Effect of different protein in early stage supplementation on prognosis of patients with severe pneumonia
-
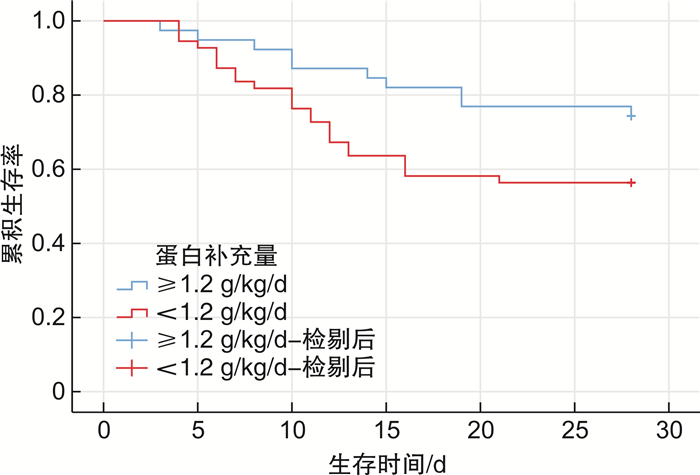
摘要: 目的 探讨早期不同蛋白摄入量对重症肺炎患者预后的影响。方法 回顾性分析诊断为重症肺炎的患者共94例,根据患者入ICU后28 d生存情况分为生存组和死亡组,收集统计2组患者的基线资料、实验室指标、临床资料等,并计算2组患者入院72 h内平均蛋白补充量,并根据蛋白补充量分为低蛋白组(< 1.2 g/kg/d)和高蛋白组(≥1.2 g/kg/d)。比较不同蛋白组患者的并发症发生率及预后情况。统计采用Cox回归分析以及Kaplane-Meier生存曲线分析。结果 死亡组患者蛋白补充≥1.2 g/kg/d的患者例数明显少于生存组(χ2=2.667,P=0.008);Cox回归分析显示蛋白补充量(≥1.2 g/kg/d)与显著降低病死率相关(HR=0.342,P=0.022);通过生存曲线分析显示≥1.2 g/kg/d的高蛋白组生存时间明显长于低蛋白组(χ2=4.805,P=0.028);高蛋白组并发ARDS和脓毒性休克的发生率低于低蛋白组(P < 0.05);另外与低蛋白组比较,高蛋白组可以缩短ICU住院时间(t=3.189,P=0.002),并降低28 d内病死率(χ2=6.665,P=0.010)。结论 对于重症肺炎患者早期蛋白补充≥1.2 g/kg/d有利于改善患者病情并降低病死率。Abstract: Objective To investigate the effects of different protein intake in early stage on the prognosis of patients with severe pneumonia.Methods A total of 94 patients diagnosed with severe pneumonia were retrospectively analyzed and divided into survival group and death group according to their 28-day survival. Baseline data, laboratory indicators and clinical information of the two groups of patients were collected and statistically analyzed, and the average protein supplementation of the two groups within 72 h after admission was calculated. They were divided into low protein group(< 1.2 g/kg/d) and high protein group(≥1.2 g/kg/d). Complications and prognosis of patients with different protein groups were compared. Cox regression analysis and Kaplane-Meier survival curve analysis were used.Results The number of patients with protein supplement ≥1.2 g/kg/d in the death group was significantly lower than that in the survival group(χ2=2.667, P=0.008). Cox regression analysis showed that protein supplementation(≥1.2 g/kg/d) was associated with significantly lower mortality(HR=0.342, P=0.022). Survival curve analysis showed that the survival time of high protein group ≥1.2 g/kg/d was significantly longer than that of control group(χ2=4.805, P=0.028). The incidences of ARDS and septic shock in high protein group were lower than those in low protein group(P < 0.05). The high protein group had shorter length of ICU stay(t=3.189, P=0.002) and lower mortality within 28 days(χ2=6.665, P=0.010) compared with the low protein group.Conclusion Early protein supplementation ≥1.2 g/kg/d is beneficial to reduce mortality and improve prognosis in patients with severe pneumonia.
-
Key words:
- protein supplement /
- severe pneumonia /
- prognosis
-

-
表 1 生存组和死亡组基线资料比较
X±S,例(%) 基线资料 生存组(n=60) 死亡组(n=34) t/χ2 P 年龄/岁 61.34±5.54 68.45±8.52 2.189 0.029 性别 1.870 0.174 男 37 18 女 23 16 BMI/(kg/m2) 23.16±4.72 21.43±3.95 1.423 0.156 APACHE Ⅱ评分/分 24.45±4.68 27.43±4.25 2.467 0.014 NRS2002评分/分 4.95±1.23 5.18±1.56 1.450 0.150 基础疾病 糖尿病 12(20) 7(20.59) 2.564 0.109 高血压 15(25) 9(26.47) 1.112 0.292 冠心病 8(13.33) 4(11.76) 3.024 0.082 慢性支气管炎 4(6.67) 2(5.88) 2.876 0.090 肺部感染病原体 细菌 43(71.67) 24(70.59) 2.456 0.117 病毒 5(8.33) 3(8.82) 1.768 0.184 真菌 3(5.00) 2(5.88) 3.123 0.077 非典型病原体 2(3.33) 1(2.94) 2.634 0.105 其他 7(11.67) 4(11.76) 2.520 0.112 总胆红素/(μmol/L) 14.54±4.65 12.76±3.43 1.453 0.147 ALT/(U/L) 49.87±13.39 54.67±14.48 1.897 0.059 AST/(U/L) 56.86±17.37 60.64±18.65 1.870 0.062 Cr/(μmol/L) 76.35±20.32 83.94±24.19 0.854 0.393 BUN/(mmol/L) 15.76±4.37 18.17±5.06 1.346 0.179 WBC/(×109/L) 12.35±7.98 13.56±8.17 1.65 0.100 血小板/(×109/L) 123.46±45.87 119.67±53.68 1.754 0.080 PCT/(μg/L) 12.41±6.38 16.26±7.36 2.328 0.021 CRP/(mg/L) 109.53±65.34 163.38±79.95 3.012 0.003 PaO2/FiO2 189.75±56.46 155.38±60.23 2.430 0.016 蛋白补充量≥1.2 g/kg/d 29(48.33) 10(29.41) 2.667 0.008 注:ALT,丙氨酸氨基转移酶;AST,门冬氨酸氨基转移酶;Cr,肌酐;BUN,尿素氮。 表 2 重症肺炎患者病死率的Cox回归分析
变量 单因素 多因素 HR(95%CI) P HR(95%CI) P 年龄 1.148(1.009~1.921) 0.012 1.072(0.624~1.459) 0.083 CRP 1.087(0.348~2.342) 0.078 APACHE Ⅱ评分 2.578(1.137~10.563) < 0.001 1.234(1.021~1.685) 0.006 氧合指数 1.126(1.108~3.236) 0.018 1.067(0.976~2.679) 0.164 蛋白补充量(≥1.2 g/kg/d) 0.265(0.124~0.876) 0.023 0.342(0.198~1.234) 0.022 表 3 低蛋白组和高蛋白组临床并发症和预后比较
X±S,例(%) 并发症和预后 低蛋白组(n=55) 高蛋白组(n=39) t/χ2 P 并发症 ARDS 18(32.73) 8(20.51) 5.124 0.024 脓毒性休克 8(14.55) 4(10.26) 4.567 0.033 急性肾损伤 7(12.73) 4(10.26) 2.650 0.104 机械通气时间/d 7.85±4.23 5.98±5.25 2.950 0.003 ICU住院时间/d 12.34±4.78 10.89±3.67 3.189 0.002 总住院时间/d 17.38±3.86 14.45±4.27 1.540 0.124 28 d内死亡 25(45.45) 9(23.08) 6.665 0.010 -
[1] Huang J, Guo JQ, Li HT, et al. Efficacy and safety of adjunctive corticosteroids therapy for patients with severe community-acquired pneumonia: a systematic review and meta-analysis[J]. Medicine(Baltimore), 2019, 98(13): e14636.
[2] Smith TJ, McClung JP. Nutrition, immune function, and infectious disease[J]. Med J(Ft Sam Houst Tex), 2021(PB 8-21-01/02/03): 133-136.
[3] Yanagita Y, Arizono S, Tawara Y, et al. The severity of nutrition and pneumonia predicts survival in patients with aspiration pneumonia: a retrospective observational study[J]. Clin Respir J, 2022, 16(7): 522-532. doi: 10.1111/crj.13521
[4] Huang SW, Lin HC, Chou YF, et al. The impact of higher protein intake in patients with prolonged mechanical ventilation[J]. Nutrients, 2022, 14(20): 4395. doi: 10.3390/nu14204395
[5] Balasubramanian S, Tran DH, Serra M, et al. Assessing calorie and protein recommendations for survivors of critical illness weaning from prolonged mechanical ventilation-can we find a proper balance?[J]. Clin Nutr ESPEN, 2021, 45: 449-453. doi: 10.1016/j.clnesp.2021.07.001
[6] 瞿介明, 施毅. 中国成人医院获得性肺炎与呼吸机相关性肺炎诊断和治疗指南(2018年版)的更新与解读[J]. 中华结核和呼吸杂志, 2018, 41(4): 244-246. doi: 10.3760/cma.j.issn.1001-0939.2018.04.002
[7] 侯佳彤, 吴筱箐, 梁杰佳, 等. 重症肺炎营养治疗进展[J]. 中国医师杂志, 2020, 22(7): 1118-1120, f3. doi: 10.3760/cma.j.cn431274-20200301-00217
[8] Sharma K, Mogensen KM, Robinson MK. Pathophysiology of critical illness and role of nutrition[J]. Nutr Clin Pract, 2019, 34(1): 12-22. doi: 10.1002/ncp.10232
[9] Stoppe C, Wendt S, Mehta NM, et al. Biomarkers in critical care nutrition[J]. Crit Care, 2020, 24(1): 499. doi: 10.1186/s13054-020-03208-7
[10] Bagheri A, Hashemi R, Soltani S, et al. The relationship between food-based pro-inflammatory diet and sarcopenia: findings from a cross-sectional study in Iranian elderly people[J]. Front Med(Lausanne), 2021, 8: 649907.
[11] Burns DP, Murphy KH, Lucking EF, et al. Inspiratory pressure-generating capacity is preserved during ventilatory and non-ventilatory behaviours in young dystrophic mdx mice despite profound diaphragm muscle weakness[J]. J Physiol, 2019, 597(3): 831-848. doi: 10.1113/JP277443
[12] Zhang Q, Zhou J, Zhu DM, et al. Evaluation of the effect of high protein supply on diaphragm atrophy in critically ill patients receiving prolonged mechanical ventilation[J]. Nutr Clin Pract, 2022, 37(2): 402-412. doi: 10.1002/ncp.10672
[13] Casaer MP, Mesotten D, Hermans G, et al. Early versus late parenteral nutrition in critically ill adults[J]. N Engl J Med, 2011, 365(6): 506-517. doi: 10.1056/NEJMoa1102662
[14] Fuentes Padilla P, Martínez G, Vernooij RW, et al. Early enteral nutrition(within 48 hours)versus delayed enteral nutrition(after 48 hours)with or without supplemental parenteral nutrition in critically ill adults[J]. Cochrane Database Syst Rev, 2019, 2019(10): CD012340.
[15] Li P, Zhong CY, Qiao SB, et al. Effect of supplemental parenteral nutrition on all-cause mortality in critically Ill adults: a meta-analysis and subgroup analysis[J]. Front Nutr, 2022, 9: 897846. doi: 10.3389/fnut.2022.897846
[16] 潘金萍, 刘菁, 都军, 等. 早期肠内营养联合补充性肠外营养在危重症患者中的应用研究[J]. 临床急诊杂志, 2022, 23(4): 231-236. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202204002.htm
[17] Meftahi GH, Jangravi Z, Sahraei H, et al. The possible pathophysiology mechanism of cytokine storm in elderly adults with COVID-19 infection: the contribution of inflame-aging[J]. Inflamm Res, 2020, 69(9): 825-839. doi: 10.1007/s00011-020-01372-8
[18] Whittle J, Molinger J, MacLeod D, et al. Persistent hypermetabolism and longitudinal energy expenditure in critically ill patients with COVID-19[J]. Crit Care, 2020, 24(1): 581. doi: 10.1186/s13054-020-03286-7
[19] Compher C, Bingham AL, McCall M, et al. Guidelines for the provision of nutrition support therapy in the adult critically ill patient: the American Society for Parenteral and Enteral Nutrition[J]. J Parenter Enter Nutr, 2022, 46(1): 12-41. doi: 10.1002/jpen.2267
[20] Singer P, Blaser AR, Berger MM, et al. ESPEN guideline on clinical nutrition in the intensive care unit[J]. Clin Nutr, 2019, 38(1): 48-79. doi: 10.1016/j.clnu.2018.08.037
[21] Silvah JH, de Lima CMM, Nicoletti CF, et al. Protein provision and lower mortality in critically ill patients with COVID-19[J]. Clin Nutr ESPEN, 2021, 45: 507-510. doi: 10.1016/j.clnesp.2021.07.005
-




 下载:
下载: