-
摘要: 目的 收集气性坏疽病例的临床资料,总结临床特点及治疗经验,为临床诊治提供数据参考。方法 回顾2013年1月—2023年1月北京积水潭医院重症医学科收治的诊断为气性坏疽的患者,将患者分为感染性休克组及非感染性休克组,记录基本信息、入院实验室数据、病原学数据、临床预后和预测评分(LRINEC评分、SIARI评分和NAS评分)。结果 共纳入14例患者,死亡的3例(21.4%)患者早期均出现感染性休克。患者全部为男性;基础疾病包括高血压(3例)、糖尿病(2例)、冠心病(1例)、肾功能不全(1例)等;感染部位包括下肢8例(57.1%),会阴区及肛周2例(14.3%),手部1例(7.1%),骨盆区及骶尾部1例(7.1%),泌尿系1例(7.1%),腹部1例(7.1%)。12例(85.7%)患者粗大杆菌涂片阳性;4例(28.6%)患者的伤口分泌物培养出产气荚膜梭菌。感染性休克组早期APTT、PT、INR明显高于非感染性休克组(P < 0.05)。ICU住院时间(P=0.176)和总住院天数(P=0.257)在2组间差异无统计学意义。感染性休克组的住院费用为(16.0±10.0)万元,显著高于无感染性休克组的(7.2±3.9)万元(P=0.048)。结论 气性坏疽早期诊断十分重要,LRINEC评分和粗大杆菌涂片是较为敏感的筛查手段,气性坏疽一旦进展为感染性休克,病死率及住院费用将明显增加。感染性休克组患者早期的凝血指标也明显较差。
-
关键词:
- 气性坏疽 /
- 产气荚膜梭菌 /
- 坏死性筋膜炎实验室风险指标评分 /
- 坏死性筋膜炎 /
- 外毒素
Abstract: Objective Collect clinical data of gas gangrene cases and summarize clinical characteristics and treatment experience to provide data reference for clinical diagnosis and treatment.Methods The patients diagnosed as gas gangrene in the Department of Intensive Care Unit of Beijing Jishuitan Hospital from January 2013 to January 2023 were divided into septic shock group and non-septic shock group. The basic information, admission laboratory data, pathogenic data, clinical prognosis, and prediction score(LRINEC score, SIARI score, NAS score) were recorded.Results A total of 14 patients were included. Three patients(21.4%) died of septic shock at the early stage. All patients were male. Basic diseases include hypertension(3 cases), diabetes(2 cases), coronary heart disease(1 case), renal insufficiency(1 case), etc. The infection sites included 8 cases(57.1%) of lower limbs, 2 cases(14.3%) of perineal region and perianal region, 1 case(7.1%) of hand, 1 case(7.1%) of pelvic region and sacrococcygeal region, 1 case(7.1%) of urinary system, and 1 case(7.1%) of abdomen. The early wound secretion smears from the 12(85.7%) patients with gas gangrene infection in the present study showed large gram-positive rods. Clostridium perfringens was cultured in the wound secretion of 4 patients(28.6%). The early APTT, PT and INR in septic shock group were significantly higher than those in non-septic shock group(P < 0.05). There was no significant difference between the two groups in the length of stay in ICU(P=0.176) and the total length of stay in hospital(P=0.257). The hospitalization cost of the septic shock group was(160 000±100 000) Yuan, significantly higher than(72 000±39 000) Yuan in the non-septic shock group(P=0.048).Conclusion The early diagnosis of gas gangrene is very important. LRINEC score and the early wound secretion smears are relatively sensitive screening methods. Once gas gangrene develops into septic shock, the mortality and hospitalization costs will increase significantly and the early coagulation indexes of patients with septic shock will be significantly worse. -

-
表 1 基本资料及临床预后
例序 性别 年龄/岁 主要创伤诊断 合并症 伤口粗大杆菌涂片a) 培养结果(初始创面/血) 初始抗生素 预后 1 男 53 小腿开放性损伤,胫腓骨骨折 无 + 创面(产气荚膜梭菌) 哌拉西林他唑巴坦 治愈 2 男 27 小腿开放性损伤伴骨折,膝关节脱位 无 + 创面(大肠埃希菌) 哌拉西林他唑巴坦 治愈 3 男 17 小腿挤压伤,胫骨远端骨折,小腿开放性损伤 无 + 创面(产气荚膜梭菌+屎肠球菌) 头孢哌酮钠舒巴坦钠+甲硝唑 治愈 4 男 51 手开放性外伤累及肌腱,掌骨骨折 无 + 无 头孢哌酮钠舒巴坦钠 治愈 5 男 9 小腿开放性损伤伴骨折,胫骨远端骨折伴腓骨骨折 无 + 创面(大肠埃希菌+嗜水气单胞菌) 头孢哌酮钠舒巴坦钠+甲硝唑 治愈 6 男 19 左下肢截肢清创术后 无 - 创面(鲍曼不动杆菌,屎肠球菌),血培养(鲍曼不动杆菌) 头孢哌酮钠舒巴坦钠+万古霉素 治愈 7 男 76 肢体闭塞性动脉硬化症,右股腘动脉人工血管血栓形成 糖尿病,高血压,冠心病 + 创面(产气荚膜梭菌+溶血性葡萄球菌) 亚胺培南西司他丁钠 治愈 8 男 49 腘动脉损伤(双侧),骨盆骨折(开放性),皮肤剥脱伤(右股、骨盆区、骶尾部),热压伤(右股) 无 + 创面(大肠埃希菌、奇异变形菌),血培养(大肠埃希菌、奇异变形菌) 亚胺培南西司他丁钠+甲硝唑 治愈 9 男 12 小腿车祸伤,小腿多发血管、神经、肌腱损伤 无 + 创面(拜氏梭菌,摩氏摩根菌,大肠埃希菌) 哌拉西林他唑巴坦+甲硝唑 治愈 10 男 11 左股及臀部皮肤缺损,左下肢、臀部撕脱伤 无 + 创面(产气荚膜梭菌+粪肠球菌+阴沟肠杆菌) 美罗培南 治愈 11 男 62 肛周感染;盆间隙及后腹膜间隙感染 高血压、糖尿病、肾功能不全 + 创面(肺炎克雷伯菌),血培养(肺炎克雷伯菌) 亚胺培南西司他丁钠+甲硝唑 死亡 12 男 22 肌肉挫伤伴肌坏死(腹部,左下肢,左髋部);大面积皮肤及软组织剥脱 无 - 创面(粪肠球菌) 哌拉西林他唑巴坦+万古霉素 死亡 13 男 28 会阴部撕裂伤,会阴部伤口感染,骨盆髋臼骨折,股骨干骨折 无 + 创面(大肠埃希菌,粪肠球菌),血培养(大肠埃希菌) 头孢哌酮钠舒巴坦钠 死亡 14 男 35 尿道异物,泌尿系感染 高血压 + 创面(牛链球菌Ⅱ型),血培养(牛链球菌Ⅱ型) 左氧氟沙星+奥硝唑 治愈 注:例1~例7为无感染性休克组,例8~例14为感染性休克组;a)粗大杆菌涂片为入院初始取样结果。 表 2 感染性休克组及非感染性休克组实验室检查结果比较
X±S,M(Q1,Q3) 实验室指标 非感染性休克组(n=7) 感染性休克组(n=7) 总体(n=14) P Z/t 白细胞/(×109/L) 16.6(13.7,17.9) 21.4(16.6,23.4) 16.9(14.6,21.0) 0.110 2.551 血红蛋白/(g/L) 73.7±21.2 86.3±21.6 80.0±21.6 0.294 1.207 血钠/(mmol/L) 134.7±5.5 138.4±7.0 136.4±6.2 0.306 1.150 APTT/s 30.4±3.4 41.1±9.7 35.8±8.9 0.018 7.541 PT/s 12.8±1.3 16.0±3.6 14.4±3.1 0.044 5.069 INR 1.0±0.0 1.3±0.3 1.2±0.3 0.018 7.453 血糖/(mmol/L) 5.8(5.7,6.8) 6.9(6.5,7.8) 6.5(5.7,7.2) 0.201 1.636 尿素氮/(mmol/L) 5.0(3.4,9.2) 9.9(6.3,12.8) 7.8(4.0,10.9) 0.225 1.473 血肌酐/(μmol/L) 62.0(48.0,73.0) 101.0(74.5,130.5) 73.0(49.8,101.8) 0.141 2.164 表 3 LRINEC评分
变量(单位) 分值 C反应蛋白/(mg/L) < 150 0 ≥150 4 白细胞/(×109/L) < 15 0 15~25 1 >25 2 血红蛋白/(g/L) >13.5 0 11~13.5 1 < 11 2 血钠/(mmol/L) ≥135 0 < 135 2 血肌酐/(μmol/L) ≤141 0 >141 2 血糖/(mmol/L) ≤10 0 >10 1 表 4 感染性休克组和非感染性休克组预测评分及预后比较
X±S 评分及预后 非感染性休克组 感染性休克组 t P LRINEC评分/分 7.0±2.1 7.3±2.3 0.060 0.811 SIARI评分/分 3.9±2.1 5.9±0.7 5.654 0.035 NAS评分/分 4.7±3.4 5.4±2.9 0.183 0.676 ICU住院天数/d 4.9±2.2 9.0±7.3 2.066 0.176 总住院天数/d 33.7±21.3 23.3±9.1 1.419 0.257 住院费用/万元 7.2±3.9 16.0±10.0 4.727 0.048 -
[1] Leiblein M, Wagner N, Adam EH, et al. Clostridial gas gangrene-A rare but deadly infection: case series and comparison to other necrotizing soft tissue infections[J]. Orthop Surg, 2020, 12(6): 1733-1747. doi: 10.1111/os.12804
[2] Sárvári KP, Schoblocher D. The antibiotic susceptibility pattern of gas gangrene-forming Clostridium spp. clinical isolates from South-Eastern Hungary[J]. Infect Dis, 2020, 52(3): 196-201. doi: 10.1080/23744235.2019.1696472
[3] Stevens DL, Bryant AE. Necrotizing soft-tissue infections[J]. N Engl J Med, 2018, 378(10): 971. doi: 10.1056/NEJMc1800044
[4] Sison-Martinez J, Cooper JS. Hyperbaric treatment of clostridial myositis and myonecrosis[M]. Treasure Island: StatPearls Publishing, 2023.
[5] Buboltz JB, Murphy-Lavoie HM. Gas gangrene[M]. Treasure Island: StatPearls Publishing, 2023.
[6] Madsen MB, Skrede S, Perner A, et al. Patient's characteristics and outcomes in necrotising soft-tissue infections: results from a Scandinavian, multicentre, prospective cohort study[J]. Intensive Care Med, 2019, 45(9): 1241-1251. doi: 10.1007/s00134-019-05730-x
[7] Breidung D, Malsagova AT, Barth AA, et al. Diagnostic and prognostic value of the Laboratory Risk Indicator for Necrotising Fasciitis(LRINEC)based on an 18 years'experience[J]. J Plast Reconstr Aesthetic Surg, 2023, 77: 228-235. doi: 10.1016/j.bjps.2022.11.061
[8] R K, Tandup C, Reddy D, et al. Prospective validation and comparison of laboratory risk indicator for necrotizing fasciitis(LRINEC)and site other than lower limb, immunosuppression, age, renal impairment, and inflammatory markers(SIARI)scoring systems for necrotizing fasciitis[J]. J Surg Res, 2023, 283: 719-725. doi: 10.1016/j.jss.2022.11.001
[9] Harasawa T, Kawai-Kowase K, Tamura J, et al. Accurate and quick predictor of necrotizing soft tissue infection: usefulness of the LRINEC score and NSTI assessment score[J]. J Infect Chemother, 2020, 26(4): 331-334. doi: 10.1016/j.jiac.2019.10.007
[10] Preseau T, Deviendt J, Duttman R, et al. Clostridium perfringens in gas gangrene: still a smoked Gun![J]. J Transl Int Med, 2020, 8(1): 54-56. doi: 10.2478/jtim-2020-0009
[11] 孙旭, 米萌, 朱仕文, 等. 开放骨折并发气性坏疽的诊治[J]. 骨科临床与研究杂志, 2018, 3(4): 230-234. doi: 10.19548/j.2096-269x.2018.04.009
[12] Srivastava I, Aldape MJ, Bryant AE, et al. Spontaneous C. septicum gas gangrene: a literature review[J]. Anaerobe, 2017, 48: 165-171. doi: 10.1016/j.anaerobe.2017.07.008
[13] Abu El Hawa AA, Dekker PK, Mishu MD, et al. Early diagnosis and surgical management of necrotizing fasciitis of the lower extremities: risk factors for mortality and amputation[J]. Adv Wound Care(New Rochelle), 2022, 11(5): 217-225. doi: 10.1089/wound.2021.0031
[14] 肖光夏. 气性坏疽[M]//吴在德, 吴肇汉. 外科学. 7版. 北京: 人民卫生出版社, 2008: 162-163.
[15] Cheung JK, Adams V, D'Souza D, et al. The EngCP endo α-N-acetylgalactosaminidase is a virulence factor involved in Clostridium perfringens gas gangrene infections[J]. Int J Med Microbiol, 2020, 310(2): 151398. doi: 10.1016/j.ijmm.2020.151398
[16] Liu S, Yang XF, Zhang H, et al. Amentoflavone attenuates Clostridium perfringens gas gangrene by targeting alpha-toxin and perfringolysin O[J]. Front Pharmacol, 2020, 11: 179. doi: 10.3389/fphar.2020.00179
[17] Kanaujia R, Dahiya D, Banda AR, et al. Non-traumatic gas gangrene due to Clostridium sporogenes[J]. Lancet Infect Dis, 2020, 20(6): 754. doi: 10.1016/S1473-3099(20)30024-4
[18] Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America[J]. Clin Infect Dis, 2014, 59(2): e10-e52. doi: 10.1093/cid/ciu296
-

| 引用本文: | 白颖, 孙旭, 刘颖, 等. 重症气性坏疽患者的临床特点分析[J]. 临床急诊杂志, 2023, 24(6): 281-286. doi: 10.13201/j.issn.1009-5918.2023.06.002 |
| Citation: | BAI Ying, SUN Xu, LIU Ying, et al. Analysis of the clinical characteristics of patients with severe gas gangrene[J]. J Clin Emerg, 2023, 24(6): 281-286. doi: 10.13201/j.issn.1009-5918.2023.06.002 |
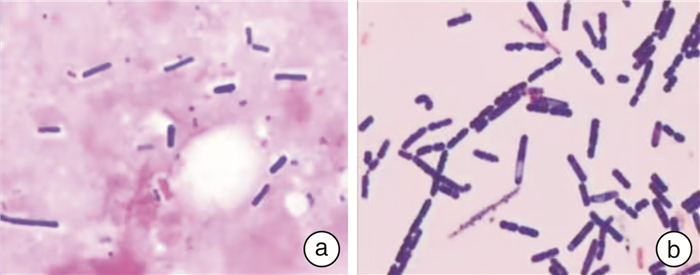
- Figure 1.
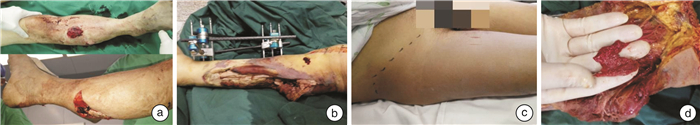
- Figure 2.



 下载:
下载: