Value of qSOFA score in predicting the severity of acute upper gastrointestinal bleeding
-
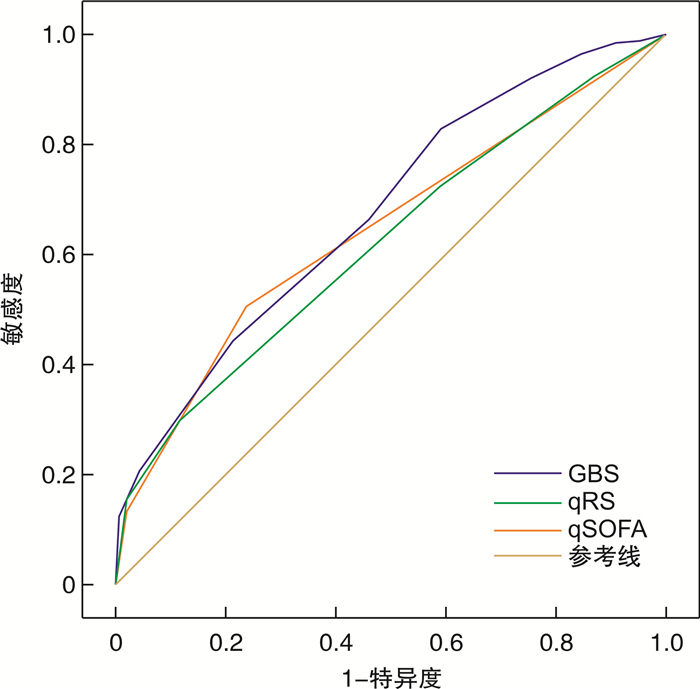
摘要: 目的 评估快速序贯器官衰竭(qSOFA)评分对急性上消化道出血病情严重程度的预测价值,并与Glasgow Blatchford评分(GBS)和内镜检查前的Rockall评分(pRS)的预测价值进行比较。方法 回顾性选取河北大学附属医院急诊科收治的917例急性上消化道出血患者,收集所有患者的临床资料,将需要进行输血治疗、再出血、重症监护及入院28 d内死亡定义为不良结局,表示患者病情严重,并据此分为无不良结局组(409例)和不良结局组(508例)。采用受试者工作特征(ROC)曲线分析GBS、pRS和qSOFA评分对急性上消化道出血患者不良结局的预测价值,并计算敏感度、特异度及截断值等参数。结果 2组患者的年龄、性别、呼吸频率、是否伴黑便、呕吐咖啡样物等指标比较,差异无统计学意义(P>0.05);收缩压、心率、血尿素氮、血红蛋白、伴呕血、晕厥、意识状态改变及合并症等指标比较,差异有统计学意义(P< 0.05)。GBS、pRS和qSOFA评分预测急性上消化道出血不良结局的ROC曲线下面积分别为0.681、0.626和0.648,差异有统计学意义(P< 0.05)。结论 GBS、pRS和qSOFA评分均能预测急性上消化道出血的病情严重程度,而qSOFA评分更简单方便,可以用来评估急性上消化道出血的病情严重程度。
-
关键词:
- Glasgow Blatchford评分 /
- pre-endoscopic Rockall评分 /
- 快速序贯器官衰竭评分 /
- 急性上消化道出血 /
- 预测
Abstract: Objective To evaluate the predictive value of quick sequential organ failure assessment (qSOFA) score on the severity of acute upper gastrointestinal bleeding, and to compare with the predictive value of Glasgow-Blatchford score (GBS) and pre-endoscopic Rockall score (pRS).Methods A retrospective study was conducted on 917 patients with acute upper gastrointestinal bleeding in the Emergency Department of the Affiliated Hospital of Hebei University, and clinical data were collected. Patients who underwent blood transfusion treatment, rebleeding, intensive care and death within 28 days of admission were included in the adverse outcome group, and the remaining patients were included in the group without adverse outcomes, and the predictive value of GBS, pRS and qSOFA score on adverse outcomes was analyzed and compared. The predictable value of GBS, pRS and qSOFA score for adverse outcomes in patients with acute upper gastrointestinal bleeding was analyzed using the receiver operator characteristic (ROC) curve, and the sensitivity, specificity and truncation values were calculated.Results There was no statistical significance(P>0.05) in the two groups of patients in comparing the indicators of age, sex, respiratory rate, whether they were accompanied by melaena and vomiting of coffee ground-like content; and the systolic blood pressure, heart rate, blood urea nitrogen, hemoglobin, concomitant hematemesis, syncope, altered state of consciousness and comorbidities were compared, and the differences were statistically significant(P< 0.05). The area under the ROC curve predicting the adverse outcome of acute upper gastrointestinal bleeding was 0.681, 0.626 and 0.648, respectively, and the difference was statistically significant(P< 0.05).Conclusion GBS, pRS and qSOFA score can predict the severity of acute upper gastrointestinal bleeding, while qSOFA score is simpler and more convenient and can be used to assess the severity of acute upper gastrointestinal bleeding. -

-
表 1 GBS、pRS和qSOFA评分的标准
评分项目 得分 GBS 血尿素氮/(mg·dL-1) ≥6.5~<8.0 2 ≥8.0~<10.0 3 ≥10.0~<25.0 4 ≥25.0 6 血红蛋白(男)/(g·L-1) ≥120~<130 1 ≥100~<120 3 <100 6 血红蛋白(女)/(g·L-1) ≥100~<120 1 <100 6 收缩压/mmHg ≥100~≤109 1 ≥90~<100 2 <90 3 其他要素 心率≥100次/min 1 伴黑便 1 伴晕厥 2 肝脏疾病或心衰 2 pRS 年龄/岁 <60 0 ≥60~<80 1 ≥80 2 休克表现 心率>100次/min 1 收缩压<100 mmHg 2 合并症 冠心病、慢性心衰、肾衰、肝功能不全 2 转移性恶性肿瘤 3 qSOFA评分 收缩压≤100 mmHg 1 呼吸频率≥22次/min 1 意识状态改变(GCS评分≤14) 1 注:1 mmHg=0.133 kPa;GCS评分为格拉斯哥昏迷评分,分为睁眼反应、言语反应及运动反应3项评分内容。 表 2 无不良结局组与不良结局组急性上消化道出血患者临床数据比较
M(Q1,Q3),例(%) 项目 总体(n=917) 无不良结局组(n=409) 不良结局组(n=508) P 年龄/岁 63(54,72) 63(54,72) 63(53,71) 0.792 男性 609(66.4) 262(64.1) 347(68.3) 0.182 收缩压/mmHg 122(105,143) 133(114,152) 115(97,134) < 0.05 心率/(次·min-1) 92(80,105) 89(79,102) 94(81,109) < 0.001 呼吸频率/(次·min-1) 20(19,20) 20(19,20) 20(19,21) 0.343 血尿素氮/(mmol·L-1) 9.65(6.40,14.73) 8.70(6.00,13.40) 10.20(7.00,16.10) < 0.001 血红蛋白/(g·L-1) 82(62,107) 92(73,119) 72(56,97) < 0.001 黑便 610(66.5) 273(66.7) 337(66.3) 0.944 呕血 528(57.6) 209(51.1) 319(62.8) < 0.001 呕吐咖啡样物 38(4.1) 21(5.1) 17(3.3) 0.186 晕厥 34(3.7) 9(2.2) 25(4.9) 0.035 意识状态改变 92(10.00) 14(3.40) 78(15.40) < 0.001 合并症a) 448(40.1) 175(42.8) 273(53.7) < 0.05 注:a)合并症包括冠心病、慢性心衰、肾衰及肝功能不全。 表 3 GBS、pRS及qSOFA评分预测不良结局的价值
项目 截断值 约登指数 敏感度/% 特异度/% AUC 阳性似然比/% 阴性似然比/% GBS >7 0.239 83.07 40.83 0.681 63.6 66.0 pRS >3 0.182 29.72 88.51 0.626 76.3 50.3 qSOFA评分 >0 0.273 50.98 76.28 0.648 72.8 55.6 表 4 GBS、pRS和qSOFA评分对不同不良结局指标的预测效能
项目 敏感度/% 特异度/% AUC 95%CI P 输血治疗 GBS 71.79 63.20 0.726 0.696~0.754 < 0.001 pRS 34.07 83.70 0.620 0.587~0.651 < 0.001 qSOFA评分 54.95 68.01 0.627 0.594~0.658 < 0.001 再出血 GBS 44.31 72.21 0.612 0.580~0.644 < 0.001 pRS 21.86 98.28 0.619 0.587~0.651 < 0.001 qSOFA评分 51.50 68.61 0.615 0.582~0.646 < 0.001 重症监护 GBS 68.66 54.47 0.645 0.613~0.676 < 0.001 pRS 85.07 33.53 0.643 0.611~0.674 < 0.001 qSOFA评分 67.16 63.53 0.677 0.645~0.707 < 0.001 28 d内死亡 GBS 61.90 77.34 0.731 0.701~0.759 < 0.001 pRS 61.90 79.35 0.772 0.744~0.799 < 0.001 qSOFA评分 90.48 62.50 0.832 0.806~0.855 < 0.001 -
[1] Tang Y, Shen J, Zhang F, et al. Scoring systems used to predict mortality in patients with acute upper gastrointestinal bleeding in the ED[J]. Am J Emerg Med, 2018, 36(1): 27-32. doi: 10.1016/j.ajem.2017.06.053
[2] Li Y, Song Y. Diagnostic Value of Serum Gastrin and Epidermal Growth Factor to the Gastric Ulcer Complicated with Upper Gastrointestinal Hemorrhage[J]. J Coll Physicians Surg Pak, 2020, 30(12): 1269-1272. doi: 10.29271/jcpsp.2020.12.1269
[3] 王立军. 急性上消化道出血的诊断与治疗新进展[J]. 中国中西医结合急救杂志, 2021, 28(1): 125-127.
[4] 涂霁韬, 薛思军. 奥美拉唑联合卡络磺钠治疗上消化道出血的疗效及安全性分析[J]. 中国中西医结合消化杂志, 2020, 28(11): 881-884. doi: 10.3969/j.issn.1671-038X.2020.11.13
[5] Taslidere B, Sonmez E, Özcan AB, et al. Comparison of the quick SOFA score with Glasgow-Blatchford and Rockall scores in predicting severity in patients with upper gastrointestinal bleeding[J]. Am J Emerg Med, 2021, 45: 29-36. doi: 10.1016/j.ajem.2021.02.016
[6] 中国医师协会急诊医师分会, 中华医学会急诊医学分会, 全军急救医学专业委员会, 等. 急性上消化道出血急诊诊治流程专家共识(2020版)[J]. 中华急诊医学杂志, 2021, 30(1): 15-24. doi: 10.3760/cma.j.issn.1671-0282.2021.01.006
[7] Liu S, Zhang X, Walline JH, et al. Comparing the Performance of the ABC, AIMS65, GBS, and pRS Scores in Predicting 90-day Mortality Or Rebleeding Among Emergency Department Patients with Acute Upper Gastrointestinal Bleeding: A Prospective Multicenter Study[J]. J Transl Int Med, 2021, 9(2): 114-122. doi: 10.2478/jtim-2021-0026
[8] Umemura Y, Ogura H, Gando S, et al. Prognostic Accuracy of Quick SOFA is different according to the severity of illness in infectious patients[J]. J Infect Chemother, 2019, 25(12): 943-949. doi: 10.1016/j.jiac.2019.05.010
[9] Usul E, Korkut S, Kayipmaz AE, et al. The role of the quick sequential organ failure assessment score(qSOFA)and modified early warning score(MEWS)in the pre-hospitalization prediction of sepsis prognosis[J]. Am J Emerg Med, 2021, 41: 158-162. doi: 10.1016/j.ajem.2020.09.049
[10] 赵尚飞, 黄妮, 宋明全. AIMS65与Blatchford评分评估上消化道出血的比较研究[J]. 临床急诊杂志, 2021, 22(2): 92-97. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202102004.htm
[11] Tokioka F, Okamoto H, Yamazaki A, et al. The prognostic performance of qSOFA for community-acquired pneumonia[J]. J Intensive Care, 2018, 6: 46. doi: 10.1186/s40560-018-0307-7
[12] Cannon JW. Hemorrhagic Shock[J]. N Engl J Med, 2018, 378(4): 370-379. doi: 10.1056/NEJMra1705649
[13] Standl T, Annecke T, Cascorbi I, et al. The Nomenclature, Definition and Distinction of Types of Shock[J]. Dtsch Arztebl Int, 2018, 115(45): 757-768.
[14] 张健峰, 顾晓蕾, 李斌, 等. 血乳酸联合qSOFA评分对早期筛选诊断脓毒症患者的价值[J]. 临床急诊杂志, 2021, 22(5): 344-347.
-




 下载:
下载: