Correlation analysis of prognostic nutritional index and prognosis in patients with acute heart failure
-
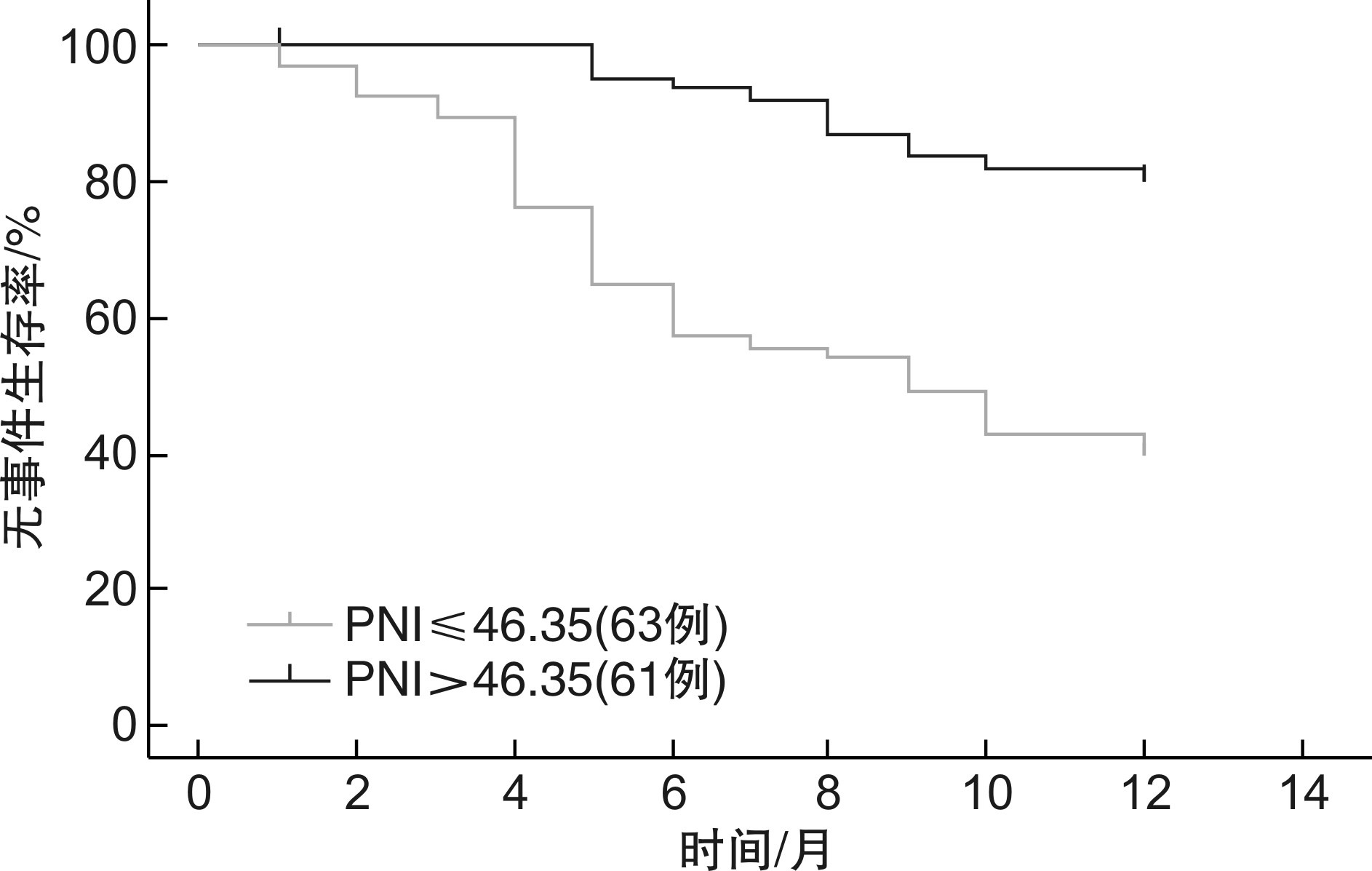
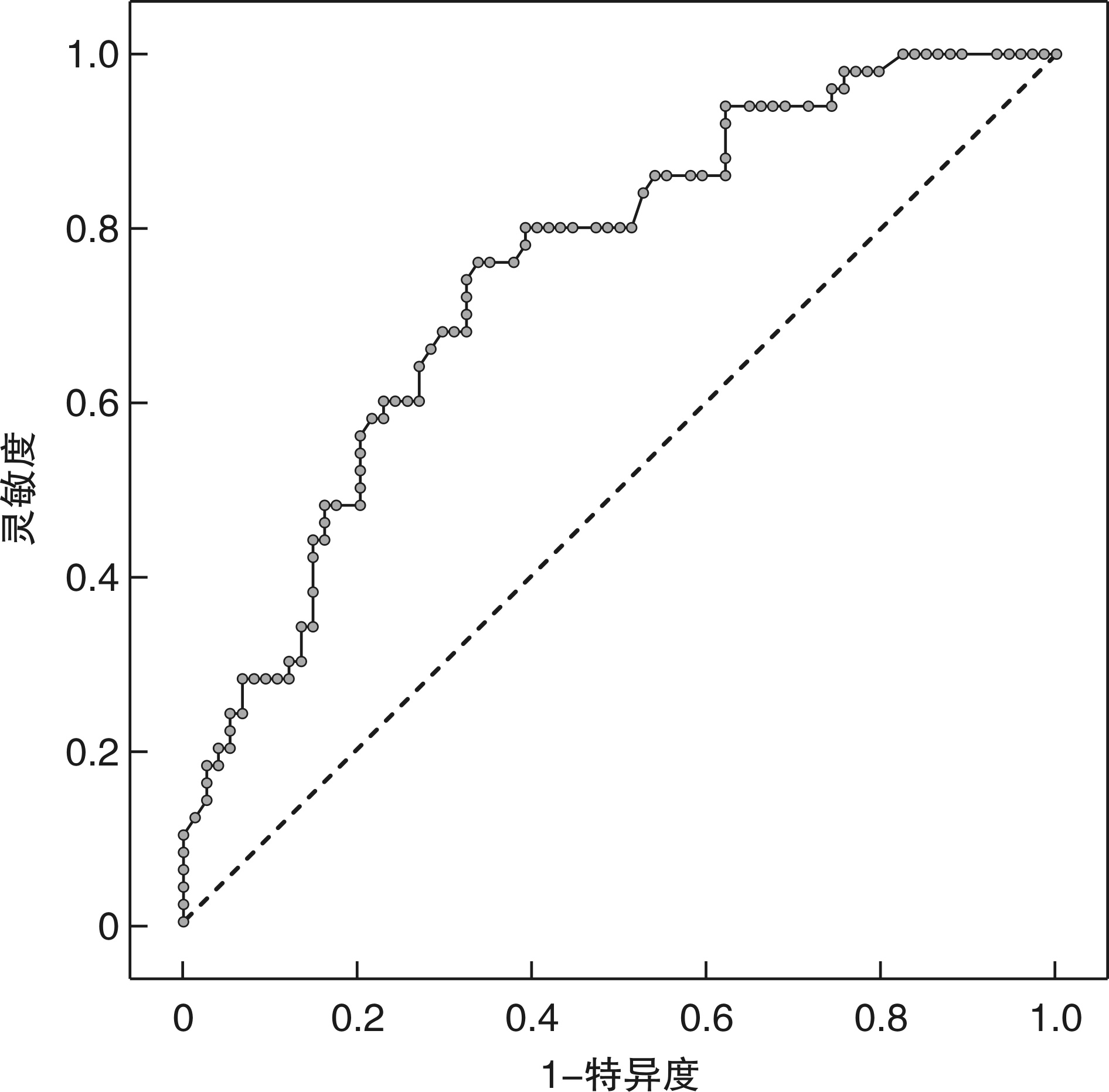
摘要: 目的 探讨预后营养指数(PNI)对急性心力衰竭(AHF)患者预后的影响。方法 回顾性分析124例因AHF入住我院的患者临床资料,进行为期1年的随访。定义终点事件为全因死亡或心衰再住院治疗,根据患者检验结果计算PNI,分析其对AHF患者预后的影响。结果 1年内预后良好组和预后不良组的PNI水平差异有统计学意义(P < 0.05)。ROC曲线显示:曲线下面积(AUC)为0.747,PNI最佳截断值为46.35(95%CI:0.661~0.833),灵敏度为76.0%,特异度为66.2%。PNI≤46.35的营养不良组患者出现预后不良的风险是营养良好患者的3.44倍(95%CI:1.276~9.273,P=0.015)。此外,N末端脑钠肽前体(NT-proBNP)、左心室射血分数(LVEF)均是影响AHF患者1年预后的独立危险因素(P < 0.05)。结论 入院时低PNI评分与AHF患者的不良预后相关,PNI用于评估AHF患者预后具有一定的临床价值。Abstract: Objective To investigate the effect of prognostic nutritional index (PNI) on prognosis of patients with acute heart failure (AHF).Methods The clinical data of 124 patients admitted to our hospital due to acute heart failure were retrospectively analyzed and followed up for 1 year. The endpoint event was defined as all-cause death or rehospitalization for heart failure, and PNI was calculated based on patient test results to analyze its effect on prognosis in patients with acute heart failure.Results There was significant difference in PNI levels between the good prognosis group and the poor prognosis group within 1 year (P < 0.05). The ROC curve showed that the area under the curve (AUC) was 0.747, the optimal cut-off value of PNI was 46.35 (95%CI: 0.661-0.833), the sensitivity was 76.0%, and the specificity was 66.2%. Patients in the malnourished group with PNI≤46.35 had a 3.44-fold higher risk of poor outcome than those in the well-nourished group (95%CI: 1.276-9.273 P=0.015). In addition, N-terminal brain natriuretic peptide precursor (NT-proBNP) and left ventricular ejection fraction (LVEF) were independent risk factors for 1-year prognosis in patients with acute heart failure (P < 0.05).Conclusion Low PNI score on admission is associated with poor prognosis in patients with acute heart failure, and PNI has certain clinical value in evaluating the prognosis of patients with acute heart failure.
-
Key words:
- acute heart failure /
- prognostic nutritional index /
- malnutrition /
- risk factors /
- prognosis /
- clinical value
-

-
表 1 不同预后及营养状态的AHF患者的基线临床特征
例(%),X±S,M(Q1,Q3) 变量 总体(n=124) 预后 营养状态 良好(n=74) 不良(n=50) t/χ2 P 高PNI (n=61) 低PNI (n=63) t/χ2 P 年龄/岁 71(64,79) 70(58,77) 78(67,83) 3.334 0.001 68(56,75) 77(68,82) 3.561 <0.001 女性 60(48.3) 35(47.3) 25(50.0) 0.087 0.768 26(42.6) 34(54) 1.600 0.206 住院时间/d 8.34±3.69 7.61±3.21 9.42±4.10 2.750 0.007 7.48±2.71 9.17±4.30 2.620 0.010 AHF类型 2.223 0.176 0.106 0.745 新发心衰 47(37.9) 32(43.2) 15(30.0) 24(39.3) 23(36.5) 心衰急性加重 77(62.1) 42(56.8) 35(70.0) 37(60.7) 40(63.5) 心衰合并症 高血压 75(60.5) 42(56.8) 33(66.0) 1.067 0.302 39(63.9) 36(57.1) 0.598 0.439 糖尿病 33(26.6) 19(25.7) 14(28.0) 0.083 0.774 24(39.3) 9(14.3) 9.964 0.002 缺血性心肌病 49(39.5) 24(32.4) 25(50.0) 3.853 0.050 20(32.8) 29(46) 2.275 0.131 NYHA分级 3.338 0.197 0.337 0.828 Ⅱ级 30(24.2) 20(27.0) 10(20.0) 16(26.2) 14(22.2) Ⅲ级 58(46.8) 37(50.0) 21(42.0) 27(44.3) 31(49.2) Ⅳ级 36(29.0) 17(23.0) 19(38.0) 18(29.5) 18(28.6) 实验室检查 Hb/(g·L-1) 129.0±22.1 135.0±20.4 120.0±21.7 3.930 0.001 135.1±21.5 122.9±21.2 3.169 0.002 淋巴细胞数/(×109·L-1) 1.40±0.53 1.54±0.49 1.19±0.52 3.730 0.001 1.70±0.48 1.11±0.39 7.553 < 0.001 白蛋白/(g·L-1) 39.1±4.5 40.6±4.2 37.0±4.2 4.150 0.001 42.4±2.8 35.8±3.3 11.890 < 0.001 胆固醇/(mmol·L-1) 3.91±1.01 3.95±0.96 3.84±1.08 0.639 0.524 3.90±1.0 3.91±1.01 0.083 0.934 AST/(U·L-1) 26.0 (18.0,41.8) 27.5 (19.0,45.8) 22.0 (14.0,33.0) 2.010 0.045 30 (19,34.5) 24 (15,33) 1.790 0.073 ALT/(U·L-1) 24.5 (19.0,34.0) 24.5 (19.0,36.3) 24.5 (17.0,21.0) 0.970 0.334 25 (19,34.5) 24 (19,33) 0.620 0.535 肌酐/(μmol·L-1) 76.0 (65.0,94.8) 73 (59.8,89.0) 105.0 (82.0,139.2) 2.091 0.036 75 (61,89) 79 (66,103) 1.400 0.162 尿素氮/(mmol·L-1) 6.8 (5.3,8.9) 8.1 (6.3,10.6) 7.3 (6.4,10.1) 2.832 0.050 6.7 (4.8,8.6) 6.8 (5.5,9.8) 0.977 0.328 NT-proBNP/(pg·mL-1) 4121 (1999,8116) 2751 (1618,6136) 7769 (3901,14 382) 5.140 < 0.001 3121 (1849,6255) 2912 (1849,9813) 3.054 0.002 LVEF/% 29.6±10.7 31.3±11.2 27.1±9.4 2.210 0.029 30.3±12.1 38.9±9.2 0.760 0.452 临床用药情况 利尿剂 116(93.5) 67(90.5) 49(98.0) 2.751 0.097 54(88.5) 62(98.4) 5.021 0.025 ACER/ARB 31(25.0) 20(27.0) 11(22.0) 0.402 0.526 17(27.9) 14(22.2) 0.527 0.468 β受体阻滞剂 92(74.2) 59(79.7) 33(66.0) 2.938 0.087 46(75.4) 46(73.0) 0.093 0.761 ARNI 88(71.0) 52(70.3) 11(22.0) 0.043 0.835 42(68.9) 46(73.0) 0.261 0.610 左西孟旦 20(16.1) 9(12.2) 33(66.0) 2.135 0.144 7(11.5) 13(20.6) 1.922 0.166 他汀药物 82(66.1) 49(66.2) 33(66.0) 0.001 0.980 39(63.9) 43(68.3) 0.258 0.611 阿司匹林 60(48.4) 37(50.0) 23(46.0) 0.191 0.662 31(50.8) 29(46) 0.284 0.594 PNI 46.3 (42.0,50.4) 48.1 (44.3,52.0) 43.5 (40.0,46.5) 4.503 < 0.001 高PNI 61(49.2) 49(66.2) 12(24.0) 21.280 < 0.001 低PNI 63(50.8) 25(33.8) 38(76.0) 预后不良 12(19.7) 38(60.3) 21.280 < 0.001 注:Hb,血红蛋白浓度;ALT,丙氨酸氨基转移酶;AST,天门冬氨酸氨基转移酶;NT-proBNP,N末端脑钠肽前体;LVEF,左心室射血分数;NYHA,纽约心脏协会;ACEI,血管紧张素转化酶抑制剂;ARB,血管紧张素Ⅱ受体阻滞剂;ARNI,沙库巴曲缬沙坦;PNI,预后营养指数。 表 2 影响AHF患者预后的单因素和多因素分析(n=124)
变量 单因素 多因素 HR(95%CI) P HR(95%CI) P 高PNI 1 1 低PNI 6.207(2.766~13.928) <0.001 3.440(1.276~9.273) 0.015 年龄 1.054(1.018~1.091) 0.003 1.005(0.959~1.053) 0.834 Hb 0.966(0.947~0.985) <0.001 0.982(0.956~1.007) 0.162 AST 0.976(0.956~0.996) 0.018 0.978(0.954~1.003) 0.081 肌酐 1.013(1.000~1.026) 0.044 0.990(0.962~1.020) 0.514 LVEF 0.961(0.927~0.997) 0.032 0.951(0.909~0.996) 0.034 尿素氮 1.144(1.019~1.285) 0.023 1.133(0.894~1.437) 0.301 住院天数 1.151(1.034~1.280) 0.010 1.045(0.901~1.211) 0.562 NT-proBNP 1.000(1.000~1.000) <0.001 1.000(1.000~1.000) 0.005 -
[1] 中国医疗保健国际交流促进会急诊医学分会, 中华医学会急诊医学分会, 中国医师协会急诊医师分会, 等. 急性心力衰竭中国急诊管理指南(2022)[J]. 临床急诊杂志, 2022, 23(8): 519-547. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2022.08.001
[2] Buttà C, Roberto M, Tuttolomondo A, et al. Old and New Drugs for Treatment of Advanced Heart Failure[J]. Curr Pharm Des, 2020, 26(14): 1571-1583. doi: 10.2174/1381612826666191226165402
[3] Rubio-Gracia J, Josa-Laorden C, Sánchez-Marteles M, et al. Prognostic value of malnutrition in patients with acute heart failure and its influence on the interpretation of markers of systemic venous congestion[J]. Med Clin(Barc), 2021, 157(8): 371-379.
[4] Onodera T, Goseki N, Kosaki G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients[J]. Nihon Geka Gakkai Zasshi, 1984, 85(9): 1001-1005.
[5] Ma S, Zhang BP, Lu TY, et al. Value of the prognostic nutritional index(PNI)in patients with newly diagnosed, CD5-positive diffuse large B-cell lymphoma: a multicenter retrospective study of the Huaihai Lymphoma Working Group[J]. Cancer, 2022, 128(19): 3487-3494. doi: 10.1002/cncr.34405
[6] Wang Z, Zhao L, He S. Prognostic nutritional index and the risk of mortality in patients with hypertrophic cardiomyopathy[J]. Int J Cardiol, 2021, 331: 152-157. doi: 10.1016/j.ijcard.2021.01.023
[7] Liu TD, Zheng YY, Tang JN, et al. Prognostic nutritional index as a novel predictor of long-term prognosis in patients with coronary artery disease after percutaneous coronary intervention[J]. Clin Appl Thromb Hemost, 2022, 28: 10760296221103271.
[8] Cai J, Chen C, Zhang L, et al. The association between the prognostic nutritional index and 28-day mortality among atrial fibrillation patients in China over 80 years of age[J]. Nutr Metab Cardiovasc Dis, 2022, 32(6): 1493-1501. doi: 10.1016/j.numecd.2022.03.013
[9] Zencirkiran Agus H, Kahraman S. Prognostic nutritional index predicts one-year outcome in heart failure with preserved ejection fraction[J]. Acta Cardiol, 2020, 75(5): 450-455. doi: 10.1080/00015385.2019.1661139
[10] Caraballo C, Desai NR, Mulder H, et al. Clinical implications of the New York heart association classification[J]. J Am Heart Assoc, 2019, 8(23): e014240. doi: 10.1161/JAHA.119.014240
[11] Coffey S, Roberts-Thomson R, Brown A, et al. Global epidemiology of valvular heart disease[J]. Nat Rev Cardiol, 2021, 18(12): 853-864. doi: 10.1038/s41569-021-00570-z
[12] Martin M, Guffroy A, Argemi X, et al. Systemic lupus erythematosus and lymphopenia: Clinical and pathophysiological features[J]. La Revue De Médecine Interne, 2017, 38(9): 603-613. doi: 10.1016/j.revmed.2017.01.005
[13] Akbulut M, Halil G, Emre O, et al. A novel echocardiographic index for prediction of malnutrition in acute heart failure[J]. Acta Cardiol, 2022: 1-7.
[14] Kojima I, Tanaka S, Otobe Y, et al. What is the optimal nutritional assessment tool for predicting decline in the activity of daily living among older patients with heart failure?[J]. Heart Vessels, 2022, 37(8): 1356-1362. doi: 10.1007/s00380-022-02033-y
[15] Abu-Sawwa R, Dunbar SB, Quyyumi AA, et al. Nutrition intervention in heart failure: should consumption of the DASH eating pattern be recommended to improve outcomes?[J]. Heart Fail Rev, 2019, 24(4): 565-573. doi: 10.1007/s10741-019-09781-6
[16] Habaybeh D, de Moraes MB, Slee A, et al. Nutritional interventions for heart failure patients who are malnourished or at risk of malnutrition or cachexia: a systematic review and meta-analysis[J]. Heart Fail Rev, 2021, 26(5): 1103-1118. doi: 10.1007/s10741-020-09937-9
[17] Cheng YL, Sung SH, Cheng HM, et al. Prognostic nutritional index and the risk of mortality in patients with acute heart failure[J]. J Am Heart Assoc, 2017, 6(6): e004876. doi: 10.1161/JAHA.116.004876
[18] Shirakabe A, Hata N, Kobayashi N, et al. The prognostic impact of malnutrition in patients with severely decompensated acute heart failure, as assessed using the Prognostic Nutritional Index(PNI)and Controlling Nutritional Status(CONUT)score[J]. Heart Vessels, 2018, 33(2): 134-144. doi: 10.1007/s00380-017-1034-z
[19] 张彩霞, 潘满冬, 杜鹏辉, 等. 预后营养指数和γ-谷氨酰转移酶/白蛋白比值与老年急性冠脉综合征患者短期预后的相关性[J]. 临床急诊杂志, 2022, 23(6): 378-383. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2022.06.002
[20] Delcea C, Buzea CA, Dan GA. The neutrophil to lymphocyte ratio in heart failure: a comprehensive review[J]. Rom J Intern Med, 2019, 57(4): 296-314.
[21] Kałużna-Oleksy M, Krysztofiak H, Migaj J, et al. Relationship between nutritional status and clinical and biochemical parameters in hospitalized patients with heart failure with reduced ejection fraction, with 1-year follow-up[J]. Nutrients, 2020, 12(8): 2330. doi: 10.3390/nu12082330
[22] Hong XF, Yan J, Xu LY, et al. Relationship between nutritional status and frailty in hospitalized older patients[J]. Clin Interv Aging, 2019, 14: 105-111. doi: 10.2147/CIA.S189040
-




 下载:
下载: