Predictive value of neutrophil to lymphocyte and platelet ratio on acute kidney injury in patients with acute Stanford type A aortic dissection
-
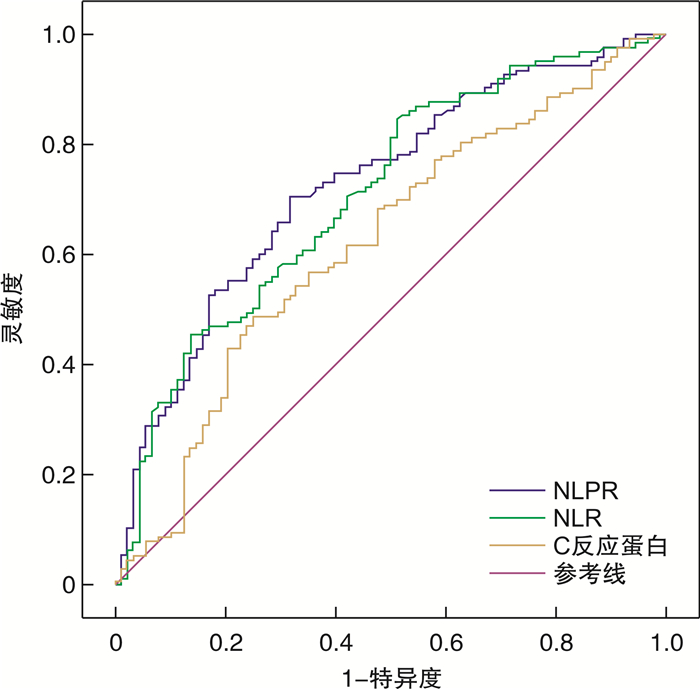
摘要: 目的探讨中性粒细胞与淋巴细胞和血小板比值(NLPR)对急性Stanford A型主动脉夹层(ATAAD)患者急性肾损伤(AKI)早期预测的临床价值。方法回顾性分析南京医科大学附属南京医院重症医学科收治的211例ATAAD患者的临床资料,根据2012 KDIGO-AKI标准将患者分为急性肾损伤组(AKI组)和非急性肾损伤组(非AKI组),通过logistic回归评估AKI的独立危险因素,并通过ROC曲线和曲线下面积(AUC)评价NLPR等指标对AKI的预测价值。结果纳入患者中AKI组123例,非AKI组88例,AKI发病率为58.3%;AKI组NLPR显著高于非AKI组,差异有统计学意义(P < 0.01)。与非AKI组相比,AKI组术后机械通气时间更长(P < 0.05)、住ICU时间均更长(P < 0.01),院内病死率增加(P < 0.01),需要呋塞米静脉泵入治疗的比例更高(P < 0.01),以及肾脏替代治疗的比例更高(P < 0.01)。多因素logistic回归分析显示:NLPR(OR=1.118,95%CI:1.055~1.186,P < 0.01)是ATAAD患者AKI的独立危险因素,ROC曲线显示了NLPR对AKI具有较好的预测价值。结论NLPR作为一种新型炎症指标,是ATAAD患者AKI的独立危险因素,对AKI的发生有良好的早期预测价值。Abstract: ObjectiveTo investigate the clinical value of neutrophil to lymphocyte and platelet ratio(NLPR) for acute kidney injury(AKI) in patients with acute Stanford type A aortic dissection(ATAAD).MethodsThe clinical data of 211 ATAAD patients admitted to Intensive Care Unit, Nanjing Hospital Affiliated to Nanjing Medical University were retrospectively analyzed. The patients were divided into acute kidney injury group(AKI group) and non-acute kidney injury group(non-AKI group) based on 2012 KDIGO-AKI criteria. The independent risk factors of AKI were identified via logistic analysis, and the predictive value of NLPR and other indicators for AKI was evaluated by the calculation of receiver operating characteristic(ROC) curve and area under the curve(AUC).ResultsThere were 123 patients in the AKI group and 88 patients in the non-AKI group, and the incidence of AKI was 58.3%. The NLPR in AKI group was significantly higher than that in the non-AKI group(P < 0.01). Compared with the non-AKI group, the AKI group had longer postoperative mechanical ventilation time(P < 0.05) and longer ICU stay time(P < 0.01), increased in-hospital mortality(P < 0.01), higher proportion of patients requiring intravenous furosemide therapy(P < 0.01), and higher proportion of patients requiring renal replacement therapy(P < 0.01). Multivariate logistic regression analysis showed that: NLPR was an independent risk factor for AKI in ATAAD patients(OR=1.118, 95%CI: 1.055-1.186,P < 0.01), and the ROC curve showed that NLPR had a good predictive value.ConclusionAs a novel inflammatory index, NLPR is an independent risk factor for AKI in ATAAD patients, and has a good early predictive value for the occurrence of AKI.
-
Key words:
- acute Stanford type A aortic dissection /
- acute kidney injury /
- neutrophil /
- lymphocyte /
- platelet /
- ratio /
- predictive value
-

-
表 1 两组患者术前基本临床资料的对比
临床资料 总体(211例) AKI组(123例) 非AKI组(88例) P 年龄/岁 53(47,59) 54(47,59) 53(47,58) 0.494 男性/例(%) 161(76.3) 95(77.2) 66(75.6) 0.706 体重/kg 75(64,85) 73(64,83) 75(65,86) 0.525 高血压/例(%) 163(77.3) 102(82.9) 61(69.3) < 0.05 糖尿病/例(%) 13(6.2) 9(7.3) 4(4.5) 0.564 吸烟/例(%) 54(25.6) 34(27.6) 20(22.7) 0.420 左室射血分数/% 59(55,64) 58(54,64) 61(56,65) < 0.05 APACHEⅡ/分 12(9,15) 12(9,15) 10.5(9,15) 0.110 WBC/(×109·L-1) 12.25(9.96,15.29) 12.80(10.12,15.73) 11.53(9.73,14.24) < 0.05 NEUT/(×109·L-1) 10.56(8.37,13.67) 11.43(9.08,14.12) 9.83(7.88,12.07) < 0.01 LYM/(×109·L-1) 0.89(0.66,1.19) 0.77(0.59,1.05) 1.09(0.78,1.43) < 0.01 PLT/(×109·L-1) 157(131,192) 153(126,184) 166(140,201) < 0.05 NLR 12.35(8.42,18.65) 14.02(10.18,20.78) 9.99(6.03,14.05) < 0.01 NLPR 7.55(4.93,12.50) 9.80(6.17,15.64) 5.79(3.67,8.36) < 0.01 Scr/(μmol·L-1) 76.1(61,93.3) 75.9(63.2,94.0) 76.9(60.4,90.4) 0.413 BUN/(mmol·L-1) 6.42(5.06,7.65) 6.88(5.35,7.70) 6.08(4.82,7.54) < 0.05 CRP/(mg·L-1) 64.05(32.49,102.72) 76.74(41.51,109.30) 48.88(24.79,79.53) < 0.01 PaO2/FiO2/mmHg 275(227,331) 275(221,328) 276(233,331) 0.271 注:1 mmHg=0.133kPa。 表 2 两组患者手术相关临床资料及术后观察指标对比
项目 总体(211例) AKI组(123例) 非AKI组(88例) P Scr最高值/(μmol·L-1) 131.8(97.0,211.0) 151.0(123.0,250.4) 90.2(76.1,105.1) < 0.01 血红蛋白/(g·L-1) 88(75,100) 89(78,101) 87(75,100) 0.361 白蛋白/(g·L-1) 30.6(26.2,34.1) 30.5(27.0,33.1) 31.1(25.5,34.4) 0.442 体外循环时间/min 210(182,257) 220(188,270) 197(180,229) < 0.01 主动脉阻断时间/min 142(112,172) 157(122,203) 128(94,129) < 0.01 术中失血量/mL 590(410,770) 630(390,860) 570(430,688) 0.133 术后24 h输血量/mL 950(670,1200) 970(650,1250) 925(723,1160) 0.772 术后24 h引流量/mL 490(350,610) 530(360,640) 455(350,590) 0.215 表 3 两组患者术后不良事件及临床转归的对比
项目 总体(211例) AKI组(123例) 非AKI组(88例) P 机械通气时间/h 68(54,83) 71(58,85) 61(50,76) < 0.05 肾脏替代治疗/例(%) 19(9.0) 19(15.4) 0(0) < 0.01 呋塞米泵入治疗/例(%) 54(24.4) 52(39.1) 2(2.3) < 0.01 住ICU时间/d 6.1(4.2,7.9) 6.7(4.5,8.9) 5.5(4.1,7.0) < 0.01 院内死亡/例(%) 21(10.0) 19(15.4) 2(2.3) < 0.01 出院/死亡时Scr/(μmol·L-1) 74.0(59.0,99.3) 82.3(64.0,108.0) 70.0(53.8,83.0) < 0.01 表 4 logistic回归分析ATAAD患者发生AKI的危险因素
项目 单因素logistic回归分析 多因素logistic回归分析 OR 95%CI P OR 95%CI P 高血压病 2.150 1.119~4.129 0.022 2.041 1.005~4.146 0.048 左室射血分数 0.948 0.901~0.999 0.044 CRP 1.008 1.002~1.013 0.011 1.006 1.000~1.013 0.044 NLPR 1.125 1.062~1.192 < 0.001 1.118 1.055~1.186 < 0.001 体外循环时间 1.008 1.002~1.014 0.011 1.007 1.001~1.014 0.027 表 5 NLPR、NLR及CRP与ATAAD患者AKI的预测价值
预测指标 预测界值 灵敏度/% 特异度/% AUC 95%CI P 标准误 NLPR 7.05 70.7 68.2 0.727 0.658~0.796 < 0.001 0.035 NLR 9.21 84.6 48.9 0.710 0.640~0.781 < 0.001 0.036 CRP 79.41 48.8 75.0 0.622 0.545~0.699 0.002 0.039 -
[1] Sheikh AS, Ali K, Mazhar S. Acute aortic syndrome[J]. Circulation, 2013, 128(10): 1122-1127. doi: 10.1161/CIRCULATIONAHA.112.000170
[2] Pape LA, Awais M, Woznicki EM, et al. Presentation, diagnosis, and outcomes of acute aortic dissection: 17-year trends from the international registry of acute aortic dissection[J]. J Am Coll Cardiol, 2015, 66(4): 350-358. doi: 10.1016/j.jacc.2015.05.029
[3] Erbel R, Aboyans V, Boileau C, et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The task force for the diagnosis and treatment of aortic diseases of the European Society of Cardiology(ESC)[J]. Eur Heart J, 2014, 35(41): 2873-2926. doi: 10.1093/eurheartj/ehu281
[4] Tsai HS, Tsai FC, Chen YC, et al. Impact of acute kidney injury on one-year survival after surgery for aortic dissection[J]. Ann Thorac Surg, 2012, 94(5): 1407-1412. doi: 10.1016/j.athoracsur.2012.05.104
[5] Wu HB, Ma WG, Zhao HL, et al. Risk factors for continuous renal replacement therapy after surgical repair of type A aortic dissection[J]. J Thorac Dis, 2017, 9(4): 1126-1132. doi: 10.21037/jtd.2017.03.128
[6] Amano K, Takami Y, Ishikawa H, et al. Lower body ischaemic time is a risk factor for acute kidney injury after surgery for type A acute aortic dissection[J]. Interact Cardiovasc Thorac Surg, 2020, 30(1): 107-112. doi: 10.1093/icvts/ivz220
[7] Sasabuchi Y, Kimura N, Shiotsuka J, et al. Long-Term Survival in Patients With Acute Kidney Injury After Acute Type A Aortic Dissection Repair[J]. Ann Thorac Surg, 2016, 102(6): 2003-2009. doi: 10.1016/j.athoracsur.2016.05.006
[8] Karkouti K. Transfusion and risk of acute kidney injury in cardiac surgery[J]. Br J Anaesth, 2012, 109(Suppl 1): 29-38.
[9] Peerapornratana S, Manrique-Caballero CL, Gómez H, et al. Acute kidney injury from sepsis: current concepts, epidemiology, pathophysiology, prevention and treatment[J]. Kidney Int, 2019, 96(5): 1083-1099. doi: 10.1016/j.kint.2019.05.026
[10] Gameiro J, Fonseca JA, Jorge S, et al. Neutrophil, lymphocyte and platelet ratio as a predictor of mortality in septic-acute kidney injury patients[J]. Nefrologia(Engl Ed), 2020, 40(4): 461-468.
[11] Mae Y, Takata T, Ida A, et al. Prognostic value of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio for renal outcomes in patients with rapidly progressive glomerulonephritis[J]. J Clin Med, 2020, 9(4): 1128. doi: 10.3390/jcm9041128
[12] Yu GQ, Zhang Q, Wang RC, et al. Predictive value of neutrophilto-lymphocyte ratio and other inflammatory indicators in estimating clinical severity of coronavirus disease[J]. World J Emerg Med, 2021, 12(1): 79-80. doi: 10.5847/wjem.j.1920-8642.2021.01.014
[13] Nagareddy P, Smyth SS. Inflammation and thrombosis in cardiovascular disease[J]. Curr Opin Hematol, 2013, 20(5): 457-463. doi: 10.1097/MOH.0b013e328364219d
[14] Kidney Disease Improving Global Outcomes(KDIGO)Acute Kidney Injmy Work Group. KDIGO clinical practice guideline for acute kidney injury[J]. Kidney Int Suppl, 2012, 2(suppl 1): 1-138.
[15] Ahsen A, Ulu MS, Yuksel S, et al. As a new inflammatory marker for familial Mediterranean fever: neutrophil-to-lymphocyte ratio[J]. Inflammation, 2013, 36(6): 1357-1362. doi: 10.1007/s10753-013-9675-2
[16] Wada H, Dohi T, Miyauchi K, et al. Pre-procedural neutrophil-to-lymphocyte ratio and long-term cardiac outcomes after percutaneous coronary intervention for stable coronary artery disease[J]. Atherosclerosis, 2017, 265: 35-40. doi: 10.1016/j.atherosclerosis.2017.08.007
[17] Hwang SY, Shin TG, Jo IJ, et al. Neutrophil-to-lymphocyte ratio as a prognostic marker in critically-ill septic patients[J]. Am J Emerg Med, 2017, 35(2): 234-239. doi: 10.1016/j.ajem.2016.10.055
[18] 潘树滨, 张芳晓, 马晓春, 等. 中性粒细胞/淋巴细胞比值早期预测脓毒症器官功能损伤及28 d病死率的临床价值[J]. 中华危重病急救医学, 2021, 33(6): 665-670. doi: 10.3760/cma.j.cn121430-20210325-00437
[19] Salciccioli JD, Marshall DC, Pimentel MA, et al. The association between the neutrophil-to-lymphocyte ratio and mortality in critical illness: an observational cohort study[J]. Crit Care, 2015, 19(1): 13. doi: 10.1186/s13054-014-0731-6
[20] Ma AJ, Cheng JL, Yang J, et al. Neutrophil-to-lymphocyte ratio as a predictive biomarker for moderate-severe ARDS in severe COVID-19 patients[J]. Crit Care, 2020, 24(1): 288. doi: 10.1186/s13054-020-03007-0
[21] 卢志, 王立华, 贾岚, 等. 中性粒细胞与淋巴细胞比值对急性肾损伤预测作用的Meta分析[J]. 中华危重病急救医学, 2021, 33(3): 311-317. doi: 10.3760/cma.j.cn121430-20201215-00755
[22] Fan LL, Wang YJ, Nan CJ, et al. Neutrophil-lymphocyte ratio is associated with all-cause mortality among critically ill patients with acute kidney injury[J]. Clin Chim Acta, 2019, 490: 207-213. doi: 10.1016/j.cca.2018.09.014
[23] Parlar H, Şaşkın H. Are Pre and Postoperative Platelet to Lymphocyte Ratio and Neutrophil to Lymphocyte Ratio Associated with Early Postoperative AKI Following CABG[J]? Braz J Cardiovasc Surg, 2018, 33(3): 233-241.
[24] Yilmaz H, Cakmak M, Inan O, et al. Can neutrophil-lymphocyte ratio be independent risk factor for predicting acute kidney injury in patients with severe sepsis[J]? Renal Failure, 2015, 37(2): 225-229. doi: 10.3109/0886022X.2014.982477
[25] Bu X, Zhang L, Chen P, et al. Relation of neutrophil-to-lymphocyte ratio to acute kidney injury in patients with sepsis and septic shock: A retrospective study[J]. Int Immunopharmacol, 2019, 70: 372-377. doi: 10.1016/j.intimp.2019.02.043
[26] Koo CH, Eun Jung D, Park YS, et al. Neutrophil, lymphocyte, and platelet counts and acute kidney injury after cardiovascular surgery[J]. J Cardiothorac Vasc Anesth, 2018, 32(1): 212-222. doi: 10.1053/j.jvca.2017.08.033
[27] Gameiro J, Fonseca JA, Dias JM, et al. Neutrophil, lymphocyte and platelet ratio as a predictor of postoperative acute kidney injury in major abdominal surgery[J]. BMC Nephrol, 2018, 19(1): 320. doi: 10.1186/s12882-018-1073-4
[28] Jansen MPB, Florquin S, Roelofs JJTH. The role of platelets in acute kidney injury[J]. Nat Rev Nephrol, 2018, 14(7): 457-471. doi: 10.1038/s41581-018-0015-5
[29] Sbarouni E, Georgiadou P, Analitis A, et al. Significant changes in platelet count, volume and size in acute aortic dissection[J]. Int J Cardiol, 2013, 168(4): 4349-4350. doi: 10.1016/j.ijcard.2013.05.074
[30] Zhang S, Qian H, Yang Q, et al. Relationship between the extent of dissection and platelet activation in acute aortic dissection[J]. J Cardiothorac Surg, 2015, 10: 162. doi: 10.1186/s13019-015-0351-5
[31] Huang B, Tian L, Fan X, et al. Low admission platelet counts predicts increased risk of in-hospital mortality in patients with type A acute aortic dissection[J]. Int J Cardiol, 2014, 172(3): e484-e486. doi: 10.1016/j.ijcard.2014.01.001
[32] Itagaki R, Kimura N, Mieno M, et al. Characteristics and treatment outcomes of acute type a aortic dissection with elevated D-dimer concentration[J]. J Am Heart Assoc, 2018, 7(14): e009144. doi: 10.1161/JAHA.118.009144
-




 下载:
下载: