The relationship between the level of HDL-C and the severity of coronary artery disease and its influence on the prognosis of interventional procedures
-
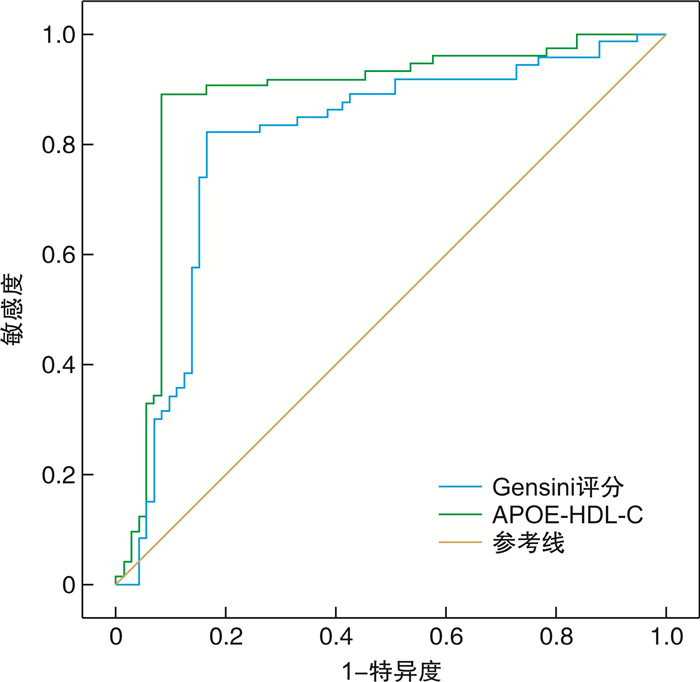
摘要: 目的 探讨HDL-C水平与冠脉病变严重程度的关系及对介入预后的影响。方法 选择2019年1月—2019年12月期间在我院行介入治疗的96例急性冠脉综合征患者进行回顾性分析,收集患者一般资料、实验室检查结果及Gensini评分。根据介入治疗后有无MACE将患者分为两组,比较两组患者上述各指标,并采用多因素logistic回归分析判断各因素的综合作用。相关性分析采用Pearson相关系数法,并以ROC分析评估载脂蛋白E的HDL-C(APOE-HDL-C)及Gensini评分对介入治疗预后的预测价值。结果 单因素分析基础上多因素logistic回归分析结果显示:有吸烟史、糖尿病、Gensini评分升高为介入治疗后MACE发生的危险因素,APOE-HDL-C升高为保护性因素(P< 0.05)。APOE-HDL-C与Gensini评分呈负相关(r=-0.693,P< 0.05)。ROC分析结果显示Gensini评分、APOE-HDL-C对介入治疗后发生MACE的预测截断值分别为42分,4.96 mg/dL;曲线下面积(AUC)分别为0.803(95%CI0.726~0.880)、0.879(95%CI0.814~0.943),当APOE-HDL-C为4.96 mg/dL时敏感度为79.17%,特异度为84.19%(P< 0.05)。结论 急性冠脉综合征患者介入治疗后MACE的发生主要受吸烟史、糖尿病、APOE-HDL-C水平与Gensini评分的影响,APOE-HDL-C水平与Gensini评分呈负相关关系,两者均可作为介入治疗后发生MACE的预测指标。Abstract: Objective To investigate the relationship between the level of HDL-C and the severity of coronary artery disease and its influence on the prognosis of interventional procedures.Methods Ninty-six patients with acute coronary syndrome who received interventional therapy in our hospital from January 2019 to December 2019 were selected for retrospective analysis, and general data, laboratory test results and Gensini score of the patients were collected.The patients were divided into 2 groups according to the presence or absence of MACE after interventional treatment. The above indicators of the 2 groups were compared, and multivariate logistic regression analysis was used to judge the comprehensive effect of each factor. Correlation analysis adopts Pearson correlation coefficient method, and ROC analysis is used to evaluate the predictive value of APOE-HDL-C and Gensini score for the prognosis of interventional therapy.Results Multivariate logistic regression analysis based on univariate analysis showed that smoking history, diabetes, and elevated Gensini score were risk factors for MACE after interventional therapy, and elevated APOE-HDL-C were protective factors(P< 0.05). There was a negative correlation between APOE-HDL-C and Gensini score(r=-0.693,P< 0.05). ROC analysis results showed that the cut-off values of Gensini score and APOE-HDL-C for MACE after interventional therapy were 42 points, 4.96 mg/dL; Area under the curve(AUC) were 0.803(95%CI0.726-0.880), 0.879(95%CI0.814-0.943). When APOE-HDL-C is 4.96 mg/dL, the sensitivity is 79.17% and the specificity is 84.19%(P< 0.05).Conclusion The incidence of MACE in patients with ACS after PCI is mainly affected by smoking history, diabetes, APOE-HDL-C level and Gensini score. There is a negative correlation between APOE-HDL-C level and Gensini score, both of which can be used as predictors of MACE after PCI.
-

-
表 1 两组一般资料及实验室指标比较
例,X±S 因素 MACE组(26例) 无MACE组(70例) χ2/t P 性别 男 18 33 4.190 0.041 女 8 37 年龄/岁 67.08±14.11 60.16±13.97 2.151 0.034 吸烟史 有 19 30 6.928 0.008 无 7 40 饮酒史 有 9 29 0.368 0.544 无 17 41 糖尿病 有 11 15 4.185 0.041 无 15 55 高血压 有 16 39 0.263 0.608 无 10 31 BMI 23.56±4.11 23.49±3.92 0.077 0.939 总胆固醇/(mmol·L-1) 4.21±1.03 4.27±1.08 -0.245 0.807 三酰甘油/(mmol·L-1) 1.83±0.52 1.71±0.55 0.964 0.338 LDL-C/(mmol·L-1) 2.57±0.73 2.19±0.64 2.488 0.015 HDL-C/(mmol·L-1) 1.04±0.27 1.19±0.25 -2.557 0.012 APOE-HDL-C/(mg·dL-1) 5.42±1.63 4.68±1.57 2.031 0.045 尿酸/(μmol·L-1) 342.17±96.02 329.83±102.77 1.020 0.309 肌酐/(μmol·L-1) 72.49±18.53 73.92±21.03 -0.585 0.559 谷丙转氨酶/(U·L-1) 31.68±9.33 32.04±9.75 -0.312 0.756 Gensini评分/分 61.27±14.82 38.93±7.85 18.198 < 0.001 表 2 各因素赋值情况
因素 赋值 性别 男=0,女=1 年龄 原值代入 吸烟史 无=0,有=1 糖尿病 无=0,有=1 LDL-C 原值代入 HDL-C 原值代入 APOE-HDL-C 原值代入 Gensini评分 原值代入 表 3 介入治疗后MACE发生情况的多因素分析
变量 β S.E Wald P OR 95%CI 下限 上限 女性 -0.302 0.156 3.748 0.053 0.739 0.545 1.004 年龄增加 0.211 0.154 1.877 0.171 1.235 0.913 1.670 有吸烟史 0.378 0.192 3.876 0.049 1.459 1.002 2.126 糖尿病 0.395 0.171 5.336 0.021 1.484 1.027 2.146 LDL-C升高 0.257 0.173 2.207 0.137 1.293 0.921 1.815 HDL-C升高 -0.311 0.185 2.826 0.093 0.733 0.510 1.053 APOE-HDL-C升高 -0.372 0.176 4.467 0.035 0.689 0.488 0.973 Gensini评分升高 0.355 0.169 4.412 0.036 1.426 1.024 1.986 -
[1] 杨利娇, 王虹, 韩婷婷, 等. 急性冠状动脉综合征患者的临床特征及预后因素分析[J]. 重庆医学, 2018, 47(10): 67-72. https://www.cnki.com.cn/Article/CJFDTOTAL-CQYX201810017.htm
[2] Nicholls SJ, Puri R, Ballantyne CM, et al. Effect of infusion of high-density lipoprotein mimetic containing recombinant apolipoprotein AI Milano on coronary disease in patients with an acute coronary syndrome in the MILANO-PILOT trial: a randomized clinical trial[J]. JAMA Cardio, 2018, 3(9): 806-814. doi: 10.1001/jamacardio.2018.2112
[3] 齐玥, 刘静, 王淼, 等. 携带载脂蛋白E的HDL-C与冠心病发病风险的前瞻性队列研究[J]. 中华流行病学杂志, 2021, 42(2): 297-302. doi: 10.3760/cma.j.cn112338-20200310-00302
[4] 苏广胜, 付茜, 庞文跃. 载脂蛋白B/载脂蛋白A1比值与青年冠心病患者冠状动脉病变严重程度的研究[J]. 临床心血管病杂志, 2021, 37(7): 663-667. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202107014.htm
[5] Qi Y, Liu J, Wang W, et al. Apolipoprotein E-containing high-density lipoprotein(HDL)modifies the impact of cholesterol-overloaded HDL on incident coronary heart disease risk: A community-based cohort study[J]. J Clin Lipidol, 2018, 12(1): 89-98. doi: 10.1016/j.jacl.2017.11.003
[6] 中华医学会心血管病学分会介入心脏病学组, 中国医师协会心血管内科医师分会血栓防治专业委员会, 中华心血管病杂志编辑委员会. 中国经皮冠状动脉介入治疗指南(2016)[J]. 中华心血管病杂志, 2016, 44(5): 382-400. doi: 10.3760/cma.j.issn.0253-3758.2016.05.006
[7] Valanti E K, Dalakoura-Karagkouni K, Sanoudou D. Current and emerging reconstituted HDL-apoA-I and HDL-apoE approaches to treat atherosclerosis[J]. J Pers Med, 2018, 8(4): 34-37. doi: 10.3390/jpm8040034
[8] 郭宏毅, 李志勇, 闫杰松. 高龄急性冠状动脉综合征患者临床特征及介入治疗预后分析[J]. 解放军医药杂志, 2017, 29(3): 53-56. doi: 10.3969/j.issn.2095-140X.2017.03.014
[9] 郝岩, 潘洋, 高洪瑞, 等. 术前血清脂蛋白a和低密度脂蛋白胆固醇预测急性冠状动脉综合征患者PCI术后短期不良预后价值的比较[J]. 临床心血管病杂志, 2020, 36(12): 1115-1119. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202012010.htm
[10] Tan Y, Ou H, Zhang M, et al. Tanshinone IIA promotes macrophage cholesterol efflux and attenuates atherosclerosis of apoE-/-mice by omentin-1/ABCA1 pathway[J]. Curr Pharm Biotechno, 2019, 20(5): 422-432. doi: 10.2174/1389201020666190404125213
[11] Yu DR, Wang T, Huang J, et al. MicroRNA-9 overexpression suppresses vulnerable atherosclerotic plaque and enhances vascular remodeling through negative regulation of the p38MAPK pathway via OLR1 in acute coronary syndrome[J]. J Cell Biochem, 2020, 121(1): 49-62. doi: 10.1002/jcb.27830
[12] Song QQ, NIN JP, Zhang SY, et al. Effects of simulated heat wave and ozone on high fat diet ApoE deficient mice[J]. Biomed Environ Sci, 2018, 31(10): 757-768.
[13] Lincoff AM, Nicholls SJ, Riesmeyer JS, et al. Evacetrapib and cardiovascular outcomes in high-risk vascular disease[J]. N Engl J Med, 2017, 376(20): 1933-1942. doi: 10.1056/NEJMoa1609581
[14] Nicholls SJ, Schwartz GG, Buhr KA, et al. Apabetalone and hospitalization for heart failure in patients following an acute coronary syndrome: a prespecified analysis of the BET on MACE study[J]. Cardiovasc Diabetol, 2021, 20(1): 1-9. doi: 10.1186/s12933-020-01183-5
[15] Li L, Shi M, Salerno S, et al. Microbial and metabolomic remodeling by a formula of Sichuan dark tea improves hyperlipidemia in apoE-deficient mice[J]. Plos one, 2019, 14(7): 219010-219014.
[16] Garcia C, Montee N, Faccini J, et al. Acute coronary syndrome remodels the antiplatelet aggregation properties of HDL particle subclasses[J]. J Thromb Haemost, 2018, 16(5): 933-945. doi: 10.1111/jth.14003
[17] Low-Kam C, Rhainds D, Lo K S, et al. Variants at the APOE/C1/C2/C4 locus modulate cholesterol efflux capacity independently of high-density lipoprotein cholesterol[J]. J Am Heart Assoc, 2018, 7(16): 9545-9549.
[18] Moriarty PM, Varvel SA, Gordts PLSM, et al. Lipoprotein(a)mass levels increase significantly according to APOE genotype: an analysis of 431 239 patients[J]. Arterioscl Throm Vas, 2017, 37(3): 580-588. doi: 10.1161/ATVBAHA.116.308704
[19] Zhu P, Li L, Gao B, et al. Impact of chronic methamphetamine treatment on the atherosclerosis formation in ApoE-/- mice fed a high cholesterol diet[J]. Oncotarget, 2017, 8(33): 55064-55069. doi: 10.18632/oncotarget.19020
[20] Horiuchi Y, Ohkawa R, Lai SJ, et al. Characterization of the cholesterol efflux of apolipoprotein E-containing highdensity lipoprotein in thp-1 cells[J]. Biol Chem, 2019, 400(2): 209-218. doi: 10.1515/hsz-2018-0284
-




 下载:
下载: