Prediction value of age adjusted charlson comorbidity index in prognosis of sepsis patients
-
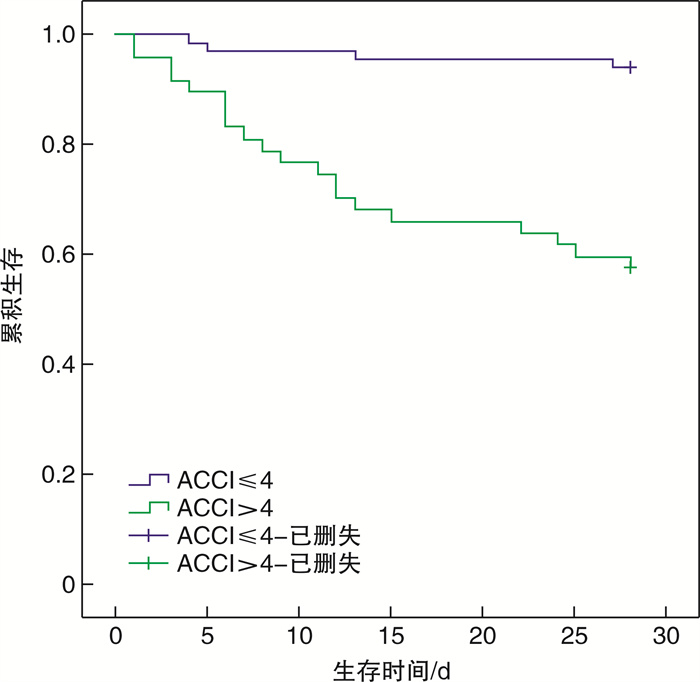
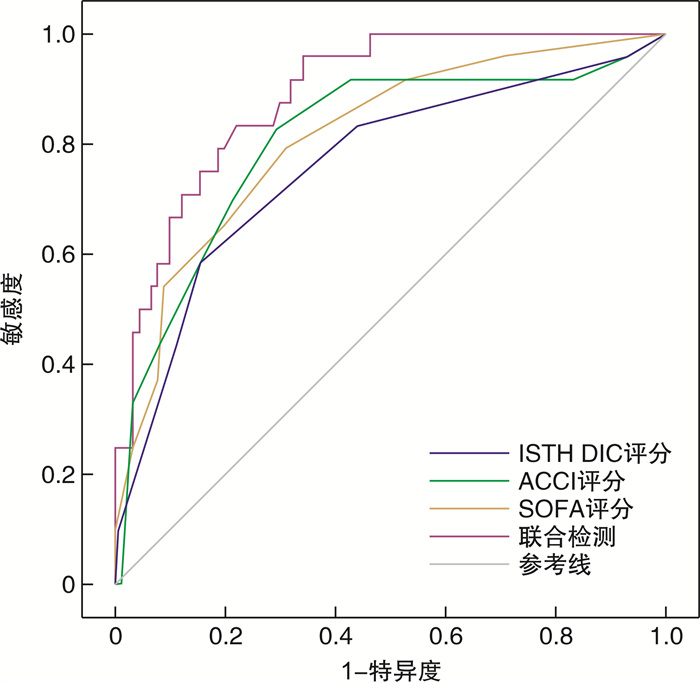
摘要: 目的 探讨年龄校准的查尔森共病指数(ACCI)预测脓毒症患者预后的应用价值。方法 选择2018年8月-2019年9月期间在上海交通大学医学院附属仁济医院急诊科普通病房住院的脓毒症患者作为研究对象。收集患者的基本资料、入住急诊科普通病房24 h内各项生化指标的最差值以及ACCI评分、序贯器官衰竭评分(SOFA)、国际血栓与止血学会弥散性血管内凝血(ISTH DIC)评分等指标。根据28 d预后情况将患者分为存活组和死亡组,比较2组患者各项指标的差异;并进行二元多因素logistic回归分析,找出患者28 d死亡的独立危险因素;绘制受试者工作特征曲线(ROC)评估ACCI评分、SOFA评分和ISTH DIC评分以及三者联合对于脓毒症患者28 d预后的预测价值;根据ACCI评分预测预后的最佳截断值并分组,比较2组患者各种指标的差异;生存资料分析采用Kaplan-Meier方法绘制生存曲线,组间生存率的比较采用log-rank检验。结果 共纳入115例脓毒症患者,其中28 d存活91例,死亡24例,病死率为20.87%;死亡组的脓毒症患者的ACCI评分、SOFA评分、ISTH DIC评分、年龄、平均每天住院费用、D-二聚体明显高于存活组患者,BMI、血小板计数、纤维蛋白原明显低于存活组,将2组间差异有统计学意义的指标纳入二元多因素logistic回归分析显示,影响患者预后的独立危险因素为ACCI评分、SOFA评分以及BMI;ROC曲线分析显示,ACCI评分、SOFA评分、ISTH DIC评分及三者联合检测评估脓毒症患者28 d预后的曲线下面积分别是0.807、0.812、0.762、0.890;ACCI评分预测脓毒症患者28 d预后的最佳截断值为4.5分,此时敏感度为83.3%,特异度为70.3%;与ACCI评分≤4分组相比,ACCI评分>4分组的年龄、凝血酶原时间、SOFA评分、ISTH DIC评分、平均每天住院费用更高,BMI、纤维蛋白原更低;Kaplan-Meier生存分析显示,ACCI评分>4分组28 d的累计生存率明显低于ACCI评分≤4分组,均差异有统计学意义(P< 0.05)。结论 ACCI评分可以作为一种预测脓毒症患者不良预后的指标。
-
关键词:
- 脓毒症 /
- 年龄校准的查尔森共病指数 /
- 预后
Abstract: Objective To explore the value of age adjusted charlson comorbidity index(ACCI) in predicting the prognosis of sepsis patients.Methods The patients with sepsis admitted in the General ward of Department of Emergency, Renji Hospital Affiliated to Shanghai Jiaotong University School of Medicine form August 2018 to September 2019 were selected as the research subjects. Basic patient data, the worst values of various biochemical indicators within 24 h, ACCI score, sequential organ failure assessment(SOFA) score, International Society on Thrombosis and Haemostasis(ISTH DIC) score and other indicators were collected. Patients were divided into survival group and death group based on the 28-day prognosis, and the differences of each index between the two groups were compared; multivariate binary logistic regression analysis was carried out to identify the independent risk factors for patient death at 28 days.The receiver operating characteristic(ROC) curve was drawn to evaluate the value of the ACCI score, SOFA score, ISTH DIC score and combined prediction for predicting the 28-day prognosis of patients with sepsis. According to the threshold value of ACCI score in predicting prognosis, the patients were divided into two groups, and the differences of various indicators between the two groups were compared; survival data was analyzed using the Kaplan-Meier method to draw survival curves, and intergroup comparison of survival rates was performed using log-rank test.Results In this study, 115 eligible sepsis patients were enrolled, and 91 patients survived at 28 days, and 24 patients died with a 28-day mortality of 20.87%; the ACCI score, SOFA score, ISTH DIC score, age, average daily hospital stay cost and D-Dimer in the death group were significantly higher than those in the survival group, in addition, the BMI, platelet counts and fibrinogen were further decreased compared with the survival group, including statistically significant indicators between the two groups into multivariate binary logistic regression analysis, the result showed that the independent risk factors affecting the prognosis of patients were the ACCI score, SOFA score, and BMI; ROC curve analysis showed that the area under ROC curve(AUC) of ACCI score, SOFA score, ISTH DIC score and combined prediction probability were 0.807, 0.812, 0.762 and 0.890, respectively. When the cut-off point of the ACCI score predicting 28-day prognosis in sepsis was 4.5 points, the sensitivity and specificity were 83.3% and 70.3%; compared with the group with ACCI score lower than 4 points, age, SOFA score, ISTH DIC score, BNP, prothrombin time, average daily hospital stay cost were significant higher, BMI, fibrinogen were further decreased in the group with ACCI score greater than 4 points. The Kaplan-Meier survival analysis showed that the 28-day cumulative survival rate was significantly lower in the group with ACCI score greater than 4 points than in group with ACCI score lower than 4 points, the differences were all statistically significant(P< 0.05).Conclusion ACCI can be used as an indicator for predicting a poor prognosis in patients with sepsis.-
Key words:
- sepsis /
- age adjusted charlson comorbidity index /
- prognosis
-

-
表 1 存活组与死亡组入院时基本资料的比较
例(%),M(Q),X±S 基本资料 总例数(n=115) 存活组(n=91) 死亡组(n=24) χ2/t/Z P 性别 男 67(58.3) 54(59.3) 13(54.2) 0.209 0.647 女 48(41.7) 37(40.7) 11(45.8) 年龄/岁 66(22) 64(20) 80(25) 2.121 0.034 BMI 23.38±4.33 23.96±4.06 21.20±4.70 2.867 0.005 住院费用/元 37 354.75(36 687.30) 36 382.14(38 510.25) 51 119.41(41 467.54) 1.032 0.302 平均每天住院费用/元 3 513.79(2 165.33) 3 257.94(1 746.41) 5 917.50(2 631.99) 4.935 < 0.001 表 2 存活组与死亡组入院时生化资料及3种评分的比较
M(Q),X±S 生化资料及评分 总例数(n=115) 存活组(n=91) 死亡组(n=24) Z/t P CRP/(mg·L-1) 131.33(132.57) 125.37(138.27) 152.87(126.07) 0.613 0.540 白细胞计数/(×109·L-1) 12.39(9.06) 12.53(8.95) 11.90(9.45) 0.344 0.731 血红蛋白/(g·L-1) 119(35) 120(35) 116(38) -0.922 0.356 血小板计数/(×109·L-1) 140(134) 149(133) 105(138) -2.498 0.012 凝血酶原时间/s 13.0(3.0) 12.9(2.5) 13.2(4.1) 1.735 0.083 纤维蛋白原/(g·L-1) 4.76±1.90 4.97±1.90 3.98±1.70 2.328 0.022 D-二聚体/(mg·L-1) 1.91(2.86) 1.61(1.75) 4.96(10.72) 3.541 < 0.001 降钙素原/(ng·mL-1) 1.92(14.03) 1.54(14.71) 2.24(10.11) 0.485 0.627 ACCI评分/分 4(4) 3(3) 7(3) 4.656 < 0.001 SOFA评分/分 4(3) 4(3) 7(4) 4.767 < 0.001 ISTH DIC评分/分 3(1) 2(1) 4(2) 4.130 < 0.001 表 3 脓毒症患者28 d预后影响因素的logistic回归分析
危险因素 β SE χ2 P OR 95%CI ACCI评分 0.444 0.142 9.838 0.002 1.559 1.181~2.058 SOFA评分 0.584 0.155 14.200 < 0.001 1.793 1.323~2.429 BMI -0.197 0.084 5.445 0.020 0.821 0.696~0.969 表 4 ACCI评分、SOFA评分、ISTH DIC评分及三者联合检测预测脓毒症患者预后的价值
指标 AUC 95%CI P 最佳截断值 敏感度 特异度 ISTH DIC评分 0.762 0.646~0.877 < 0.001 3.5 0.583 0.846 ACCI评分 0.807 0.700~0.915 < 0.001 4.5 0.833 0.703 SOFA评分 0.812 0.715~0.910 < 0.001 4.5 0.792 0.692 联合检测 0.890 0.827~0.954 < 0.001 0.1 0.958 0.659 表 5 ACCI评分≤4分组与ACCI评分>4分组脓毒症患者各项指标的比较
M(Q),X±S 变量 ACCI评分≤4分(n=68) ACCI评分>4分(n=47) Z/t P 年龄/岁 60(18) 80(15) 6.044 < 0.001 BMI 24.06±4.15 22.41±4.43 2.035 0.044 凝血酶原时间/s 12.7(2.2) 13.4(3.6) 2.336 0.019 纤维蛋白原/(g·L-1) 5.13±1.89 4.24±1.81 2.511 0.013 平均每天住院费用/元 3 338.02(2 002.75) 3 981.08(2 516.35) 2.122 0.034 SOFA评分/分 3.5(3) 5(3) 3.136 0.002 ISTH DIC评分/分 2(1) 3(2) 3.471 0.001 -
[1] Fleischmann C, Scherag A, Adhikari NK, et al. Assessment of Global Incidence and Mortality of Hospital-treated Sepsis. Current Estimates and Limitations[J]. Am J Respir Crit Care Med, 2016, 193(3): 259-272. doi: 10.1164/rccm.201504-0781OC
[2] Tiru B, DiNino EK, Orenstein A, et al. The Economic and Humanistic Burden of Severe Sepsis[J]. Pharmacoeconomics, 2015, 33(9): 925-937. doi: 10.1007/s40273-015-0282-y
[3] 中国医疗保健国际交流促进会急诊医学分会, 中华医学会急诊医学分会, 中国医师协会急诊医师分会, 等. 中国脓毒症早期预防与阻断急诊专家共识[J]. 临床急诊杂志, 2020, 21(7): 517-529. http://zzlc.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=c441f903-8d56-4e1e-bc33-972383f6cb59
[4] Hotchkiss RS, Moldawer LL, Opal SM, et al. Sepsis and septic shock[J]. Nat Rev Dis Primers, 2016, 2: 16045. doi: 10.1038/nrdp.2016.45
[5] Singer E, Markó L, Paragas N, et al. Neutrophil gelatinase-associated lipocalin: pathophysiology and clinical applications[J]. Acta Physiol(Oxf), 2013, 207(4): 663-672. doi: 10.1111/apha.12054
[6] Marshall JC. Why have clinical trials in sepsis failed?[J]. Trends Mol Med, 2014, 20(4): 195-203. doi: 10.1016/j.molmed.2014.01.007
[7] Charlson M, Szatrowski TP, Peterson J, et al. Validation of a combined comorbidity index[J]. J Clin Epidemiol, 1994, 47(11): 1245-1251. doi: 10.1016/0895-4356(94)90129-5
[8] Yang CC, Fong Y, Lin LC, et al. The age-adjusted Charlson comorbidity index is a better predictor of survival in operated lung cancer patients than the Charlson and Elixhauser comorbidity indices[J]. Eur J Cardiothorac Surg, 2018, 53(1): 235-240. doi: 10.1093/ejcts/ezx215
[9] Cildir E, Bulut M, Akalin H, et al. Evaluation of the modified MEDS, MEWS score and Charlson comorbidity index in patients with community acquired sepsis in the emergency department[J]. Intern Emerg Med, 2013, 8(3): 255-260. doi: 10.1007/s11739-012-0890-x
[10] 张晓勤, 王茜, 罗晓秀, 等. 查尔森合并症指数及序贯器官衰竭评分联合降钙素原对脓毒症患者预后的评估价值[J]. 中华危重病急救医学, 2019, 31(11): 1335-1339. doi: 10.3760/cma.j.issn.2095-4352.2019.11.005
[11] Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock(Sepsis-3)[J]. JAMA, 2016, 315(8): 801-810. doi: 10.1001/jama.2016.0287
[12] Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation[J]. J Chronic Dis, 1987, 40(5): 373-383. doi: 10.1016/0021-9681(87)90171-8
[13] Kahl A, du Bois A, Harter P, et al. Prognostic Value of the Age-Adjusted Charlson Comorbidity Index(ACCI)on Short-and Long-Term Outcome in Patients with Advanced Primary Epithelial Ovarian Cancer[J]. Ann Surg Oncol, 2017, 24(12): 3692-3699. doi: 10.1245/s10434-017-6079-9
[14] Liu Z, Meng Z, Li Y, et al. Prognostic accuracy of the serum lactate level, the SOFA score and the qSOFA score for mortality among adults with Sepsis[J]. Scand J Trauma Resusc Emerg Med, 2019, 27(1): 51. doi: 10.1186/s13049-019-0609-3
[15] Hu T, Lv H, Jiang Y. The association between four scoring systems and 30-day mortality among intensive care patients with sepsis: a cohort study[J]. Sci Rep, 2021, 11(1): 11214. doi: 10.1038/s41598-021-90806-2
[16] Suzuki J, Sasabuchi Y, Hatakeyama S, et al. The effect of antithrombin added to recombinant human-soluble thrombomodulin for severe community-acquired pneumonia-associated disseminated intravascular coagulation: a retrospective cohort study using a nationwide inpatient database[J]. J Intensive Care, 2020, 8: 8. doi: 10.1186/s40560-019-0419-8
[17] Helms J, Severac F, Merdji H, et al. Performances of disseminated intravascular coagulation scoring systems in septic shock patients[J]. Ann Intensive Care, 2020, 10(1): 92. doi: 10.1186/s13613-020-00704-5
[18] Iba T, Levi M, Levy JH. Sepsis-Induced Coagulopathy and Disseminated Intravascular Coagulation[J]. Semin Thromb Hemost, 2020, 46(1): 89-95. doi: 10.1055/s-0039-1694995
[19] Taylor FB Jr, Toh CH, Hoots WK, et al. Scientific Subcommittee on Disseminated Intravascular Coagulation(DIC)of the International Society on Thrombosis and Haemostasis(ISTH). Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation[J]. Thromb Haemost, 2001, 86(5): 1327-1330.
[20] Gando S, Levi M, Toh CH. Disseminated intravascular coagulation[J]. Nat Rev Dis Primers, 2016, 2: 16037. doi: 10.1038/nrdp.2016.37
[21] Ding R, Wang Z, Lin Y, et al. Comparison of a new criteria for sepsis-induced coagulopathy and International Society on Thrombosis and Haemostasis disseminated intravascular coagulation score in critically ill patients with sepsis 3.0: a retrospective study[J]. Blood Coagul Fibrinolysis, 2018, 29(6): 551-558. doi: 10.1097/MBC.0000000000000755
[22] Yin Q, Liu B, Chen Y, et al. Prognostic value of the International Society on Thrombosis and Haemostasis scoring system for overt disseminated intravascular coagulation in emergency department sepsis[J]. Infection, 2014, 42(4): 629-637. doi: 10.1007/s15010-014-0600-x
-




 下载:
下载: