Prediction effect of left ventricular-arterial coupling on stroke volume response to norepinephrine in patients with septic shock
-
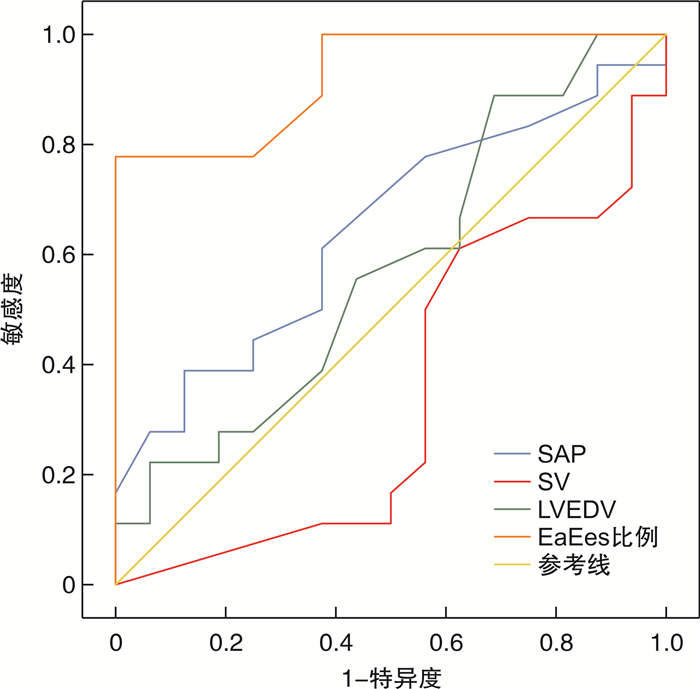
摘要: 目的 探讨左心室-动脉耦合对感染性休克患者去甲肾上腺素(NE)影响每博输出量(SV)的预测效果。方法 选取我院于2019年7月—2021年7月期间在ICU明确诊断为感染性休克的患者。依据NE输注后SV的变化程度将患者分为两组,NE致SV增加≥15%认定为SV反应者,纳入SV反应组(S组);NE致SV增加 < 15%认定为SV无反应者,纳入SV无反应组(N组)。最终S组、N组分别纳入18例、16例患者。记录NE用药剂量、尿量、NE输注至MAP稳定所需时间及累积液体输注量,所有患者均实施经胸超声心动图并记录相关指标。使用logistic回归分析筛选NE导致SV增加的潜在预测因子。绘制Ea/Ees比值、SAP、SV和左室舒张末期容积(LVEDV)的ROC曲线,并计算曲线下面积(AUC)。依据ROC曲线计算Ea/Ees比值、SAP、SV和LVEDV最大约登指数对应的敏感度及特异度。结果 两组患者NE输注至MAP稳定时间的比较差异无统计学意义(P>0.05)。两组患者NE使用剂量和研究期间尿量的比较,差异无统计学意义(P>0.05)。S组NE输注前LVESV值和Ea/Ees比值明显高于N组,Ees则明显低于N组,差异有统计学意义(P< 0.05)。S组NE输注后DAP明显高于N组,Ees则明显低于N组,差异有统计学意义(P< 0.05)。S组NE输注后左室收缩末期容积(LVESV)、Ea/Ees明显低于NE输注前,差异有统计学意义(P< 0.05)。N组NE输注后SAP、DAP、Ea、Ees明显高于NE输注前,差异有统计学意义(P< 0.05)。Logistic回归分析结果显示HR、SAP、VTI、SV和LVEDV与SV对NE的反应无明显相关性(P>0.05)。Ea/Ees则与SV对NE的反应存在明显相关性(P< 0.05)。LVEDV、SAP、SV的AUC均 < 0.7,Ea/Ees的AUC为0.924。Ea/Ees的最大约登指数为0.701,对应敏感度为77.8%,特异度为100.0%。结论 输注NE可引起感染性休克患者Ea和Ees的变化,左心室-动脉耦合对感染性休克患者输注NE后SV反应具有预测价值。Abstract: Objective Todiscuss the prediction effect of left ventricular-arterial coupling on stroke volume(SV)response to norepinephrine(NE)in patients with septic shock.Methods Patients diagnosed with septic shock in ICU of our hospital from July 2019 to July 2021 were selected. They were divided into two groups according to the SV change after NE infusion. Patients with≥15% increase in SV caused by NE were identified as SV responsor and included in SV responder group(S group). Patients with < 15% increase in SV caused by NE were identified as non-responder to SV and included in the SV non-responder group(N group). Finally, 18 and 16 patients were included in group S and group N, respectively. NE dose, urine volume, time required for NE infusion to MAP stabilization and cumulative fluid infusion volume were recorded. Transthoracic echocardiography was performed for all patients and related indicators were recorded. Logistic regression analysis was used to screen for potential predictors of the increase in SV due to NE. The ROC curves of Ea/Ees ratio, SAP, SV and LVEDV were drawn, and the AUC was calculated. The sensitivity and specificity of Ea/Ees ratio, SAP, SV and LVEDV were calculated according to ROC curve.Results There was no statistical significance in the time from NE infusion to MAP stabilization between 2 groups(P>0.05). There was no significant difference in NE dose and urine volume between 2 groups(P>0.05). Before NE infusion, the LVESV value and Ea/Ees ratio of group S were significantly higher than those of group N, while Ees was significantly lower than that of group N, with statistical significance(P< 0.05). After NE infusion, DAP in group S was significantly higher than that in group N, and Ees was significantly lower than that in group N, with statistical significance(P< 0.05). The LVESV and Ea/Ees of group S after NE infusion were significantly lower than those before NE infusion, and the difference was statistically significant(P< 0.05). SAP, DAP, Ea and Ees of group N after NE infusion were significantly higher than those before NE infusion, with statistical significance(P< 0.05). Logistic regression analysis showed that HR, SAP, VTI, SV and LVEDV had no significant correlation with SV response to NE(P< 0.05). Ea/Ees was significantly correlated with the reaction of SV to NE(P< 0.05). The AUC of LVEDV, SAP and SV were all < 0.7, and the AUC of Ea/Ees was 0.924. The maximum Youden index of Ea/Ees was 0.701, the corresponding sensitivity was 77.8%, and the specificity was 100%.Conclusion NE infusion can cause changes of Ea and Ees in patients with septic shock and left ventricular-arterial coupling has predictive value for SV response in patients with septic shock after NE infusion.
-
Key words:
- left ventricular-arterial coupling /
- septic shock /
- norepinephrine /
- stroke volume
-

-
表 1 两组患者一般情况的比较
X±S,例(%) 一般情况 S组
(18例)N组
(16例)t P 年龄/岁 70.4±8.6 71.5±10.3 0.339 0.737 性别/例 男 12(66.7) 13(81.3) 0.448 女 6(33.3) 3(18.8) BMI 22.3±2.8 22.6±3.0 0.302 0.765 APACHE Ⅱ评分/分 20±5 21±6 0.530 0.600 SOFA评分/分 8±2 9±2 1.455 0.155 感染部位 肺 9(50.0) 8(50.0) 1.000 腹部 5(27.8) 5(31.3) 1.000 尿路 3(16.7) 2(12.5) 1.000 其他 1(5.56) 1(6.25) 1.000 合并症 高血压 8(44.4) 8(50.0) 1.000 糖尿病 8(44.4) 7(43.8) 1.000 慢性阻塞性肺疾病(COPD) 4(22.2) 4(25.0) 1.000 冠心病 1(5.56) 2(12.5) 1.000 慢性肾病 1(5.56) 1(6.25) 1.000 IMV治疗 13(72.2) 11(68.8) 1.000 PaO2/FiO2 257±106 285±147 0.642 0.525 PEEP/cmH2Oa) 5±1 5±1 潮气量/(mL·kg-1) 6.9±1.1 7.1±1.3 0.486 0.630 丙泊酚 9(50.0) 7(43.8) 0.744 咪达唑仑 10(55.6) 8(43.8) 1.000 芬太尼 8(44.4) 7(43.8) 1.000 血乳酸/(mmol·L-1) 2.8±1.4 3.1±1.7 0.564 0.577 NE输注至MAP稳定时间/min 88±41 99±53 0.681 0.501 液体输注量/mL NE输注前 1533±569 1716±618 0.899 0.375 研究期间 186±97 212±105 0.751 0.458 确诊24 h内 3853±1084 4039±1216 0.472 0.640 NE剂量/(μg·kg-1·min-1) 0.23±0.14 0.33± 0.22 1.600 0.120 尿量/(mL·kg-1·h-1) 1.18±0.56 1.34± 0.85 0.655 0.517 注:a)1 cmH2O=0.098 kPa。 表 2 输注NE对两组患者心血管的影响
X±S 指标 S组(18例) N组(16例) t1/t2 P1/P2 NE输注前 NE输注后 NE输注前 NE输注后 HR/(次·min-1) 109±14 107±15 107±11 99±14 0.459/1.601 0.649/0.119 SAP/mmHg 87±6 112±151) 85±4 108±121) 1.128/0.851 0.268/0.401 DAP/mmHg 49±5 63±71) 46±5 54±61) 1.746/3.999 0.090/ < 0.001 CVP/mmHg 8±3 9±3 8±4 9±4 VTI/cm 16.9±2.9 19.2±3.11) 19.0±3.4 20.6±3.8 1.944/1.182 0.061/0.246 SV/mL 46±7 56±91) 51±8 56±11 1.944/- 0.061/- LVEDV/mL 102±12 105±10 99±11 104±9 0.757/0.305 0.455/0.762 LVESV/mL 53±6 48±71) 44±9 44±7 3.467/1.633 0.002/0.106 LVEF/% 47±5 53±61) 49±6 52±7 1.060/0.449 0.297/0.657 CI/(L·min-1·m-2) 3.4±1.0 3.7±1.2 3.5±1.1 3.6±1.4 0.278/0.224 0.783/0.824 Tpre-e/ms 61±13 58±16 55±15 54±17 1.250/0.707 0.221/0.485 Ttot-s/ms 220±52 259±49 236±54 262±50 0.880/0.177 0.386/0.861 Ea/(mmHg·mL-1) 1.61±0.34 1.79±0.38 1.47±0.30 1.82±0.391) 1.266/0.227 0.215/0.822 Ees/(mmHg·mL-1) 1.14±0.22 1.44±0.391) 1.48±0.42 1.81±0.461) 3.006/2.538 0.005/0.016 Ea/Ees 1.42±0.19 1.24±0.321) 1.02±0.20 1.07±0.31 5.978/1.569 < 0.001/0.127 与同组NE输注前相比,1)P < 0.05;P1:两组间NE输注前相比;P2:两组间NE输注后相比。 表 3 SV对NE反应预测因素的logistic回归分析
危险因素 B SE Wald P OR(95%CI) HR -0.122 0.089 1.877 0.171 0.886(0.744~1.054) SAP 0.002 0.134 0.000 0.988 1.002(0.770~1.303) VTI 0.542 0.324 2.797 0.094 1.719(0.911~3.245) SV 0.196 0.133 2.174 0.140 1.216(0.938~1.578) LVEDV 0.145 0.109 1.756 0.185 1.156(0.933~1.432) Ea/Ees -15.705 7.787 4.067 0.044 0(0~0.643) 表 4 各指标的AUC及敏感度、特异度的比较
项目 AUC 约登指数 敏感度
/%特异度/% 95%CI Ea/Ees 0.924 0.701 77.8 100.0 0.838~1.000 LVEDV 0.578 0.379 88.9 31.2 0.383~0.774 SAP 0.646 0.264 38.9 87.5 0.459~0.832 SV 0.344 -0.014 61.1 37.5 0.153~0.534 -
[1] Vincent JL, Jones G, David S, et al. Frequency and mortality of septic shock in Europe and North America: a systematic review and meta-analysis[J]. Crit Care, 2019, 23(1): 196. doi: 10.1186/s13054-019-2478-6
[2] Levy MM, Evans LE, Rhodes A. The Surviving Sepsis Campaign Bundle: 2018 update[J]. Intensive Care Med, 2018, 44(6): 925-928. doi: 10.1007/s00134-018-5085-0
[3] Scheeren T, Bakker J, De Backer D, et al. Current use of vasopressors in septic shock[J]. Ann Intensive Care, 2019, 9(1): 20. doi: 10.1186/s13613-019-0498-7
[4] Hamzaoui O, Shi R. Early norepinephrine use in septic shock[J]. J Thorac Dis, 2020, 12(Suppl 1): S72-S77.
[5] Rhodes A, Evans LE, Alhazzani W, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016[J]. Intensive Care Med, 2017, 43(3): 304-377. doi: 10.1007/s00134-017-4683-6
[6] Guarracino F, Baldassarri R, Pinsky MR. Ventriculo-arterial decoupling in acutely altered hemodynamic states[J]. Crit Care, 2013, 17(2): 213. doi: 10.1186/cc12522
[7] Hsu S, Simpson CE, Houston BA, et al. Multi-Beat Right Ventricular-Arterial Coupling Predicts Clinical Worsening in Pulmonary Arterial Hypertension[J]. J Am Heart Assoc, 2020, 9(10): e016031. doi: 10.1161/JAHA.119.016031
[8] Little WC, Pu M. Left ventricular-arterial coupling[J]. J Am Soc Echocardiogr, 2009, 22(11): 1246-1248. doi: 10.1016/j.echo.2009.09.023
[9] Chirinos JA. Ventricular-arterial coupling: Invasive and non-invasive assessment[J]. Artery Res, 2013, 7(1): 10.
[10] Yan J, Zhou X, Hu B, et al. Prognostic value of left ventricular-arterial coupling in elderly patients with septic shock[J]. J Crit Care, 2017, 42: 289-293. doi: 10.1016/j.jcrc.2017.08.017
[11] Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock(Sepsis-3)[J]. JAMA, 2016, 315(8): 801-810. doi: 10.1001/jama.2016.0287
[12] Chen CH, Fetics B, Nevo E, et al. Noninvasive single-beat determination of left ventricular end-systolic elastance in humans[J]. J Am Coll Cardiol, 2001, 38(7): 2028-2034. doi: 10.1016/S0735-1097(01)01651-5
[13] 付婧, 燕宪亮, 许铁. 乌司他丁通过抑制炎症反应及激活Nrf2/ARE通路提高感染性休克患者临床疗效的研究[J]. 临床急诊杂志, 2020, 21(2): 161-164. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202002014.htm
[14] Lipcsey M, Castegren M, Bellomo R. Hemodynamic management of septic shock[J]. Minerva Anestesiol, 2015, 81(11): 1262-1272.
[15] 龚蕊, 邵娟, 周胜亮, 等. 去甲肾上腺素在感染性休克中应用的新进展[J]. 江西医药, 2015, 50(10): 1132-1135. doi: 10.3969/j.issn.1006-2238.2015.10.069
[16] 中华医学会重症医学分会. 中国严重脓毒症/脓毒性休克治疗指南(2014)[J]. 中华内科杂志, 2015, 54(6): 557-581. https://www.cnki.com.cn/Article/CJFDTOTAL-QKYL201504002.htm
[17] 方奕鹏, 张会娟, 郭喆, 等. 急诊成人脓毒症防治的新认识——美国急诊医师协会"急诊科与院前成人疑似脓毒症患者早期诊疗共识"解析[J]. 临床急诊杂志, 2021, 22(5): 361-368. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202105016.htm
[18] Espinoza EDV, Hernandez G, Bakker J. Norepinephrine, more than a vasopressor[J]. Ann Transl Med, 2019, 7(Suppl 1): S25.
[19] Persichini R, Silva S, Teboul JL, et al. Effects of norepinephrine on mean systemic pressure and venous return in human septic shock[J]. Crit Care Med, 2012, 40(12): 3146-3153. doi: 10.1097/CCM.0b013e318260c6c3
[20] Guarracino F, Ferro B, Morelli A, et al. Ventriculoarterial decoupling in human septic shock[J]. Crit Care, 2014, 18(2): R80. doi: 10.1186/cc13842
[21] Little WC, Cheng CP. Left ventricular-arterial coupling in conscious dogs[J]. Am J Physiol, 1991, 261(1 Pt 2): H70-76. https://pubmed.ncbi.nlm.nih.gov/1858932/
[22] Kelly RP, Ting CT, Yang TM, et al. Effective arterial elastance as index of arterial vascular load in humans[J]. Circulation, 1992, 86(2): 513-521. doi: 10.1161/01.CIR.86.2.513
[23] Monge García MI, Santos A. Understanding ventriculo-arterial coupling[J]. Ann Transl Med, 2020, 8(12): 795. doi: 10.21037/atm.2020.04.10
-




 下载:
下载: