Risk factors of conversion from laparoscopic cholecystectomy to laparotomy for acute calculous cholecystitis base on multivariate logistic regression analysis(a multicenter retrospective study)
-
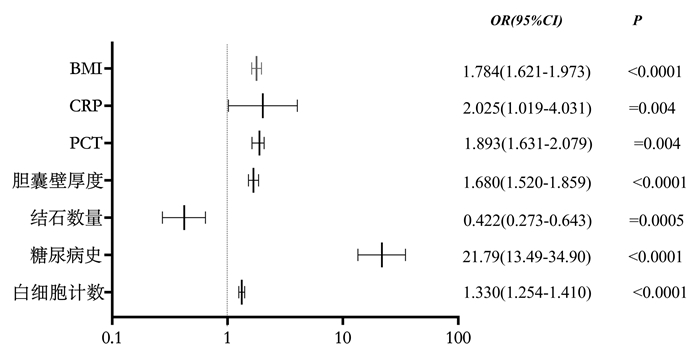
摘要: 目的 探讨急性结石性胆囊炎行腹腔镜胆囊切除术过程中转开腹的影响因素。方法 回顾性分析3191例急性结石性胆囊炎行腹腔镜胆囊切除术患者的临床资料,按术中是否中转开腹胆囊切除术分为中转组和非中转组,通过多元回归模式对患者性别、年龄、BMI、既往病史(糖尿病病史、高血压病史及既往腹部外科手术史)、术前实验室检查(WBC、PCT、CRP及INR)、术前胆囊B超特征(胆囊结石数量、胆囊壁厚度)及手术时间等因素进行统计学分析。结果 资料数据经多元logistic回归分析显示,BMI、糖尿病病史、术前白细胞计数、PCT、CRP、结石数量、胆囊壁厚度是影响急性结石性胆囊炎患者行腹腔镜胆囊切除中转开腹的因素(P< 0.05);BMI(OR=1.784;95%CI:1.621~1.973;P< 0.001)、糖尿病病史(OR=21.79;95%CI:13.49~34.90;P< 0.001)、WBC(OR=1.330;95%CI:1.254~1.410;P< 0.001)、PCT(OR=1.839;95%CI:1.631~2.079;P=0.004)、CRP(OR=2.025;95%CI:1.019~4.031;P=0.004)升高及胆囊壁增厚(OR=1.680;95%CI:1.520~1.859;P< 0.001)为中转开腹的独立危险因素,而结石数量(OR=0.422;95%CI:0.273~0.643;P=0.0005)为中转开腹的保护因素。结论 急性结石性胆囊炎患者实施腹腔镜胆囊切除术时,对BMI超标、术前有糖尿病病史、术前WBC、PCT及CRP较高或B超显示胆囊壁增厚、结石单发的患者,应考虑术中中转开腹手术可能。
-
关键词:
- 急性结石性胆囊炎 /
- 腹腔镜胆囊切除术 /
- 中转开腹手术 /
- 多因素 /
- logistic回归
Abstract: Objective To investigate the risk factors of conversion from laparoscopic cholecystectomy transferring to laparotomy for acute calculous cholecystitis.Methods Three thousand one hundred and ninety one patients with acute calculous cholecystitis who underwent laparoscopic cholecystectomy from Huadu District People's Hospital of Guangzhou, Guangzhou First People's Hospital, Guangzhou Red Cross Hospital, the First Affiliated Hospital/School of Clinical Medicine of Guangdong Pharmaceutical University, Guangzhou Nansha Central Hospital, Qingyuan Municipal People's Hospital, People's Hospital of Qianxi and the Second People's Hospital of Huadu District of Guangzhou were analyzed retrospectively. Base on whether transferred to open cholecystectomy or not during the operation, all of the patients were divided into two groups: Conversion group and laparoscopic cholecystectomy group. And then the factors such as gender, age, BMI, previous medical history(diabetes, hypertension and previous abdominal surgery), preoperative laboratory examination(WBC, PCT, CRP and INR), preoperative gallbladder B-ultrasound characteristics(number of gallstones and thickness of gallbladder wall) were statistically analyzed by multiple logistic regression model.Results Multivariate logistic regression analysis showed that BMI, history of diabetes, preoperative WBC, PCT, CRP, the number of stones and the thickness of gallbladder wall were the factors influencing the conversion from laparoscopic cholecystectomy transferring to laparotomy with acute calculous cholecystitis(P< 0.05); High BMI(OR=1.784; 95%CI: 1.621-1.973;P< 0.001), diabetes history(OR=21.79; 95%CI: 13.49-34.90;P< 0.001), increase of WBC count(OR=1.330; 95%CI: 1.254-1.410;P< 0.001), PCT(OR=1.839; 95%CI: 1.631-2.079;P=0.004) and CRP(OR=2.025; 95%CI: 1.019-4.031;P=0.004) and thickness of gallbladder wall(OR=1.680; 95%CI: 1.520-1.859;P< 0.001) were the independent risk factors for conversion to laparotomy, while the number of calculi(OR=0.422; 95%CI: 0.273-0.643;P=0.0005) was the protective factor for conversion to laparotomy.Conclusion When laparoscopic cholecystectomy is performed in patients with acute calculous cholecystitis, the possibility of conversion to laparotomy should be considered for those patients with High BMI, preoperative diabetes history, preoperative high white blood cell count, high PCT and CRP, or gallbladder wall thickening and solitary stones shown by B-ultrasound. -

-
表 1 ACC患者行LC过程中转开腹手术的单因素分析
例(%),X±S 资料 中转组(90例) 非中转组(3101例) χ2/t P 性别/例 男 22 723 0.306 0.759 女 78 2378 年龄/岁 55.91±14.53 56.84±13.62 1.220 1.785 BMI 28.56±1.7 18.86±2.1 8.874 < 0.001 高血压病史 1.170 2.165 有 6(6.67) 185(5.97) 无 94(93.33) 2916(94.03) 糖尿病史 306.700 < 0.001 有 35(38.89) 88(2.84) 无 55(61.11) 3013(97.16) 腹部手术史 2.280 0.099 有 15(16.67) 475(15.32) 无 75(83.33) 2626(84.68) 实验室结果 WBC/(×109·L-1) 15.72±4.73 12.83±2.62 9.996 < 0.001 PCT/(ng·mL-1) 1.66(0.72~2.61) 0.37(0.09~0.58) -5.530 < 0.001 CRP/(mg·mL-1) 37.33±8.67 13.92±4.41 11.030 < 0.001 INR 1.014±0.02 0.9887±0.03 0.130 1.517 结石数量 17.150 < 0.001 单发 56(62.22) 1254(40.44) 多发 34(37.78) 1847(59.56) 胆囊壁厚度/mm 6.70±1.86 4.67±2.2 11.790 < 0.001 表 2 影响ACC患者LC中转开腹的多因素logistic回归分析
因素 回归系数 Wald χ2 P OR 95%CI BMI 2.078 6.783 < 0.0001 1.784 1.621~1.973 糖尿病史 3.081 5.768 < 0.0001 21.790 13.49~34.900 WBC 0.285 14.284 < 0.0001 1.330 1.254~1.410 PCT 0.609 8.217 0.004 1.893 1.631~2.079 CRP 0.025 8.495 0.004 2.025 1.019~4.031 胆囊壁厚度 1.999 4.762 < 0.0001 1.680 1.520~1.859 结石数量 -0.863 4.744 0.0005 0.422 0.273~0.643 表 3 LC中转开腹各因素预测值、各预测曲线AUC及联合ROC
因素 预测值 标准误 95%CI AUC P BMI 0.08736 0.03524 0.5788~0.7170 0.6479 < 0.0001 白细胞计数 0.09787 0.03934 1.022~1.193 0.7077 < 0.0001 PCT 0.08677 0.1018 0.8867~1.324 0.6891 < 0.0001 CRP 0.008486 0.005171 0.9978~1.018 0.6176 0.0001 糖尿病 1.824 0.3564 3.040~12.32 0.6803 < 0.0001 胆囊壁厚度 0.2440 0.06479 1.123~1.448 0.7325 < 0.0001 结石数量 -0.8035 0.2608 0.2660~0.7424 0.6080 0.0005 联合预测ROC 0.02376 0.5685~0.6616 0.6150 0.0002 -
[1] Brunt LM, Deziel DJ, Telem DA, et al. Safe Cholecystectomy Multi-society Practice Guideline and State of the Art Consensus Conference on Prevention of Bile Duct Injury During Cholecystectomy[J]. Ann Surg, 2020, 272(1): 3-23. doi: 10.1097/SLA.0000000000003791
[2] Mayumi T, Okamoto K, Takada T, et al. Tokyo Guidelines 2018: management bundles for acute cholangitis and cholecystitis[J]. J Hepatobiliary Pancreat Sci, 2018, 25(1): 96-100. doi: 10.1002/jhbp.519
[3] 陈修宁, 刘占峰. 合并黄疸的急性胆囊炎急诊行腹腔镜胆囊切除术安全性分析[J]. 临床急诊杂志, 2020, 21(12): 978-981. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202012010.htm
[4] 闫加艳, 赵越, 陈炜. 国际《胆囊切除术中预防胆管损伤多协会共识和实践指南(2020)》解读[J]. 中国实用外科杂志, 2020, 40(12): 1391-1395, 1400. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGWK202012014.htm
[5] Nassar A, Hodson J, Ng HJ, et al. Predicting the difficult laparoscopic cholecystectomy: development and validation of a pre-operative risk score using an objective operative difficulty grading system[J]. Surg Endosc, 2020, 34(10): 4549-4561. doi: 10.1007/s00464-019-07244-5
[6] 马宏喆, 姚旭, 张晓博, 等. PTGD术后二期腹腔镜胆囊切除与急诊腹腔镜胆囊切除术的对照研究[J]. 临床急诊杂志, 2020, 21(1): 34-37. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202001004.htm
[7] Di Buono G, Romano G, Galia M, et al. Difficult laparoscopic cholecystectomy and preoperative predictive factors[J]. Sci Rep, 2021, 11(1): 2559. doi: 10.1038/s41598-021-81938-6
[8] Stanisic V, Milicevic M, Kocev N, et al. A prospective cohort study for prediction of difficult laparoscopic cholecystectomy[J]. Ann Med Surg(Lond), 2020, 60: 728-733. doi: 10.1016/j.amsu.2020.11.082
[9] Philip Rothman J, Burcharth J, Pommergaard HC, et al. Preoperative Risk Factors for Conversion of Laparoscopic Cholecystectomy to Open Surgery-A Systematic Review and Meta-Analysis of Observational Studies[J]. Dig Surg, 2016, 33(5): 414-423. doi: 10.1159/000445505
[10] Gregory GC, Kuzman M, Sivaraj J, et al. C-reactive Protein is an Independent Predictor of Difficult Emergency Cholecystectomy[J]. Cureus, 2019, 11(4): e4573.
[11] Terho PM, Leppäniemi AK, Mentula PJ. Laparoscopic cholecystectomy for acute calculous cholecystitis: a retrospective study assessing risk factors for conversion and complications[J]. World J Emerg Surg, 2016, 11: 54. doi: 10.1186/s13017-016-0111-4
[12] Bouassida M, Zribi S, Krimi B, et al. C-reactive Protein Is the Best Biomarker to Predict Advanced Acute Cholecystitis and Conversion to Open Surgery. A Prospective Cohort Study of 556 Cases[J]. J Gastrointest Surg, 2020, 24(12): 2766-2772. doi: 10.1007/s11605-019-04459-8
[13] Gomes CA, Soares C, Di Saverio S, et al. Gangrenous cholecystitis in male patients: A study of prevalence and predictive risk factors[J]. Ann Hepatobiliary Pancreat Surg, 2019, 23(1): 34-40. doi: 10.14701/ahbps.2019.23.1.34
[14] Nogoy DM, Padmanaban V, Balazero LL, et al. Predictors of Difficult Laparoscopic Cholecystectomy on Humanitarian Missions to Peru Difficult Laparoscopic Cholecystectomy in Surgical Missions[J]. J Surg Res, 2021, 267: 102-108. doi: 10.1016/j.jss.2021.04.020
[15] 赵云, 张光亚, 杨成林, 等. 糖尿病患者经PTGD后不同时机行腹腔镜胆囊切除的临床研究[J]. 临床急诊杂志, 2021, 22(6): 425-429. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202106014.htm
[16] Ashfaq A, Ahmadieh K, Shah AA, et al. The difficult gall bladder: Outcomes following laparoscopic cholecystectomy and the need for open conversion[J]. Am J Surg, 2016, 212(6): 1261-1264. doi: 10.1016/j.amjsurg.2016.09.024
[17] Janjic G, Simatovic M, Skrbic V, et al. Early vs. Delayed Laparoscopic Cholecystectomy for Acute Cholecystitis-Single Center Experience[J]. Med Arch, 2020, 74(1): 34-38. doi: 10.5455/medarh.2020.74.34-37
[18] Siada S, Jeffcoach D, Dirks RC, et al. A predictive grading scale for acute cholecystitis[J]. Trauma Surg Acute Care Open, 2019, 4(1): e000324. doi: 10.1136/tsaco-2019-000324
[19] Siddiqui MA, Rizvi S, Sartaj S, et al. A Standardized Ultrasound Scoring System for Preoperative Prediction of Difficult Laparoscopic Cholecystectomy[J]. J Med Ultrasound, 2017, 25(4): 227-231. doi: 10.1016/j.jmu.2017.09.001
[20] Izquierdo YE, Díaz Díaz NE, Muñoz N, et al. Preoperative factors associated with technical difficulties of laparoscopic cholecystectomy in acute cholecystitis[J]. Radiologia(Engl Ed), 2018, 60(1): 57-63.
[21] Jarrar MS, Fourati A, Fadhl H, et al. Risk factors of conversion in laparoscopic cholecystectomies for lithiasic acute cholecystitis. Results of a monocentric study and review of the literature[J]. Tunis Med, 2019, 97(2): 344-351.
-




 下载:
下载:
