related to novel coronavirus disease[J]. Crit Care, 2021, 25(1): e305. doi: 10.1186/s13054-021-03735-x
[19] Acar H, Yamanoglu A. Rapid Shallow Breathing Index as a Predictor for Intubation and Mortality in Acute Respiratory Failure[J]. Respir Care, 2022, 67(5): 562-571. doi: 10.4187/respcare.09525
[20] Dong YM, Sun J, Li YX, et al. Development and Validation of a Nomogram for Assessing Survival in Patients With COVID-19 Pneumonia[J]. Clin Infect Dis, 2021, 72(4): 652-660. doi: 10.1093/cid/ciaa963
[21] Rello J, Ramírez-Estrada S, Romero A, et al. Factors associated with ventilator-associated events: an international multicenter prospective cohort study[J]. Eur J Clin Microbiol Infect Dis, 2019, 38(9): 1693-1699. doi: 10.1007/s10096-019-03596-x
-




 下载:
下载: