The value of systemic immune inflammation index in predicting in-hospital major adverse cardiovascular events after direct percutaneous coronary intervention in patients with acute myocardial infarction
-
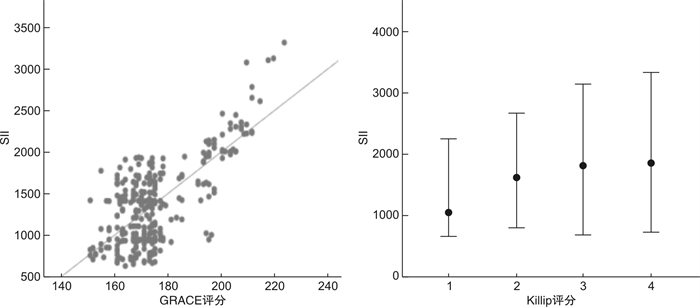
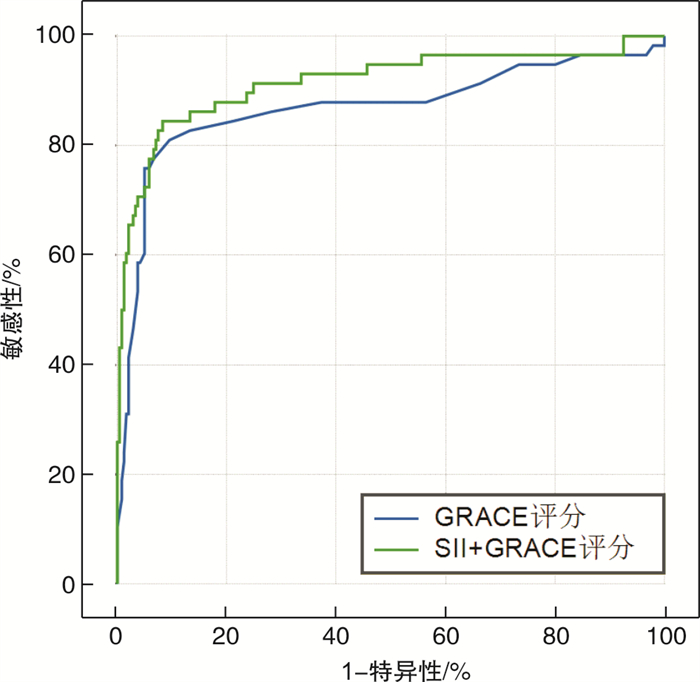
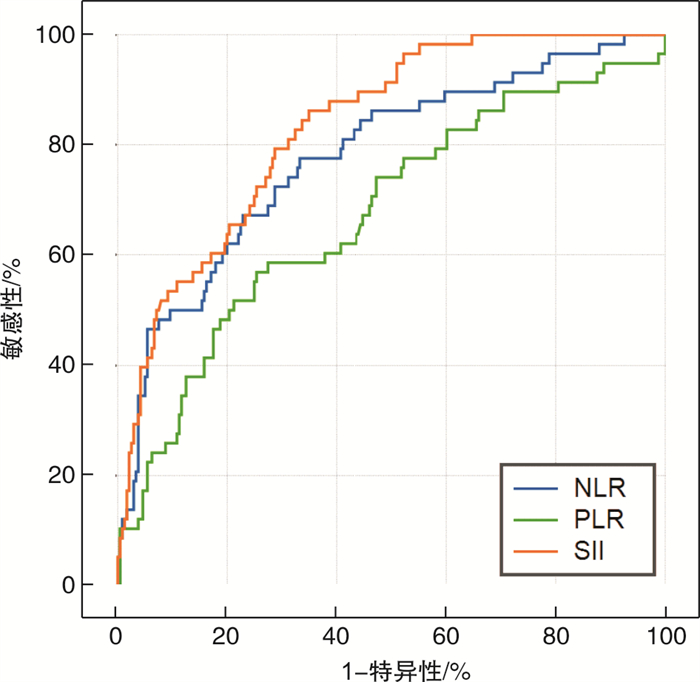
摘要: 目的 探讨全身免疫炎症指数(SII)对接受直接经皮冠状动脉介入治疗(PCI)的急性心肌梗死(AMI)患者发生院内主要不良心血管事件(MACE)的预测价值。方法 连续纳入2019年9月-2020年4月就诊于徐州医科大学附属医院急诊科,并接受直接PCI治疗的AMI患者,共计298例,回顾性分析患者的一般资料、临床表现、实验室数据、心电图及影像学资料等,由入室的血常规计算SII、中性粒细胞与淋巴细胞比值(NLR)、血小板与淋巴细胞比值(PLR)数值,根据住院期间是否发生MACE分为MACE组(n=58)与非MACE组(n=240),比较2组的临床资料,行单因素及多因素回归分析,分析MACE的危险因素,探讨SII与MACE的相关性,并绘制受试者工作特征(ROC)曲线,评估SII、NLR、PLR对AMI患者院内MACE的预测价值,根据最大约登指数确定SII的最佳临界值,并将SII联合急性冠脉事件全球注册(GRACE)评分,评价是否能增加GRACE评分预测AMI患者院内MACE的效能。结果 与非MACE组相比,MACE组SII、NLR及PLR显著升高(P< 0.05);多因素回归分析显示,SII是AMI后发生MACE的独立危险因素; ROC曲线表明,3种炎症指标对患者院内MACE的发生均有一定的预测价值,其中SII曲线下面积(AUC)为0.829(P< 0.05,95%CI0.776~0.882),显著高于NLR及PLR,表明SII预测效能最大,将SII联合GRACE评分后,AUC由原来的0.870(P< 0.05,95%CI0.803~0.882)增加至0.906(P< 0.05,95%CI0.851~0.936)。结论 入室SII与AMI患者的预后相关,能够更高效地识别高危患者,联合GRACE评分后,能够提升GRACE评分对AMI患者发生MACE的预测价值。
-
关键词:
- 全身免疫炎症指数 /
- 经皮冠状动脉介入治疗术 /
- 急性心肌梗死 /
- 主要不良心血管事件
Abstract: Objective To investigate the relationship between systemic immune inflammation index(SII) and in-hospital major adverse cardiovascular events(MACE) in patients with acute myocardial infarction(AMI) who received direct percutaneous coronary intervention(PCI).Methods A total of 298 patients with acute myocardial infarction were enrolled in the Emergency Department of the affiliated Hospital of Xuzhou Medical University from September 2019 to April 2020 and received direct PCI treatment.The general data, clinical manifestations, laboratory data, electrocardiogram and imaging data of the patients were analyzed retrospectively. The values of SII, neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) were calculated from the blood routine examination. According to the adverse events occurred during hospitalization, the patients were divided into two groups: MACE group(n=58) and non-MACE group(n=240). The clinical data of the two groups were compared and analyzed by univariate and multivariate regression analysis to analyze the risk factors of adverse events, to explore the correlation between SII and adverse events, and to draw the receiver operating characteristic(ROC) curve to evaluate the predictive value of SII, NLR and PLR in hospital MACE in patients with myocardial infarction.The best critical value of SII was determined according to the most approximate index, and SII was combined with Global Registration of Acute Coronary events(GRACE) score to evaluate whether the efficiency to predict the in-hospital MACE in patients with acute myocardial infarction can be increased.Results SII, NLR and PLR in MACE group were significantly higher than those in non-MACE group.Multivariate regression analysis showed that SII was an independent risk factor for adverse events after myocardial infarction. ROC curve showed that the three inflammatory indexes had certain predictive value for the occurrence of MACE in hospital, of which the area under SII curve(area under curve, AUC) was 0.829(P< 0.05, 95%CI0.776-0.882), which was significantly higher than that of NLR and PLR. It shows that the prediction efficiency of SII was the best. After the SII combined with GRACE score, the AUC is increased from 0.870(P< 0.05, 95%CI0.803-0.882) to 0.906(P< 0.05, 95%CI0.851-0.936).Conclusion Admission SII is related to the prognosis of patients with AMI, and can more efficiently identify high-risk patients.When SII was combined with GRACE score, the predictive value of GRACE score for MACE in patients with AMI was improved. -

-
表 1 非MACE组与MACE组患者临床资料比较
例(%),X±S 临床资料 MACE组(n=58) 非MACE组(n=240) P 年龄/岁 68.0±12.6 61.8±13.1 0.001 男性 38(65.5) 200(83.3) 0.003 BMI 25.0±3.9 25.5±3.9 0.350 高血压 30(51.7) 110(45.8) 0.410 糖尿病 16(27.6) 50(20.8) 0.260 血脂异常 20(34.5) 98(40.8) 0.690 SII 1894.7±500.4 1299.3±567.9 < 0.001 NLR 9.5±3.9 6.3±3.5 0.001 PLR 226.3±105.1 178.7±101.1 0.002 C反应蛋白/(mg·L-1) 9.4±4.3 7.2±2.1 0.190 NT-proBNP/(pg·mL-1) 1764.7±296.6 723.4±156.7 0.020 血红蛋白/(g·L-1) 133.5±14.9 142.7±20.8 0.004 血肌酐/(μmol·L-1) 107.7±40.1 69.8±39.5 0.071 白蛋白/(g·L-1) 39.0±4.1 41.0±4.9 0.620 总胆固醇/(mmol·L-1) 9.9±5.2 4.4±1.0 0.040 三酰甘油/(mmol·L-1) 1.4±0.8 1.6±1.4 0.241 LDL/(mmol·L-1) 2.8±0.9 28.0±0.9 0.922 HDL/(mmol·L-1) 1.0±0.3 1.5±0.3 0.660 ds-LDL/(mmol·L-1) 0.6±0.2 0.9±0.1 0.550 脂蛋白a/(mg·L-1) 289.8±162.3 297.0±158.3 0.901 总胆红素/(μmol·L-1) 10.7±5.4 13.2±6.5 0.312 尿酸/(μmol·L-1) 335.9±113.6 313.6±170.7 0.231 hs-TNT峰值/(ng·L-1) 4986.0±2659.6 3465.2±3292.7 0.005 肌酸激酶同工酶峰值/(ng·mL-1) 175.8±92.6 130.9±50.2 0.110 STEMI 53(91.4) 192(80.0) 0.042 Killip分级Ⅱ~Ⅳ级 34(58.6) 33(13.7) < 0.001 多支病变或左主干病变 46(79.3) 177(73.7) 0.453 GRACE评分/分 192.2±15.4 171.5±8.4 < 0.001 表 2 MACE发生的单因素和多因素Logisitic回归分析
相关因素 单因素分析 多因素分析 OR(95%CI) P OR(95%CI) P 年龄 1.039(1.015~1.065) 0.002 1.022(0.985~1.061) 0.252 SII 1.002(1.001~1.003) < 0.001 1.002(1.001~1.004) 0.004 NLR 1.292(1.173~1.424) 0.001 1.312(1.201~1.422) 0.038 PLR 1.001(1.001~1.008) 0.012 1.001(1.001~1.004) 0.042 血红蛋白 0.983(0.971~0.996) 0.009 0.987(0.968~1.007) 0.202 总胆固醇 1.027(0.910~1.158) 0.671 STEMI 2.705(1.026~7.130) 0.042 3.184(0.716~14.162) 0.131 Killip分级Ⅱ~Ⅳ级 8.929(4.712~16.912) < 0.001 4.125(1.628~10.454) 0.003 GRACE评分 1.139(1.104~1.175) < 0.001 1.128(1.088~1.168) < 0.001 表 3 SII与患者MACE的关系
例(%),X±S 相关因素 SII < 1513.8(n=186) SII>1513.8(n=112) P 年龄/岁 61.6±13.0 65.4±13.2 0.021 男性 154(82.8) 84(75.0) 0.172 高血压 88(47.3) 52(46.4) 0.921 糖尿病 39(21.0) 27(24.1) 0.512 NT-proBNP/(pg·mL-1) 752.3±149.0 1221.7±217.1 0.810 GRACE评分/分 172.9±14.2 180.0±14.7 0.001 Killip分级Ⅱ~Ⅳ级 30(16.1) 37(33.0) 0.002 多支病变或左主干病变 133(71.5) 90(80.4) 0.041 MACE 14(7.5) 44(39.3) 0.001 死亡 5(2.7) 17(15.2) 0.001 心源性休克 11(5.9) 30(26.8) 0.001 入院前停搏 3(1.6) 2(1.8) 0.910 心室颤动 6(3.2) 8(7.1) 0.110 急性心力衰竭 14(7.5) 46(41.1) 0.001 房室传导阻滞 3(3.2) 3(2.7) 0.211 -
[1] Guclu K, Celik M. Prognostic Value of Inflammation Parameters in Patients With Non-ST Elevation Acute Coronary Syndromes[J]. Angiology, 2020, 71(9): 825-830. doi: 10.1177/0003319720936500
[2] 中华医学会心血管病学分会, 中华心血管病杂志编辑委员会. 急性ST段抬高型心肌梗死诊断和治疗指南(2019)[J]. 中华心血管病杂志, 2019, 47(10): 766-783. https://www.cnki.com.cn/Article/CJFDTOTAL-GWXX201504001.htm
[3] Esenbo a K, Kurtul A, Yamantürk YY, et al. Systemic immune-inflammation index predicts no-reflow phenomenon after primary percutaneous coronary intervCandemir M, Kiziltun E, Nurko S, ahinarslan A. Relationship Between ention[J]. Acta Cardiol, 2021, 1-8.
[4] 冯彩玲, 李利军, 李正卿, 等. 血小板/淋巴细胞计数比值对急性心肌梗死后发生心力衰竭的预测价值[J]. 检验医学与临床, 2019, 16(18): 2666-2669. doi: 10.3969/j.issn.1672-9455.2019.18.023
[5] Liu Y, Ye T, Chen L, et al. Systemic immune-inflammation index predicts the severity of coronary stenosis in patients with coronary heart disease[J]. Coron Artery Dis, 2021, 32(8): 715-720. doi: 10.1097/MCA.0000000000001037
[6] 陈鑫森, 邵萌, 张天, 等. 血液学参数预测急性ST段抬高型心肌梗死患者经皮冠状动脉介入治疗术后发生主要不良心血管事件的价值研究[J]. 中国全科医学, 2020, 23(27): 3389-3395. doi: 10.12114/j.issn.1007-9572.2020.00.245
[7] Chang LS, Lin YJ, Yan JH, et al. Neutrophil-to-lymphocyte ratio and scoring system for predicting coronary artery lesions of Kawasaki disease[J]. BMC Pediatr, 2020, 20(1): 398. doi: 10.1186/s12887-020-02285-5
[8] Agarwal R, Aurora RG, Siswanto BB, et al. The prognostic value of neutrophil-to-lymphocyte ratio across all stages of coronary artery disease[J]. Coron Artery Dis, 2022, 33(2): 137-143. doi: 10.1097/MCA.0000000000001040
[9] Serrano CV Jr, de Mattos FR, Pitta FG, et al. Association between Neutrophil-Lymphocyte and Platelet-Lymphocyte Ratios and Coronary Artery Calcification Score among Asymptomatic Patients: Data from a Cross-Sectional Study[J]. Mediators Inflamm, 2019, 2019: 6513847. http://downloads.hindawi.com/journals/mi/2019/6513847.pdf
[10] Zhao L, Xu T, Li Y, et al. Variability in blood lipids affects the neutrophil to lymphocyte ratio in patients undergoing elective percutaneous coronary intervention: a retrospective study[J]. Lipids Health Dis, 2020, 19(1): 124. doi: 10.1186/s12944-020-01304-9
[11] Walzik D, Joisten N, Zacher J, et al. Transferring clinically established immune inflammation markers into exercise physiology: focus on neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio and systemic immune-inflammation index[J]. Eur J Appl Physiol, 2021, 121(7): 1803-1814. doi: 10.1007/s00421-021-04668-7
[12] Park JS, Seo KW, Choi BJ, et al. Importance of prognostic value of neutrophil to lymphocyte ratio in patients with ST-elevation myocardial infarction[J]. Medicine(Baltimore), 2018, 97(48): e13471.
[13] Zahorec R. Neutrophil-to-lymphocyte ratio, past, present and future perspectives[J]. Bratisl Lek Listy, 2021, 122(7): 474-488.
[14] Candemir M, Kiziltun E, Nurko S, et al. Relationship Between Systemic Immune-Inflammation Index (SⅡ) and the Severity of Stable Coronary Artery Disease[J]. Angiology, 2021, 72(6): 575-581. doi: 10.1177/0003319720987743
[15] Yang YL, Wu CH, Hsu PF, et al. Systemic immune-inflammation index(SⅡ)predicted clinical outcome in patients with coronary artery disease[J]. Eur J Clin Invest, 2020, 50(5): e13230.
[16] Lee Y, Baradi A, Peverelle M, et al. Usefulness of Platelet-to-Lymphocyte Ratio to Predict Long-Term All-Cause Mortality in Patients at High Risk of Coronary Artery Disease Who Underwent Coronary Angiography[J]. Am J Cardiol, 2018, 121(9): 1021-1026. doi: 10.1016/j.amjcard.2018.01.018
[17] Xu M, Chen R, Liu L, et al. Systemic immune-inflammation index and incident cardiovascular diseases among middle-aged and elderly Chinese adults: The Dongfeng-Tongji cohort study[J]. Atherosclerosis, 2021, 323(1): 20-29.
[18] Choi DH, Kobayashi Y, Nishi T, et al. Combination of Mean Platelet Volume and Neutrophil to Lymphocyte Ratio Predicts Long-Term Major Adverse Cardiovascular Events After Percutaneous Coronary Intervention[J]. Angiology, 2019, 70(4): 345-351. doi: 10.1177/0003319718768658
[19] Wada H, Dohi T, Miyauchi K, et al. Neutrophil to Lymphocyte Ratio and Long-Term Cardiovascular Outcomes in Coronary Artery Disease Patients with Low High-Sensitivity C-Reactive Protein Level[J]. Int Heart J, 2020, 61(3): 447-453. doi: 10.1536/ihj.19-543
[20] Boralkar KA, Kobayashi Y, Amsallem M, et al. Value of Neutrophil to Lymphocyte Ratio and Its Trajectory in Patients Hospitalized With Acute Heart Failure and Preserved Ejection Fraction[J]. Am J Cardiol, 2020, 125(2): 229-235. doi: 10.1016/j.amjcard.2019.10.020
[21] 徐晓婷, 张强, 杨丽红, 等. 中性粒细胞与淋巴细胞比值联合全球急性冠状动脉事件注册研究评分与急性冠脉综合征患者预后的相关性分析[J]. 中国全科医学, 2019, 22(11): 1302-1306. doi: 10.12114/j.issn.1007-9572.2018.00.260
-




 下载:
下载: