Prognostic value of early glycemic lability index in patients with out-of-hospital cardiac arrest
-
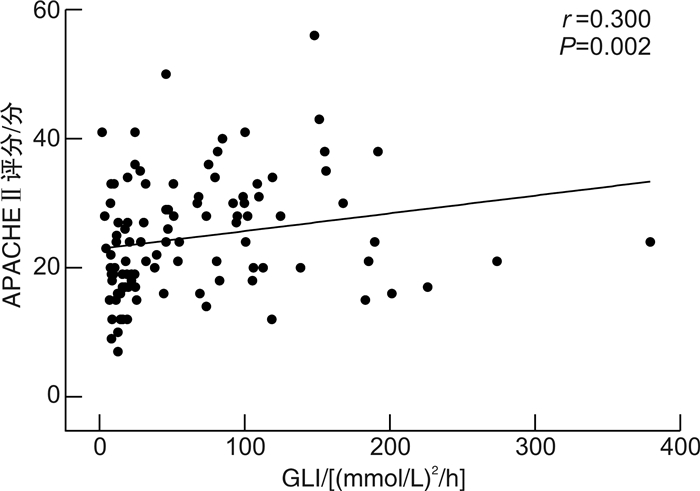
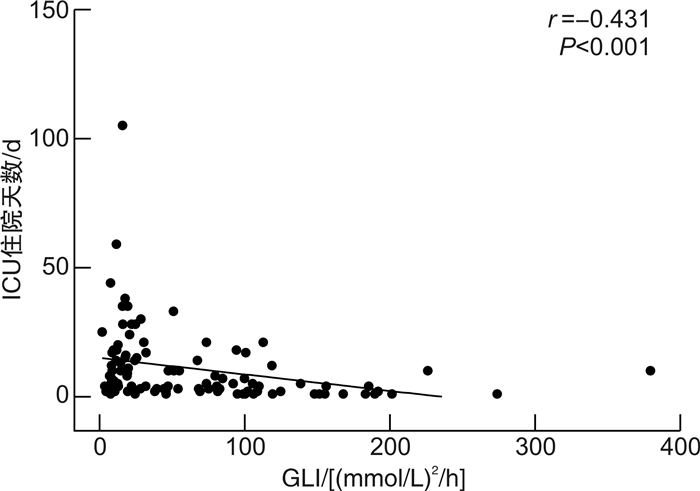
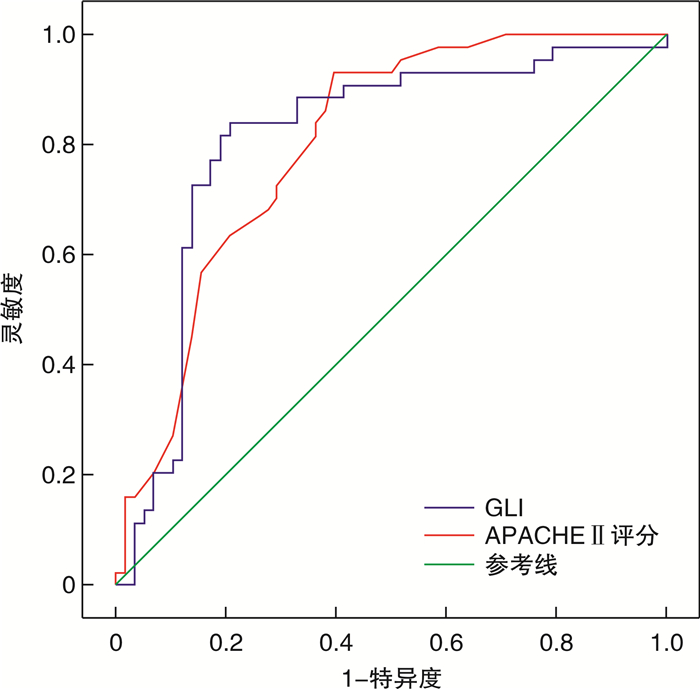
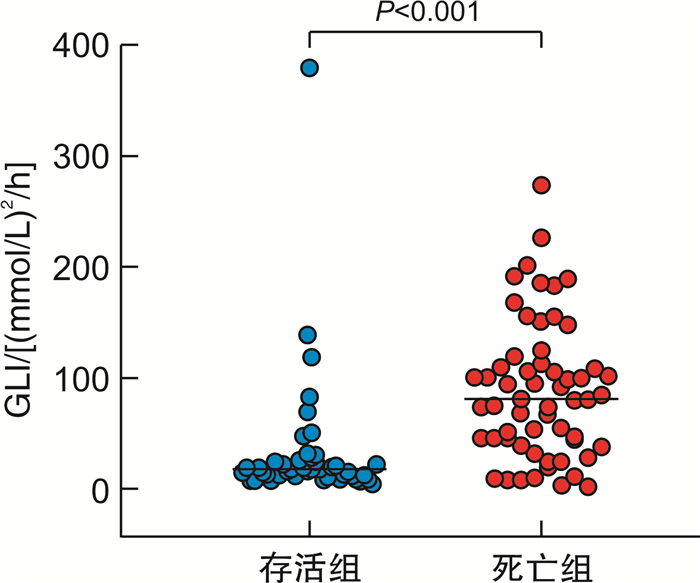
摘要: 目的 分析院外心脏骤停(out-of-hospital cardiac arrest,OHCA)患者早期血糖波动对预后的评估价值。方法 选取进入徐州医科大学附属医院符合标准的OHCA患者102例,每隔2 h一次,监测自主循环恢复(return of spontaneous circulation,ROSC)后入住ICU 24 h内的血糖值,根据公式得出血糖不稳定指数(glucose lability index,GLI)。根据患者28 d预后将其分为存活组和死亡组,比较2组患者一般资料及GLI的差异;根据GLI水平按照三分位数将患者分为3组(GLI 1组,GLI 2组,GLI 3组),比较各组患者28 d预后的差异;分析GLI和APACHE Ⅱ评分的相关性;绘制受试者工作特征(receiver operating characteristic,ROC)曲线评估GLI和APACHE Ⅱ评分对患者28 d预后的预测价值。结果 死亡组早期GLI、APACHE Ⅱ评分均大于存活组(P < 0.001);与GLI 1组相比,GLI 2组和GLI 3组28 d预后更差,APACHE Ⅱ评分更高(均P < 0.05);Spearman相关性分析显示GLI与APACHE Ⅱ呈正相关(r=0.300,P=0.002);二元logistic回归分析显示,较高的GLI(P=0.001)和较高的APACHE Ⅱ评分(P < 0.001)是OHCA患者预后差的独立危险因素。ROC曲线显示GLI和APACHE Ⅱ评分预测OHCA患者预后的曲线下面积(area under the curve,AUC)分别为0.810和0.802(P < 0.001)。结论 早期GLI可用于OHCA患者的28 d预后评估,早期积极控制血糖波动可能有利于改善患者的预后。Abstract: Objective To analyze the prognostic value of early blood glucose fluctuation in patients with out of hospital cardiac arrest(OHCA).Methods A total of 102 out-of-hospital cardiac arrest patients who entered Affiliated Hospital of Xuzhou Medical University and met the standards were selected, and the blood glucose values within 24 hours after admission to ICU after the return of spontaneous circulation(ROSC) were monitored every 2 hours. The blood glucose instability index(GLI) was obtained according to the formula. Patients were divided into survival group and death group according to their 28-day prognosis, compare the difference of general information and GLI between the two groups; Patients were divided into three groups(GLI 1, GLI 2, GLI 3) based on the GLI level according to the three quantiles, to compare the difference of 28-day prognosis in each group; Analyze the correlation between GLI and acute physiology and chronic health assessment(APACHE Ⅱ) scores; ROC curve was drawn to evaluate the predictive value of GLI and APACHE Ⅱ scores on the 28-day prognosis of patients.Results The scores of early GLI and APACHE Ⅱ in death group were higher than those in survival group(P < 0.001); Compared with GLI 1 group, GLI 2 group(P < 0.05) and GLI 3 group(P < 0.01) had worse 28-day prognosis and higher APACHE Ⅱ score; Spearman correlation analysis showed that GLI was positively correlated with APACHE Ⅱ(r=0.300, P=0.002); Binary logistic regression analysis showed that higher GLI(P=0.001) and higher APACHE Ⅱ score(P < 0.001) were independent risk factors for poor prognosis of OHCA patients. ROC curve showed that the area under the curve(AUC) predicted by GLI and APACHE Ⅱ scores for the prognosis of OHCA patients were 0.810 and 0.802, respectively(P < 0.001).Conclusion Early GLI can be used to evaluate the 28-day prognosis of OHCA patients, and early active control of blood glucose fluctuations may be helpful to improve the prognosis of patients.
-
Key words:
- out-of-hospital cardiac arrest /
- glucose variability /
- glucose lability index /
- prognosis
-

-
表 1 存活组和死亡组一般临床基线资料比较
例(%) 基线资料 存活组(n=44) 死亡组(n=58) P 年龄/岁 56(40,71) 63(49,68) 0.378 性别 0.244 男 23 37 女 21 21 高血压 23(52.27) 24(41.38) 0.277 糖尿病 13(29.55) 14(24.14) 0.542 吸烟 12(27.27) 19(32.76) 0.553 饮酒 13(29.55) 14(24.14) 0.557 CA病因 心血管系统 21(47.73) 16(27.59) 0.036 呼吸系统 3(6.82) 13(22.41) 0.061 神经系统 7(15.91) 18(31.03) 0.079 代谢 5(11.36) 1(1.72) 0.104 其他 8(18.18) 10(17.24) 0.902 CPR持续时间/min 10(8.5,11.5) 10(5,15) 0.445 机械通气时间/d 4.5(1.0,10.5) 3(2,7) 0.394 APACHE Ⅱ评分/分 19(15,24) 28(21,34) < 0.001 GLI/[(mmol/L)2/h] 17.76(12.88,24.72) 77.46(39.41,109.97) < 0.001 住院天数/d 20(10,33) 3(2,6) < 0.001 表 2 不同GLI组的组间资料比较
M(P25,P75) 组间资料 GLI 1组 GLI 2组 GLI 3组 P 28 d病死率/% 20.59 61.761) 88.241) < 0.001 入住ICU时间/d 11(5,20) 5(3,15) 2(1,5)1)2) 0.001 机械通气时间/d 4(1,10) 5(3,11) 2(1,5) 0.088 APACHE Ⅱ评分/分 19(15,25) 25(19,33)1) 28(20,34)1) < 0.001 与GLI 1组比较,1) P < 0.05;与GLI 2组比较,2) P < 0.05。 表 3 不同GLI组有无糖尿病患者之间28 d病死率的比较
组别 例数 28 d病死率/% GLI 1组 34 有糖尿病 8 37.50 无糖尿病 26 15.38 GLI 2组 34 有糖尿病 5 80.00 无糖尿病 29 58.62 GLI 3组 34 有糖尿病 14 92.86 无糖尿病 20 85.00 -
[1] Rea T, Kudenchuk PJ, Sayre MR, et al. Out of hospital cardiac arrest: past, present, and future[J]. Resuscitation, 2021, 165: 101-109. doi: 10.1016/j.resuscitation.2021.06.010
[2] 刘国祥, 朱长清, 王世伟, 等. 心脏骤停后综合征相关急性胃肠损伤的研究进展[J]. 临床急诊杂志, 2021, 22(9): 634-640. doi: 10.13201/j.issn.1009-5918.2021.09.014
[3] 中国研究型医院学会神经再生与修复专业委员会心脏重症脑保护学组, 中国研究型医院学会神经再生与修复专业委员会神经重症护理与康复学组. 亚低温脑保护中国专家共识[J]. 中华危重病急救医学, 2020, 32(4): 385-391. doi: 10.3760/cma.j.cn121430-20200117-00137
[4] 师维, 陆宗庆, 崔旋旋, 等. 2022年ERC-ESICM成人心脏骤停后温度控制临床实践指南解读[J]. 临床急诊杂志, 2022, 23(6): 371-377. doi: 10.13201/j.issn.1009-5918.2022.06.001
[5] Abramson TM, Bosson N, Whitfield D, et al. Elevated prehospital point-of-care glucose is associated with worse neurologic outcome after out-of-hospital cardiac arrest[J]. Resusc Plus, 2022, 9: 100204. doi: 10.1016/j.resplu.2022.100204
[6] Wang CH, Chang WT, Huang CH, et al. Associations between intra-arrest blood glucose level and outcomes of adult in-hospital cardiac arrest: a 10-year retrospective cohort study[J]. Resuscitation, 2020, 146: 103-110. doi: 10.1016/j.resuscitation.2019.11.012
[7] Oksanen T, Skrifvars MB, Varpula T, et al. Strict versus moderate glucose control after resuscitation from ventricular fibrillation[J]. Intensive Care Med, 2007, 33(12): 2093-2100. doi: 10.1007/s00134-007-0876-8
[8] Klonoff DC, Messler JC, Umpierrez GE, et al. Association between achieving inpatient glycemic control and clinical outcomes in hospitalized patients with COVID-19: a multicenter, retrospective hospital-based analysis[J]. Diabetes Care, 2021, 44(2): 578-585. doi: 10.2337/dc20-1857
[9] Freire Jorge P, Boer R, Posma RA, et al. Early lactate and glucose kinetics following return to spontaneous circulation after out-of-hospital cardiac arrest[J]. BMC Res Notes, 2021, 14(1): 183. doi: 10.1186/s13104-021-05604-w
[10] Duan Y, Li ZZ, Liu P, et al. The efficacy of intraoperatie continuous glucose monitoring in patients undergoing liver transplantation: a study protocol for a prospective randomized controlled superiority trial[J]. Trials, 2023, 24(1): 72. doi: 10.1186/s13063-023-07073-x
[11] 胡森安, 谭俊锋, 彭昌, 等. 血糖变异性参数在重症新型冠状病毒肺炎患者预后判断中的价值[J]. 检验医学, 2021, 36(4): 400-403. doi: 10.3969/j.issn.1673-8640.2021.04.011
[12] Lu ZQ, Tao G, Sun XY, et al. Association of blood glucose level and glycemic variability with mortality in sepsis patients during ICU hospitalization[J]. Front Public Health, 2022, 10: 857368. doi: 10.3389/fpubh.2022.857368
[13] 李佳媚, 高雅, 张静静, 等. 血糖水平及血糖变异度对ICU成年急性呼吸衰竭患者预后的影响[J]. 中国急救医学, 2021, 41(3): 196-200. doi: 10.3969/j.issn.1002-1949.2021.03.003
[14] Feng XF, Hai JJ, Ma Y, et al. Sudden cardiac death in mainland China: a systematic analysis[J]. Circ Arrhythm Electrophysiol, 2018, 11(11): e006684. doi: 10.1161/CIRCEP.118.006684
[15] 中华医学会急诊医学分会复苏学组, 中国医药教育协会急诊专业委员会, 成人心脏骤停后综合征诊断和治疗中国急诊专家共识组, 等. 成人心脏骤停后综合征诊断和治疗中国急诊专家共识[J]. 中华急诊医学杂志, 2021, 30(7): 799-808. doi: 10.3760/cma.j.issn.1671-0282.2021.07.002
[16] Cueni-Villoz N, Devigili A, Delodder F, et al. Increased blood glucose variability during therapeutic hypothermia and outcome after cardiac arrest[J]. Crit Care Med, 2011, 39(10): 2225-2231. doi: 10.1097/CCM.0b013e31822572c9
[17] Zhou DW, Li ZM, Shi GZ, et al. Proportion of time spent in blood glucose range 70 to 140 mg/dL is associated with increased survival in patients admitted to ICU after cardiac arrest: a multicenter observational study[J]. Medicine(Baltimore), 2020, 99(33): e21728.
[18] Borgquist O, Wise MP, Nielsen N, et al. Dysglycemia, glycemic variability, and outcome after cardiac arrest and temperature management at 33℃ and 36℃[J]. Crit Care Med, 2017, 45(8): 1337-1343. doi: 10.1097/CCM.0000000000002367
[19] Lee BK, Lee HY, Jeung KW, et al. Association of blood glucose variability with outcomes in comatose cardiac arrest survivors treated with therapeutic hypothermia[J]. Am J Emerg Med, 2013, 31(3): 566-572. doi: 10.1016/j.ajem.2012.11.002
[20] Watt C, Sanchez-Rangel E, Hwang JJ. Glycemic variability and CNS inflammation: reviewing the connection[J]. Nutrients, 2020, 12(12): 3906. doi: 10.3390/nu12123906
[21] Quagliaro L, Piconi L, Assaloni R, et al. Intermittent high glucose enhances apoptosis related to oxidative stress in human umbilical vein endothelial cells: the role of protein kinase C and NAD(P)H-oxidase activation[J]. Diabetes, 2003, 52(11): 2795-2804. doi: 10.2337/diabetes.52.11.2795
[22] Piconi L, Quagliaro L, Da Ros R, et al. Intermittent high glucose enhances ICAM-1, VCAM-1, E-selectin and interleukin-6 expression in human umbilical endothelial cells in culture: the role of poly(ADP-ribose)polymerase[J]. J Thromb Haemost, 2004, 2(8): 1453-1459. doi: 10.1111/j.1538-7836.2004.00835.x
[23] Chung HS, Hwang SY, Kim JA, et al. Implications of fasting plasma glucose variability on the risk of incident peripheral artery disease in a population without diabetes: a nationwide population-based cohort study[J]. Cardiovasc Diabetol, 2022, 21(1): 15. doi: 10.1186/s12933-022-01448-1
[24] Agarwal S, Mathew J, Davis GM, et al. Continuous glucose monitoring in the intensive care unit during the COVID-19 pandemic[J]. Diabetes Care, 2021, 44(3): 847-849. doi: 10.2337/dc20-2219
[25] 夏云松, 刘旭, 毕红英, 等. 血糖相关指标与重症患者预后的相关性[J]. 贵州医科大学学报, 2021, 46(11): 1316-1320, 1332. https://www.cnki.com.cn/Article/CJFDTOTAL-GYYB202111012.htm
[26] Hanna M, Balintescu A, Glassford N, et al. Glycemic lability index and mortality in critically ill patients-a multicenter cohort study[J]. Acta Anaesthesiol Scand, 2021, 65(9): 1267-1275. doi: 10.1111/aas.13843
[27] Santana D, Mosteiro A, Pedrosa L, et al. Clinical relevance of glucose metrics during the early brain injury period after aneurysmal subarachnoid hemorrhage: an opportunity for continuous glucose monitoring[J]. Front Neurol, 2022, 13: 977307. doi: 10.3389/fneur.2022.977307
[28] Weinel LM, Summers MJ, Finnis ME, et al. Are point-of-care measurements of glycated haemoglobin accurate in the critically ill?[J]. Aust Crit Care, 2019, 32(6): 465-470.
-




 下载:
下载: